![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
*14 year old girl with a chief complaint of vomiting and difficulty breathing.
*HPI: Epigastric pain, nausea and vomiting for 36 hr. Persistent vomiting for the last 8 hr. *Past history: Type 1 diabetes diagnosed at 8 yr. Poor glycemic control (Hgb A1c 6 mo earlier 11.3%) attributed to poor compliance. *ROS: Frontal headache x 24 hr. Patient remained alert during this time. No cough. No pain on breathing. No diarrhea or constipation. No fever. *PHYSICAL EXAMINATION T 37˚C, P 104/min, RR 28/min, BP 118/78 Deep respirations. Breath had a strong odor of acetone. Sleepy but oriented. Appeared dehydrated. -HEENT: Normal fundi, EOMs and pupils normal. -Cardiac exam normal, lungs clear, abdomen diffusely tender, but no peritoneal signs. -Perfusion normal, although distal extremities were cool. -No focal neurological findings. |
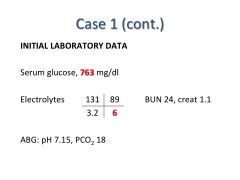
Treated with:
IV Fluids and Electrolytes Intravenous Insulin Full and uneventful recovery |
|
|
5 year old boy with Down syndrome.
3 day history of polyuria, polydipsia and anorexia. Referral to E.R. prompted by decreased intake and drowsiness over 12 hours. Past history: Thyroiditis and alopecia. No congential heart disease. Generally well. PHYSICAL EXAMINATION T 37oC, P 90/min, RR 28/min (Kussmaul breathing), BP 100/70, Weight, 16 kg (estimated 15% below normal weight) Sleepy but easily aroused. Signs of mild dehydration. HEENT: Normal fundi, EOMs and pupils normal. Cardiac exam normal, lungs clear, abdomen non-tender. No focal neurological findings. |
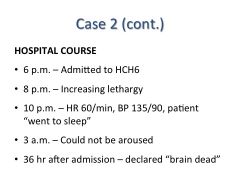
|
|
|
Incidence and Mortality of DKA:
|
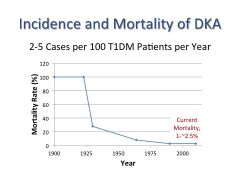
*insulin therapy + IV fluids lowered the mortality.
|
|
|
Effect of stress on metabolic hormones:
|
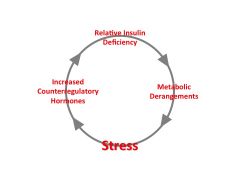
VICIOUS
Big stress here is VOMITING. |
|
|
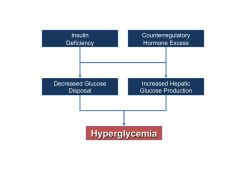
Steps leading to Hyperglycemia in DKA:
|
|
|
|
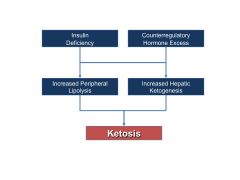
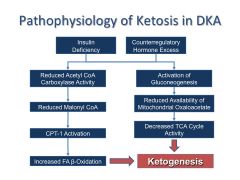
Steps leading to Ketosis in DKA:
|
|
|
|
Regulation of Fatty Acid Metabolism:
|
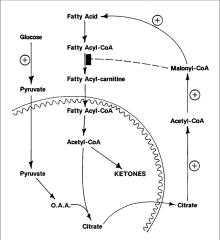
*Insulin stimulates AcCoA carboxylase and FASynthase.
|
|
|
Regulation of Ketoacid Metabolism:
|
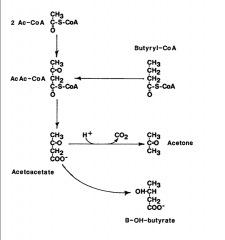
Occurs in the LIVER. Ketogenesis is favored if the amount of AcCoA exceeds the oxidative capacity of the TCA cycle (overflow).
|
|
|
Pathophysiology of Ketosis in DKA:
|
|
|
|
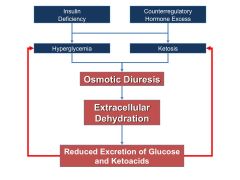
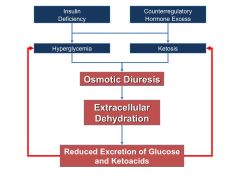
Causes and Effects of Osmotic Diuresis:
|
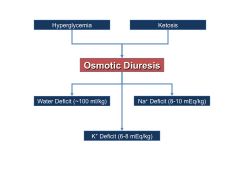
*Both glucose and ketotic acids act as osmotic agents in the urine; holding water in the tubules --> polyuria, dehydration, electrolyte deficits (Na, K).
