![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back

How often do horses urinate per day and in what volume? What is considered polyuria? |
Normal: 2-4 times per day. 10-30 ml/kg/day which is 5-15 litres Polyuria: >50 ml/kg per day >25 litres |
|

How much do horses drink per day normally? What may alter a horses water intake? Polydipsia? |
50 ml/kg/day. Temperature. Feeding salt. Water content of food. Polydipsia: is >100 ml/kg/day. |
|

Common causes of PUPD? |
Primary/psycogenic polydipsia--> stabled and bored. ECDz/PPID--> Aged, hirsute, lamitis, recurrent infections. Primary Renal disease--> Aged, weight loss, uraemia. |
|

Less common reasons for horses developing PUPD? |

Pyschogenic salt consumption--> bored in stable. Diabetes insipidus. Drug induced/iatrogenic like corticosteroids or alpha adrenergic. |
|
|
How can we differentiate PUPD from pollakiuria? |
Monitoring water consumption. |
|

In terms of signalment what are the predispositions to different PUPD conditions? |
Age: Younger horses pyschogenic/primary polydipsia. ECDz/PPID--> Older. No sex or breed predispositions. |
|

What type of PUPD is common in stabled horses? |
Pyschogenic |
|

If we have PUPD with weight loss what diseases would you be suspicious of ? |
Chronic renal failure. ECDz/ PPID. |
|

Diagnostic signs to look for when clinically examining a PUPD horse?
|
PUPD vs Pollakiuria. Hydration status. Weight loss? Any evidence of uraemia? Poor coat. Ventral oedema. Laminitis and hirsutism. |
|
|
What baseline tests should be run on a PUPD case? |
Urinalysis- SG, osmolarity, dipstick test, electrolytes and creatinine. Haematology and biochemistry- WBC, urea and creatinine, PCV, Protein levels, electrolytes. Glycaemic status. |
|
|
What are signs on haematology that may occur with kidney disease? |
Decreased RBCs. Anaemia of chronic disease or decreased production of erythropoeitin. Increased WBC due to chronic infections. |
|
|
What does increased urea and creatinine indicate in terms of urinary tract disease? |
>75% loss of total tubular function or dehydration. |
|
|
What may decreased protein reflect in terms of kidney disease? |
Glomerular mainly or tubular disease. |
|
|
What electrolyte parameters may indicate renal disease? |
Decreased sodium, chloride, potassium with acute or chronic renal failure. Calcium increase with chronic and decrease with acute. Phosphate decrease with chronic and increase with acute. |
|

If we have signs of renal disease what must we do in terms of further examination? |
Rectal examination--> evaluate kidneys and presence of pain. Ultrasonography--> Size and echogenicity of kidneys. Fractional excretion of electrolytes--> sodium. Renal biopsy..Risk of fatal haemorrhage. |
|
|
If we have no sign of renal disease or cushings ruled out what can we do? |
Water deprivation test. ADH stimulation test. |
|

What is the cause of PPID/ ECDz? |
Overproduction of proopiomelanocortin (POMC) peptides from the pars intermedia. This leads to a increase in ACTH coupled with potentiated effects of other POMC peptides on ACTH leading to dysregulated cortisol secretion. |
|
|
What is found at PMI with most ECDz/PPID horses? |
Masses of the pituatary. |
|

Clinical signs of ECD? |
Hirsutism, hypertrichosis, change to coat. Hyperhidrosis. Laminitis. Lethargy and poor demeanour. Fat redistribution . Predisposition to infetions. Weight loss. PUPD. Polphagia. Blindness. Seizures. |
|
|
Why do we get hair coat changes with ECD? |
Increased cortisol may lead to increased androgen production. Compression by growth on hypothalmic thermoregulatory centres. |
|
|
Why do we get hyperhidrosis with ECD? |
Effects of compression on hypothalmic thermoregulatory centres. MSH involved in temp reg. |
|
|
Why do we get laminitis, fat redistribution and predisposition to infection with ECD? |
Effects of glucocorticoids on metabolism and immunity. |
|

What is pathognomonic for equine cushings? |
Hypertrichosis is the summer. |
|
|
What resting hormones can we use to help us diagnose equine cushings? |
Basal glucose >5.5 mmol/l Basal insulin >36 iu/ml Basal cortisol >140nmol/l Basal ACTH over >27 pg/ml in ponies >50 pg/ml in horses. Basal MSH >91 pmol/l |
|
|
What dynamic tests can we use to help us diagnose a horse with cushings? |
ACTH stimulation test--> poor sensitivity. Dexamethasone suppression test overnight--> 50-100% specific and sensitive. TRH response test. Combine DST and TRH. |
|

What plays a role in the unreliability of diagnostic tests for equine cushings? |
Seasonality. Increased false positives in the Autumn. |
|

How can we conservatively manage a cushings horse? |
1) Good attention to feeding, dentistry, antihelmintic regimes and early detection of clinical abnormalities. 2) Clipping excess long haircoat. 3) Regular farriery and monitor for signs of laminitis. 4) Continued exercise in absence of acute or chronic orthopaedic disease. 5) Monitor weight. 6) Treat infections promptly. |
|
What medications can we use to treat ECD? |
Pergolide a dopamine agonist that inhibits release of ACTH. Cyproheptadine 5HT agonist inhibiting release of ACTH. Trilostane 3beta HSD inhibitor. |
|
|
Poor prognostic indicators in a ECD horse? |
Intractable laminitis. Weight loss. Secondary diabetes mellitus. Failure to respond to treatment. |
|
|
What are causes of urinary incontinence? |
Reflex/UMN bladder--> EHV-1, EPM Paralytic/LMN bladder--> Polyneuritis equi, EHV-1, trauma. Non neurogenic: Inflammatory/irritant e.g. cystitis, urolithiasis. Myogenic--> detrusor atony. Neoplasia. Mechanical--> breeding trauma, ectopic ureter. Hypo-oestrogenism. |
|
|
In terms of signalment what are findings with incontinence? |
Age:Foals congenital like ectopic ureter. Neoplasia older. Breed none. Sex: Fillies predisposed to ectopic ureters and cystitis, mares breeding trauma. |
|

