![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
166 Cards in this Set
- Front
- Back
|
What fluid/non-fluid compartments can the total body weight be divided into (what percentages)? |
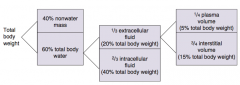
- 40% non-water mass
- 60% total body water |
|
|
What fluid compartments can the total body water be divided into? What percent of total body weight?
|
- 1/3 extracellular fluid (20% total body weight)
- 2/3 intracellular fluid (40% total body weight) |
|
|
What fluid compartments can the extracellular fluid be divided into? What percent of total body weight?
|
- 1/4 plasma volume (5% total body weight)
- 3/4 interstitial volume (15% total body weight) |
|
|
What is the "rule" to remember the % of body weight of the different fluid compartments?
|
60:40:20 rule:
- 60% total body water - 40% ICF - 20% ECF |
|
|
How do you measure the plasma volume?
|
Radio-labeled albumin
|
|
|
How do you measure the extracellular volume?
|
Inulin
|
|
|
What is the normal serum osmolarity?
|
290 mOsm/L
|
|
|
What is the glomerular filtration barrier composed of? What does each layer restrict?
|
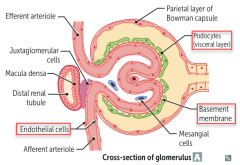
- Fenestrated capillary endothelium (size barrier)
- Fused basement membrane with heparan sulfate (negative charge barrier) - Epithelial layer consisting of podocyte foot processes |
|
|
What happens to the glomerular filtration barrier in nephrotic syndrome? Consequences?
|
Charge barrier (fused basement membrane with heparan sulfate) is lost in nephrotic syndrome, results in:
- Albuminuria - Hypoproteinemia - Generalized edema - Hyperlipidemia |
|
|
How do you calculate renal clearance?
|
Volume of plasma from which the substance is completely cleared per unit time
Cx = (Ux * V) / Px Cx = Clearance of X (mL/min) Ux = Urine concentration of X (mg/mL) Px = Plasma concentration of X (mg/mL) V = urine flow rate (mL/min) |
|
|
What does it tell you if the clearance of a substance is less than the GFR?
|
Net tubular reabsorption of X
|
|
|
What does it tell you if the clearance of a substance is greater than the GFR?
|
Net tubular secretion of X
|
|
|
What does it tell you if the clearance of a substance is equal to the GFR?
|
No net secretion or reabsorption
|
|
|
What can be used to calculate the GFR? Why?
|
Inulin clearance because it is freely filtered and is neither reabsorbed nor secreted (C-inulin = GFR)
GFR = (U-inulin * V) / P-inulin U-inulin = Urine concentration of inulin (mg/mL) P-inulin = Plasma concentration of inulin (mg/mL) V = urine flow rate (mL/min) |
|
|
How can you calculate GFR based on the pressures in the glomerulus and Bowman's capsule?
|
GFR = Kf [ (P-gc - P-bs) - (π-gc - π-bs) ]
P = hydrostatic pressure π = oncotic pressure gc = glomerular capillary bs = bowman's space π-bs usually equals zero (protein shouldn't be in bowman's space) |
|
|
What is a normal GFR?
|
~100 ml/min
|
|
|
Clearance of what can estimate GFR?
|
Creatinine clearance is an approximate measure of GFR; slightly overestimates GFR because creatinine is moderately secreted by the renal tubules
|
|
|
What is the staging of chronic kidney diseases based on?
|
Incremental reductions in GFR
|
|
|
How do you estimate the Effective Renal Plasma Flow (ERPF)?
|
Estimated using para-aminohippuric acid (PAH) clearance because it is both filtered and actively secreted in the proximal tubule; nearly all PAH entering the kidney is excreted
ERPF = (U-pah * V) / P-pah Underestimates the true renal plasma flow (RPF) by ~10% |
|
|
How do you determine the renal blood flow?
|
RBF = RPF / (1 - Hct)
RPF is estimated by ERPF = (U-pah * V) / P-pah |
|
|
What are the characteristics of para-aminohippuric acid (PAH) in the kidney?
|
- Both filtered and actively secreted in proximal tubule
- Nearly all PAH entering the kidney is excreted |
|
|
How do you calculate the filtration fraction? What is normal?
|
FF = GFR / RPF = normally 20%
- GFR is estimated by calculating clearance of inulin - RPF is estimated by calculating clearance of PAH Remember: Cx = (Ux * V) / Px |
|
|
How do you calculate the filtered load?