History and clinical signs of a horse with urinary incontinence? |
Continual dribbling of urine. Moving/vocalising leading to urination due to increased abdominal pressure. Urine smell. Crystals and hair loss on perineum, sheath, hindlimbs. Ataxia, caudal neurological deficits--> LMN, tail tone poor, anus, sensation. |
|
|
Further investigations we can undertake in a incontinence case? |
Urinalysis. Vaginal exam. Ultrasound. Cystoscopy. Cystometry. |
|
|
How can we treat incontinence? |
Palliative care like drainage and flushing. Washing and then vaseline. Antibiotics. Some mares respond to antibiotics. A adrenergic blockers to decrease sphincter tone to allow urination with UMN. Bethanecol for detrusor function. |
|

Define uraemia? |
Clinical signs associated with increase nitrogenous compounds in bloodstream such as anorexia, weight loss, bedraggled hair coat. |
|
|
Define azotaemia? |
Abnormal increase in biochemical parameters associated with renal disease. Pre-renal: decreased renal perfusion due to dehydration. Renal: Acute/chronic renal failure. Post-renal azotaemia: Obstructive disorder. Uroperitoneum. |
|
|
When does renal failure occur in the horse? |
Loss of 75% of nephrons. |
|
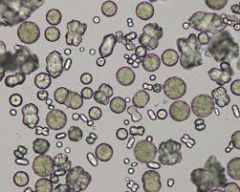
What crystal is common in horse urine and why? |
Calcium carbonate as excrete lots of calcium through their kidneys. |
|
|
Causes of ACUTE renal failure in horses? |
Acute tubular necrosis: Drugs (NSAIDs, aminoglycosides,polymixin B), heavy metals, pigments, acorns, vitamins D and K3. Vascular: vasomotor neuropathy: dehydration, shock, hypotension, adverse reaction. Acute glomeruloneuropathy--> immune mediated Acute interstital nephritis. Leptospirosis. |
|
|
DDX for chronic Chronic renal failure in horses? |
Glomerular disease. Chronic interstitial nephritis. End stage kidney disease. Amyloidosis. Neoplasia. |
|
|
Signalment findings with renal failure patients? |
Age: Older or very young due to congenital. Breed none. Sex: males predisposed to bladder rupture and females ectopic ureter. |
|
|
History and clinical exam findings with kidney failure? |
Depression. Anorexia. Dysuria that is isosthenuric. |
|
|
Normal USG of horse? Iso? Hypos? |
USG normally 1.020-1.050 Iso 1.008-1.014 Hypo <1.008 |
|
|
Normal dipstick findings on horse urine? |
pH- 7-9 Protein +1 Glucose none Ketones none. Hb/Mb none. Bilirubin None |
|
|
What tests would we run for a horse in kidney failure? |
Haematology (Anaemia) and biochemistry( Urea/creatinine, electrolytes. Urinalysis- Isosthenuria, increased urinary enzymes, haematuria, increase casts. |
|
|
Other tests we can run with a renal failure case? |
Ultrasound. Endoscopy. Fractional excretion of electrolytes. Measure GFR. Biopsy. |
|

How do we treat acute renal failure? |
1) Fluid therapy with regular monitoring of electrolyte status. Be careful not to overhydrate and for oedema formation. 2) Monitor urination. If oliguric after 24 hours address with furosemide, mannitol, dopamine. 3) Peritoneal dialysis. 4) Creatinine should decrease by at least 30% in 24 hours. 5) Slowly wean off fluids and supplement electrolytes short term. |
|
|
Approach to treating a chronic renal failure case? |
1) Fluids for 24-48 hours 2) Identify and treat abnormality. 3) Diet- correct electrolyte and acid/base abnormalities, small and frequent meals, avoid high calcium feeds like alfalfa, increase cards, anabolic steroids. 4) Blood/plasma transfusion for anaemia etc. 5) Erythropoeitin. |
|

DDX list for haematuria? |
Urethral tear. Cystitis/UTI/Urolithiasis. Idiopathic renal haematuria-> arabs Neoplasia. Drugs. Vaginal varicosities--> multiparous mares. Exercise induced haematuria. Non specific urinary disease like haemolysis, acute myopathies and coagulopathies. |
|
|
How do we differentiate haematuria from haemoglobinuria or myo? |
Small amounts scattered on dipstick is blood. Microscopic exam for cells. Spin down urine and look for pellet of sells. |
|
|
How do we differentiate glomerular from non glomerular bleeding? |
Evaluate the morphology of cells. More variable appearance with glomerular disease. HB casts. |
|
|
How does evaluating timing of haematuria help us tell where it is coming from? |
Throughout urination: kidneys, ureters, bladder. Beginning of urination: distal urethra. End : Proximal urethra and bladder neck. |
|
|
On haematology and biochemistry what would we do with a case of haematuria? |
Any evidence of haemolysis on PCV. Muscle disease--> CK, AST. Coagulation parameters. |