|
Filtered load (mg/min) = GFR (ml/min) * plasma concentration (mg/ml)
|
|
|
How do NSAIDs affect the filtration at the glomerulus?
|
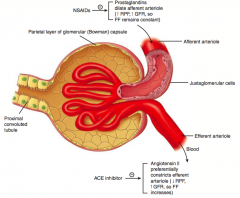
NSAIDs inhibit prostaglandins, preventing dilation of the afferent arteriole
- ↓ RPF, ↓ GFR, so Filtration Fraction remains constant (remember FF = GFR/RPF) |
|
|
How do prostaglandins affect the filtration at the glomerulus?
|
Prostaglandins dilate the afferent arteriole
- ↑ RPF, ↑ GFR, so Filtration Fraction remains constant (remember FF = GFR/RPF) |
|
|
How do ACE-inhibitors affect the filtration at the glomerulus?
|
ACE-I inhibit AngII, preventing constriction of the efferent arteriole
- ↑ RPF, ↓ GFR, so FF decreases (remember FF = GFR/RPF) |
|
|
How does Angiotensin II affect the filtration at the glomerulus?
|
AngII preferentially constricts the efferent arteriole
- ↓ RPF, ↑ GFR, so FF increases (remember FF = GFR/RPF) |
|
|
How does afferent arteriole constriction affect RPF, GFR, and FF (GFR/RPF)?
|
- ↓ RPF
- ↓ GFR - = FF |
|
|
How does efferent arteriole constriction affect RPF, GFR, and FF (GFR/RPF)?
|
- ↓ RPF
- ↑ GFR - ↑ FF |
|
|
How does ↑ plasma protein concentration affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↓ GFR - ↓ FF |
|
|
How does ↓ plasma protein concentration affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↑ GFR - ↑ FF |
|
|
How does constriction of the ureter affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↓ GFR - ↓ FF |
|
|
How do you calculate the filtered load?
|
Filtered load = GFR * Px
Px = plasma concentration of X (mg/ml) |
|
|
How do you calculate the excretion rate?
|
Excretion rate = V * Ux
V = urine flow rate (ml/min) Ux = urine concentration of X (mg/ml) |
|
|
How do you calculate the reabsorption rate?
|
Reabsorption = Filtered load - Excretion rate
Filtered load = GFR * Px Excretion rate = V * Ux |
|
|
How do you calculate the secretion rate?
|
Secretion = Excretion rate - Filtered load
Filtered load = GFR * Px Excretion rate = V * Ux |
|
|
What are the characteristics of glucose clearance in the kidney?
|
- Glucose at a normal plasma level is completely reabsorbed in the proximal tubule by Na+/glucose co-transport
- At plasma glucose of ~200 mg/dL, glucosuria begins (threshold) - At plasma glucose of ~375 mg/dL, all transporters are fully saturated (Tm) |
|
|
At what plasma glucose concentrations does all glucose get reabsorbed in the proximal tubule?
|
Up to ~200 mg/dL
- Above 200 mg/dL, glucosuria begins (threshold) |
|
|
At what plasma glucose concentrations are all Na+/glucose co-transporters fully saturated (Tm)?
|
At ~375 mg/dL
|
|
|
What happens to glucose and amino acid reabsorption during pregnancy?
|
Normal pregnancy ↓ reabsorption of glucose and amino acids in proximal tubule → glucosuria and aminoaciduria
|
|
|
How are amino acids normally treated in the kidney?
|
Normally all amino acids are reabsorbed by Na+ dependent transporters in the proximal tubule
|
|
|
What disorder causes a deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes? Implications?
|
Hartnup Disease:
- Leads to neutral aminoaciduria and ↓ absorption from gut - Results in pellagra-like symptoms; treat with high-protein diet and nicotinic acid |
|
|
What should you think of if you have a patient with a neutral aminoaciduria and decreased absorption from the gut with pellagra-like symptoms (dermatitis, diarrhea, and mental disturbance)? Cause?
|
Hartnup Disease
- Autosomal recessive deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes |
|
|
What are the characteristics of Hartnup Disease? Cause / Symptoms / Treatment?
|
- Autosomal recessive disorder, caused by deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes
- Leads to neutral aminoaciduria and ↓ absorption from gut - Results in pellagra-like symptoms (dermatitis, diarrhea, and mental disturbance) - Treat with high-protein diet and nicotinic acid |
|
|
What is reabsorbed and secreted in the proximal convoluted tubule?
|
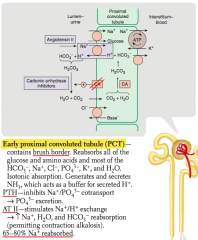
Reabsorbed:
- All glucose and amino acids - Most HCO3-, Na+, Cl-, PO4(3-), K+, H2O Secreted: - NH3 (buffers secreted H+) |
|
|
Which hormones act on the early proximal convoluted tubule?
|
- PTH
- AngII |
|
|
What is the action of PTH on the early proximal convoluted tubule?
|
Inhibits Na+ / PO4(3-) co-transport → PO4(3-) excretion
|
|
|
What is the action of Angiotensin II on the early proximal convoluted tubule?
|
- Stimulates Na+/H+ exchange → ↑ Na+, H2O, and HCO3- reabsorption
- Permits contraction alkalosis |
|
|
What percent of Na+ is reabsorbed in the early proximal convoluted tubule?
|
65-80% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the thin descending loop of Henle?
|
- Passive reabsorption of H2O via medullary hypertonicity
- Impermeable to Na+ |
|
|
What happens to urine in the thin descending loop of Henle?
|
- Concentrates urine
- Makes urine hypertonic |
|
|
What percent of Na+ is reabsorbed in the thin descending loop of Henle?
|
None - impermeable to Na+
|
|
|
What is reabsorbed and secreted in the thick ascending loop of Henle?
|

Reabsorbs:
- Active reabsorption of Na+, K+, and Cl- - Indirectly induces paracellular reabsorption of Mg2+ and Ca2+ (through + lumen potential generated by K+ backleak) Impermeable to H2O |
|
|
What happens to urine in the thick ascending loop of Henle?
|

- Impermeable to H2O but reabsorbing Na+
- This makes urine less concentrated as it ascends |
|
|
What percent of Na+ is reabsorbed in the thick ascending loop of Henle?
|

10-20% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the early distal convoluted tubule?
|
- Actively reabsorbs Na+ and Cl-
- PTH stimulates Ca2+/Na+ exchange → Ca2+ reabsorption |
|
|
Which hormones act on the distal convoluted tubule? Action?
|
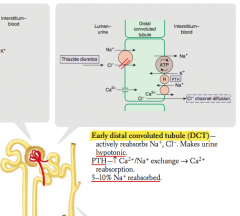
PTH - stimulates Ca2+/Na+ exchange → Ca2+ reabsorption
|
|
|
What percent of Na+ is reabsorbed in the distal convoluted tubule?
|
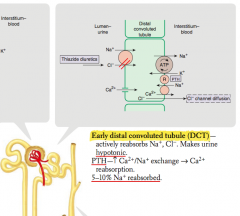
5-10% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the collecting tubule?
|

Reabsorbs Na+ in exchange for secreting K+ and H+
|
|
|
Which hormones act on the collecting tubule? Action?
|

- Aldosterone: acts on mineralocorticoid receptor → insertion of Na+ channel on luminal side
- ADH: acts at V2 receptor → insertion of aquaporin H2O channels on luminal side |
|
|
What percent of Na+ is reabsorbed in the collecting tubule
|

3-5% Na+ reabsorbed
|
|
|
In which segments of the nephron is sodium reabsorbed? What percentages?
|
- Proximal convoluted tubule: 65-80%
- Thin descending loop of Henle: none - Thick ascending loop of Henle: 10-20% - Distal convoluted tubule: 5-10% - Collecting tubule: 3-5% |
|
|
What are the types of renal tubular defects?
|
"The kidneys put out FABulous Glittering Liquid"
- Fanconi syndrome = 1st defect (PCT) - Bartter syndrome = 2nd defect (thick ascending loop of Henle) - Gitelman syndrome = 3rd defect (DCT) - Liddle syndrome = 4th defect (collecting tubule) |
|
|
Which renal tubular defect affects the Proximal Convoluted Tubule? What does it cause?
|
Fanconi Syndrome
- ↑ excretion of nearly all AAs, glucose, HCO3-, and PO4(3-) - May cause metabolic acidosis (proximal renal tubular acidosis) |
|
|
What causes Fanconi Syndrome? Where is the defect?
|
- Causes: hereditary defects (eg, Wilson disease), ischemia, and nephrotoxins/drugs
- Reabsorptive defect in the proximal convoluted tubule |
|
|
Which renal tubular defect affects the Thick Ascending Loop of Henle? What does it cause?
|
Bartter Syndrome
- Affects Na+/K+/2Cl- co-transporter - Causes hypokalemia, metabolic alkalosis and hypercalciuria |
|
|
What causes Bartter Syndrome? Where is the defect?
|
- Causes: autosomal recessive defect of Na+/K+/2Cl- co-transporter
- Reabsorptive defect in thick ascending loop of Henle |
|
|
Which renal tubular defect affects the Distal Convoluted Tubule? What does it cause?
|
Gitelman Syndrome
- Hypokalemia - Metabolic alkalosis - NO hypercalciuria |
|
|
What causes Gitelman Syndrome? Where is the defect?
|
- Cause: autosomal recessive defect of NaCl reabsorption
- Reabsorptive defect in distal convoluted tubule |
|
|
Which renal tubular defect affects the Distal and Collecting Tubules? What does it cause?
|
Liddle Syndrome
- Hypertension - Hypokalemia - Metabolic alkalosis - ↓ Aldosterone |
|
|
What causes Liddle Syndrome? Where is the defect?
|
- Cause: Autosomal Dominant defect leading to increased activity of epithelial Na+ channel
- Distal and collecting tubules |
|
|
How do you treat Liddle Syndrome?
|
Amiloride
|
|
|
What syndrome causes ↑ excretion of nearly all AAs, glucose, HCO3-, and PO4(3-), which may lead to a metabolic acidosis? What causes this?
|
Fanconi Syndrome
- Reabsorptive defect in proximal convoluted tubule - Causes: hereditary defects (eg, Wilson disease), ischemia, and nephrotoxins/drugs |
|
|
What syndrome causes hypokalemia and metabolic alkalosis with hypercalciuria? What causes this?
|
Bartter Syndrome
- Reabsorptive defect in thick ascending loop of Henle - Autosomal recessive, affects Na+/K+/2Cl- co-transporter |
|
|
What syndrome causes hypokalemia and metabolic alkalosis without hypercalciuria? What causes this?
|
Gitelman Syndrome
- Reabsorptive defect of NaCl in distal convoluted tubule - Autosomal recessive, less severe than Bartter syndrome |
|
|
What syndrome causes hypertension, hypokalemia, metabolic alkalosis, and ↓ aldosterone? What causes this?
|
Liddle Syndrome
- ↑ Na+ reabsorption in distal and collecting tubules (↑ activity of epithelial Na+ channel) - Autosomal dominant - Treat with Amiloride |
|
|
What is the meaning of the ratio of TF/P?
|
[Tubular Fluid] / [Plasma]
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is >1?
|
Solute is reabsorbed less quickly than water
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is =1?
|
Solute and water are reabsorbed at the same rate
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is <1?
|
Solute is reabsorbed more quickly than water
|
|
|
What happens to the tubular inulin concentration as it progresses along the nephron? How?
|
Inulin concentration increases in the tubule (but not in amount) along the proximal tubule as a result of water reabsorption
|
|
|
Which substance has net secretion in the proximal tubule?
|
PAH
|
|
|
Which substance has net reabsorption in the proximal tubule?
|
- Urea
- Na+, K+, Cl- - Pi - HCO3- - Glucose and amino acids |
|
|
Which substance has no net secretion or reabsorption in the proximal tubule?
|
Creatinine and Inulin
|
|
|
How does the reabsorption of Cl- compare to Na+ in the proximal tubule?
|
Cl- reabsorption occurs at a slower rate than Na+ in early proximal tubule and then matches the rate of Na+ reabsorption more distally; thus, its relative concentration increases before it plateaus
|
|
|
What is the action of Renin? Source?
|
Stimulates conversion of Angiotensinogen (from liver) to Angiotensin I
- Renin is from the kidney |
|
|
What is the source of Renin? What stimulates it?
|
Renin is from the kidney, release stimulated by:
- ↓ BP (Juxtaglomerular cells) - ↓ Na+ delivery to macula densa cells - ↑ Sympathetic tone (β1-receptors) |
|
|
What is the action of ACE? Source?
|
- ACE converts Ang I to Ang II
- ACE also stimulates Bradykinin breakdown - ACE is from the lungs and the kidneys |
|
|
What is the action of Angiotensin II?
|
- Vasoconstriction (via AT I receptors) → ↑ BP
- Constricts efferent arteriole of glomerulus → ↑ FF to preserve renal function (GFR) in low-volume states (when ↓ RBF) - Stimulates Aldosterone (adrenal gland) - Stimulates ADH (posterior pituitary) - ↑ Proximal tubule Na+/H+ activity → ↑ Na+, HCO3-, and H2O reabsorption (can permit contraction alkalosis) - Stimulates hypothalamus → thirst |
|
|
How does AngII increase the BP?
|
Acts at AT I receptors on vascular smooth muscle → Vasoconstriction → ↑ BP
|
|
|
How does AngII affect the filtration fraction (FF)?
|
Constricts efferent arteriole of glomerulus → ↑ FF to preserve renal function (GFR) in low-volume states (ie, when RBF ↓)
|
|
|
What is the effect of Aldosterone release? Source?
|
- ↑ Na+ channel and Na+/K+ pump insertion in principal cells
- Enhances K+ and H+ excretion (upregulates principal cell K+ channels and intercalated cell H+ ATPases) - Creates unfavorable Na+ gradient for Na+ and H2O reabsorption - From adrenal gland |
|
|
What is the effect of ADH release? Source?
|
- ↑ H2O channel insertion in principal cells, leading to H2O reabsorption
- From posterior pituitary |
|
|
What is the effect of Angiotensin II on the proximal tubule?
|
- ↑ Proximal tubule Na+/H+ activity
- Leads to Na+, HCO3-, and H2O reabsorption (can permit contraction alkalosis) |
|
|
Which hormone affects baroreceptor function, limiting the reflex bradycardia, which would normally accompany its pressor effects?
|
Angiotensin II
|
|
|
Which hormone is released from atria in response to increased volume, may act as a check on renin-angiotensin-aldosterone system, relaxing vascular smooth muscle via cGMP, causing ↑ GFR and ↓ renin?
|
ANP (Atrial Natriuretic Protein)
|
|
|
Which hormone is primarily responsible for regulating osmolarity and responds to low blood volume states?
|
ADH
|
|
|
Which hormone primarily regulates ECF Na+ content and volume, by responding to low blood volume states?
|
Aldosterone
|
|
|
What are the components of the juxtaglomerular apparatus?
|
- JG cells (modified smooth muscle of afferent arteriole)
- Macula Densa (NaCl sensor, part of the distal convoluted tubule) |
|
|
What is the function of the Juxtaglomerular cells?
|
Secrete renin in response to:
- ↓ Renal blood pressure - ↓ NaCl delivery to distal tubule - ↑ Sympathetic tone (β1) |
|
|
Which drugs can influence the juxtaglomerular apparatus?
|
β-blockers (specifically β1) can decrease BP by inhibiting β1 receptors of JGA, causing ↓ renin release
|
|
|
Which hormones are secreted by the kidney?
|
- Erythropoietin
- 1,25-(OH)2 Vitamin D - Renin - Prostaglandins |
|
|
What is the source and function of Erythropoietin?
|
Released by interstitial cells in the peritubular capillary bed in response to hypoxia
|
|
|
What is the source and function of 1,25-(OH)2 Vitamin D?
|
- Proximal tubule cells convert 25-OH vitamin D to 1,25-(OH)2 Vitamin D (Active form)
- Enzyme: 1α-Hydroxylase (stimulated by PTH) |
|
|
What is the source and function of Renin?
|
Secreted by JG cells in response to ↓ renal arterial pressure and ↑ renal sympathetic discharge (β1 effect)
|
|
|
What is the source and function of prostaglandins?
|
- Paracrine secretion vasodilates the afferent arterioles to ↑ RBF
- From kidney |
|
|
What is the effect of NSAIDs on the kidney?
|
- NSAIDs block renal-protective prostaglandin synthesis → constriction of the afferent arteriole and ↓ GFR
- This may result in acute renal failure |
|
|
Which hormones act on the kidney?
|
- Angiotensin II (ATII)
- Atrial Natriuretic Peptide (ANP) - Parathyroid Hormone (PTH) - Aldosterone - ADH (Vasopressin) |
|
|
What causes Angiotensin II (AT II) to be released and act on kidney? Function?
|
- Synthesized in response to ↓ BP
- Causes efferent arteriole constriction → ↑ GFR and ↑ FF - Compensatory Na+ reabsorption in proximal and distal nephron - Net effect: preservation of renal function in low-volume state (↑FF) with simultaneous Na+ reabsorption to maintain circulating volume |
|
|
What causes Parathyroid Hormone (PTH) to be released and act on kidney? Function?
|
- Secreted in response to ↓ plasma [Ca2+], ↑ plasma [PO4(3-)], or ↓ plasma 1,25-(OH)2 vitamin D
- Causes ↑ [Ca2+] reabsorption from DCT, ↓ [PO4(3-)] reabsorption (PCT), and ↑ 1,25-(OH)2 vitamin D production - Increases Ca2+ and PO4(3-) absorption from gut via vitamin D |
|
|
Where are Ca2+ and PO4(3-) reabsorbed in nephron in response to PTH?
|
- Ca2+ reabsorbed in DCT
- PO4(3-) reabsorbed in PCT |
|
|
What causes Atrial Natriuretic Peptide (ANP) to be released and act on kidney? Function?
|
- Secreted in response to ↑ atrial pressure
- Causes ↑ GFR and ↑ Na+ filtration with no compensatory Na+ reabsorption in distal nephron - Net effect: Na+ loss and volume loss |
|
|
What causes Aldosterone to be released and act on kidney? Function?
|
- Secreted in response to ↓ blood volume (via AT II) and ↑ plasma [K+]
- Causes ↑ Na+ reabsorption, ↑ K+ secretion, ↑ H+ secretion |
|
|
What causes ADH (Vasopressin) to be released and act on kidney? Function?
|
- Secreted in response to ↑ plasma osmolarity and ↓ blood volume
- Binds to receptors on principal cells, causing ↑ number of water channels and ↑ H2O reabsorption |
|
|
Which conditions/drugs cause K+ to shift out of cells (causing hyperkalemia)?
|
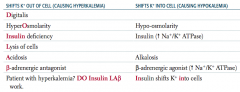
Patient with hyperkalemia? DO Insulin LAβ work
- Digitalis - HyperOsmolarity - INSULIN deficiency - Lysis of cells - Acidosis - β-adrenergic antagonist |
|
|
Which conditions/drugs cause K+ to shift into cells (causing hypokalemia)?
|
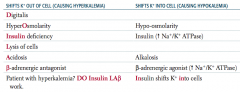
INsulin shifts K+ INto cells
- Hypoosmolarity - Insulin (↑ Na+ / K+ ATPase) - Alkalosis - β-adrenergic agonist (↑ Na+ / K+ ATPase) |
|
|
What electrolyte disturbance causes nausea, malaise, stupor, and coma?
|
Low serum Na+
|
|
|
What electrolyte disturbance causes irritability, stupor, or coma?
|
High serum Na+
|
|
|
What electrolyte disturbance causes U waves on ECG, flattened T waves, arrhythmias, and muscle weakness?
|
Low serum K+
|
|
|
What electrolyte disturbance causes wide QRS and peaked T waves on ECG, arrhythmias, and muscle weakness?
|
High serum K+
|
|
|
What electrolyte disturbance causes tetany, seizures, and QT prolongation?
|
Low serum Ca2+
|
|
|
What electrolyte disturbance causes stones (renal), bones (pain), groans (abdominal pain), psychiatric overtones (anxiety, altered mental status), but not necessarily calciuria?
|
High serum Ca2+
|
|
|
What electrolyte disturbance causes tetany and Torsades de Pointes?
|
Low serum Mg2+
|
|
|
What electrolyte disturbance causes ↓ DTRs, lethargy, bradycardia, hypotension, cardiac arrest, and hypocalcemia?
|
High serum Mg2+
|
|
|
What electrolyte disturbance causes bone loss and osteomalacia?
|
Low serum PO4(3-)
|
|
|
What electrolyte disturbance causes renal stones, metastatic calcifications, and hypocalcemia?
|
High serum PO4(3-)
|
|
|
What is the effect of low vs high serum concentration of Na+?
|
- Low: nausea, malaise, stupor, coma
- High: irritability, stupor, coma |
|
|
What is the effect of low vs high serum concentration of K+?
|
- Low: U waves on ECG, flattened T waves, arrhythmias, muscle weakness
- High: wide QRS and peaked T waves on ECG, arrhythmias, muscle weakness |
|
|
What is the effect of low vs high serum concentration of Ca2+?
|
- Low: tetany, seizures, QT prolongation
- High: stones (renal), bones (pain), groans (abdominal pain), psychiatric overtones (anxiety, altered mental status), but not necessarily calciuria |
|
|
What is the effect of low vs high serum concentration of Mg2+?
|
- Low: tetany and torsades de pointes
- High: ↓ DTRs (reflexes), lethargy, bradycardia, hypotension, cardiac arrest, hypocalcemia |
|
|
What is the effect of low vs high serum concentration of PO4(3-)?
|
- Low: bone loss, osteomalacia
- High: renal stones, metastatic calcifications, hypocalcemia |
|
|
What is the pH, PCO2, and [HCO3-] associated with metabolic acidosis? Compensatory response?
|
- ↓ pH
- ↓ PCO2 - ↓↓ [HCO3-] - Immediate hyperventilation ↓↓ = 1° distrubance ↓ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with metabolic alkalosis? Compensatory response?
|
- ↑ pH
- ↑ PCO2 - ↑↑ [HCO3-] - Immediate hypoventilation ↑↑ = 1° distrubance ↑ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with respiratory acidosis? Compensatory response?
|
- ↓ pH
- ↑↑ PCO2 - ↑ [HCO3-] - ↑ Renal [HCO3-] reabsorption (delayed) ↑↑ = 1° distrubance ↑ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with respiratory alkalosis? Compensatory response?
|
- ↑ pH
- ↓↓ PCO2 - ↓ [HCO3-] - ↓ Renal [HCO3-] reabsorption (delayed) ↓↓ = 1° distrubance ↓ = compensatory response |
|
|
What is the Henderson-Hasselbach equation in terms of [HCO3-] and PCO2?
|
pH = 6.1 + log [HCO3-] / 0.03 PCO2
|
|
|
How can you calculate the predicted respiratory compensation for a simple metabolic acidosis? What does it tell you?
|
Winters Formula
- If the measured PCO2 differs significantly from the predicted PCO2, then a mixed acid-base disorder is likely present PCO2 = 1.5 [HCO3-] + 8 +/- 2 |
|
|
If you suspect an acidosis or alkalosis, what do you check first?
|
Check arterial pH
- pH <7.4 = Acidemia - pH >7.4 = Alkalemia |
|
|
What do you test after you establish a patient has an acidemia (arterial pH <7.4)?
|
Check PCO2
- PCO2 >40 mmHg = Respiratory Acidosis - PCO2 <40 mmHg = Metabolic Acidosis with compensation (hyperventilation) |
|
|
What do you test after you establish a patient has an alkalemia (arterial pH >7.4)?
|
Check PCO2
- PCO2 <40 mmHg = Respiratory Alkalosis - PCO2 >40 mmHg = Metabolic Alkalosis with compensation (hypoventilation) |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 >40mmHg? What causes this?
|
Respiratory Acidosis, caused by hypoventilation, such as:
- Airway obstruction - Acute lung disease - Chronic lung disease - Opioids, sedatives - Weakening of respiratory muscles |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg? What should you check next?
|
Metabolic Acidosis with compensation (hyperventilation)
- Check for anion gap Anion Gap = Na+ - (Cl- + HCO3-) Normal: 8-12 mEq/L |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg and an ↑ anion gap? What are the potential causes?
|
Metabolic Acidosis with compensation (hyperventilation)
MUDPILES: - Methanol (formic acid) - Uremia - Diabetic Ketoacidosis - Propylene glycol - Iron tablets or INH - Lactic acidosis - Ethylene glycol (oxalic acid) - Salicylates (late) |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg and a normal anion gap (8-12 mEq/L)? What are the potential causes?
|
Metabolic Acidosis with compensation (hyperventilation)
HARD-ASS: - Hyperalimentation - Addison disease - Renal tubular acidosis - Diarrhea - Acetazolamide - Spironolactone - Saline infusion |
|
|
What is the diagnosis if a patient has pH >7.4 and PCO2 <40mmHg? What causes this?
|
Respiratory alkalosis, can be caused by:
Hyperventilation: - Hysteria - Hypoxemia (eg, high altitude) - Salicylates (early) - Tumor - Pulmonary embolism |
|
|
What is the diagnosis if a patient has pH >7.4 and PCO2 >40mmHg? What causes this?
|
Metabolic alkalosis with compensation (hypoventilation), caused by:
- Loop diuretics - Vomiting - Antacid use - Hyperaldosteronism |
|
|
What do these have in common? What would they cause?
- Airway obstruction - Acute lung disease - Chronic lung disease - Opioids, sedatives - Weakening of respiratory muscles |
Causes of hypoventilation → Respiratory Acidosis
|
|
|
What do these have in common? What would they cause?
- Methanol (formic acid) - Uremia - Diabetic Ketoacidosis - Propylene glycol - Iron tablets or INH - Lactic acidosis - Ethylene glycol (oxalic acid) - Salicylates (late) |
Metabolic Acidosis with compensation (hyperventilation) with ↑ Anion Gap
|
|
|
What do these have in common? What would they cause?
- Hyperalimentation - Addison disease - Renal tubular acidosis - Diarrhea - Acetazolamide - Spironolactone - Saline infusion |
Metabolic Acidosis with compensation (hyperventilation) with normal Anion Gap (8-12 mEq/L)
|
|
|
What do these have in common? What would they cause?
- Hysteria - Hypoxemia (eg, high altitude) - Salicylates (early) - Tumor - Pulmonary embolism |
Causes of hyperventilation → Respiratory Alkalosis
|
|
|
What do these have in common? What would they cause?
- Loop diuretics - Vomiting - Antacid use - Hyperaldosteronism |
Metabolic Alkalosis with compensation (hypoventilation)
|
|
|
When should you calculate the anion gap? How? What is normal?
|
When you have a metabolic acidosis (pH < 7.4 and PCO2 < 40 mmHg)
Anion Gap = Na+ - (Cl- + HCO3-) Normal = 8-12 mEq/L |
|
|
What kind of disorder causes a non-anion gap hyperchloremic metabolic acidosis?
|
Renal Tubular Acidosis
|
|
|
What are the types of Renal Tubular Acidosis?
|
- Type 1: distal, pH >5.5
- Type 2: proximal, pH <5.5 - Type 4: hyperkalemic, pH <5.5 |
|
|
Which type of Renal Tubular Acidosis is caused by a defect in the ability of the α intercalated cells to secrete H+? Implications?
|
Type 1 (distal, pH >5.5)
- New HCO3- is not generated → metabolic acidosis - Associated with hypokalemia, ↑ risk for calcium phosphate kidney stones (d/t ↑ urine pH and ↑ bone turnover) |
|
|
What can cause Type 1 Renal Tubular Acidosis (distal, pH >5.5)?
|
Defects in ability of α intercalated cells to secrete H+
- Amphotericin B toxicity - Analgesic nephropathy - Congenital anomalies (obstruction) of urinary tract |
|
|
Which type of Renal Tubular Acidosis is caused by a defect in the proximal tubule HCO3- reabsorption? Implications?
|
Type 2 (proximal, pH < 5.5)
- Leads to ↑ excretion of HCO3- in urine and subsequent metabolic acidosis - Urine is acidified by α intercalated cells in collecting tubule - Associated with hypokalemia and ↑ risk for hypophosphatemic rickets |
|
|
What can cause Type 2 Renal Tubular Acidosis (proximal, pH <5.5)?
|
Defects in proximal tubule HCO3- reabsorption:
- Fanconi syndrome (eg, Wilson disease) - Chemicals toxic to proximal tubule (eg, lead, aminoglycosides) - Carbonic anhydrase inhibitors - Multiple myeloma (light chains) |
|
|
Which type of Renal Tubular Acidosis is caused by hypoaldosteronism, aldosterone resistance, or K+ sparing diuretics? Implications?
|
- Results in hyperkalemia
- Impairs ammoniagenesis in proximal tubule → ↓ buffering capacity and ↓ H+ excretion into urine |
|
|
What can cause Type 4 Renal Tubular Acidosis (hyperkalemic, pH <5.5)?
|
- Hypoaldosteronism
- Aldosterone resistance - K+ sparing diuretics |
|
|
What are the characteristics of Type 1 Renal Tubular Acidosis?
|
Distal, pH>5.5
- Defect in ability of α intercalated cells to secrete H+ - New HCO3- is not generated → metabolic acidosis - Associated with hypokalemia, ↑ risk for calcium phosphate kidney stones (d/t ↑ urine pH and ↑ bone turnover) Causes: - Amphotericin B toxicity - Analgesic nephropathy - Congenital anomalies (obstruction) of urinary tract |
|
|
What are the characteristics of Type 2 Renal Tubular Acidosis?
|
Proximal, pH<5.5
- Defect in proximal tubule HCO3- reabsorption - ↑ Excretion of HCO3- in urine and subsequent metabolic acidosis - Urine acidified in α intercalated cells in collecting tubule - Associated with hypokalemia and ↑ risk for hypophosphatemic rickets Causes: - Fanconi syndrome (eg, Wilson disease) - Chemicals toxic to proximal tubule (eg, lead, aminoglycosides) - Carbonic anhydrase inhibitors - Multiple myeloma (light chains) |
|
|
What are the characteristics of Type 4 Renal Tubular Acidosis?
|
Hyperkalemic, pH<5.5
- Results in hyperkalemia, which impairs ammoniagenesis in proximal tubule - ↓ Buffering capacity and ↓ H+ excretion into urine Causes: - Hypoaldosteronism - Aldosterone resistance - K+ sparing diuretics |
|
|
Which type of Renal Tubular Acidosis is associated with hypokalemia and and increased risk for calcium phosphate kidney stones?
|
Type 1 (distal, pH >5.5)
|
|
|
Which type of Renal Tubular Acidosis is associated with hypokalemia and increased risk for hypophosphatemic rickets?
|
Type 2 (proximal, pH <5.5)
|
|
|
Which type of Renal Tubular Acidosis is associated with hyperkalemia?
|
Type 4 (hyperkalemic, pH <5.5)
|