|
|
|
Body Composition of a Hypothetical 70 kg Male with 17% Body Fat:
|
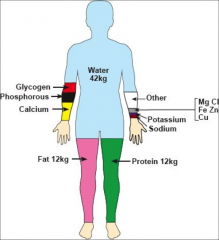
*Big water deficits in DKA (6-7L deficit)
|
|
|
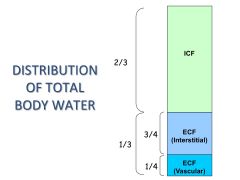
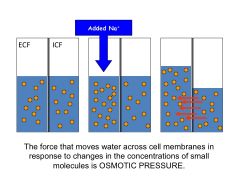
DISTRIBUTION OF TOTAL BODY WATER:
|
|
|
|
Extracellular Electrolyte Makeup:
|
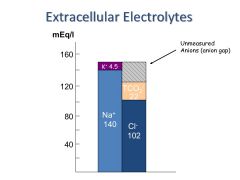
|
|
|
*healthy numbers
|
|
|
|
|
|
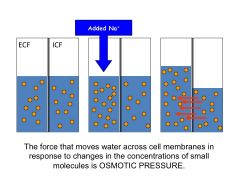
Fluid Shifts in DKA:
|
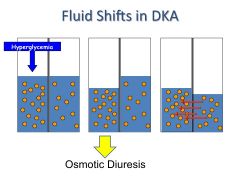
*Combined intra and extracellular fluid deficits
*Extracellular deficit --> combined hypotension and tachycardia |
|
|
Glucose Kinetics:
|
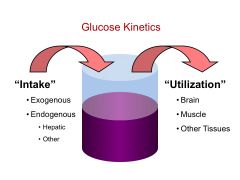
|
|
|
Glucose Kinetics in the starved state:
|
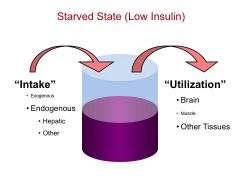
*Muscle use of glucose goes down.
|
|
|
Glucose Kinetics in the fed state:
|
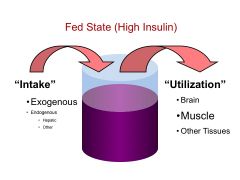
*Muscle use of glucose goes up.
|
|
|
Glucose Kinetics in DKA:
|
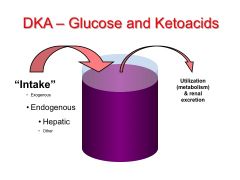
*Inappropriate hepatic glucose production.
*Muscle usage is not upregulated to compensate. |
|
|
|
|
|
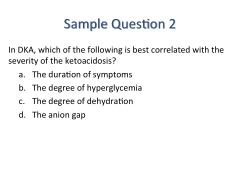
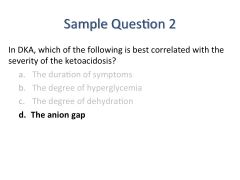
What happens to the anion gap in DKA?
|
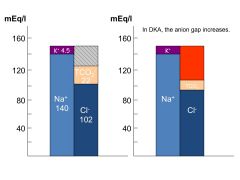
*B/c keto acids represent unmeasured anions.
|
|
|
The HENDERSON-HASSELBALCH EQUATION in DKA:
|
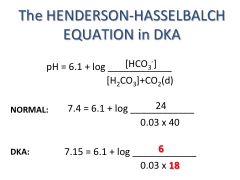
[Bicarb] falls more than CO2 does.
*Metabolic acidosis *Respiratory alkalosis that doesn't compensate ENOUGH --> acidosis. |
|
|
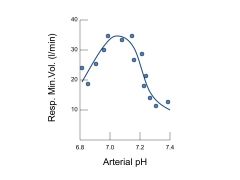
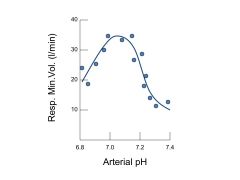
Left side= crash; intubate; pt is on way to death.
|
|
|
Presenting History in DKA:
|
*Past history of diabetes – or a new diagnosis of diabetes (T1DM; rarely other types)
*In pre-existing diabetes, efficacy of management *There are typical symptoms *Precipitating factor -Infection (pneumonia, UTI, a cold...) -Stress (including “life stress”) -Insulin deficiency (can be due to non-compliance) -Infarction (myocardial, cerebral...) |
|
|
Presenting Symptoms in DKA and their causes:
|
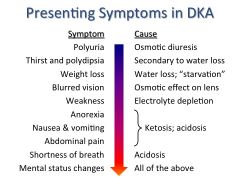
|
|
|
Presenting Signs in DKA and their causes:
|
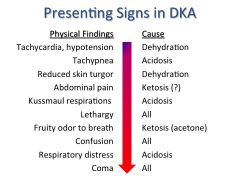
|
|
|
Deficits in DKA:
|
Water – 100 ml per kg (10% dehydration)
Sodium – 7 to 10 mEq per kg Potassium – 3 to 5 mEq per kg |
|
|
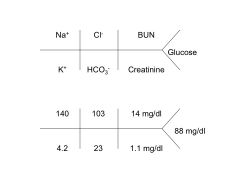
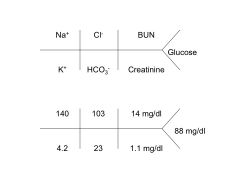
Laboratory Findings in DKA:
|
*Hyperglycemia – typically up to 600 mg/dl
*Ketosis / ketonuria *Anion gap acidosis – pH<7.3; bicarb <15 mEq/l *Hyperkalemia – variable, even though all patients with DKA are potassium depleted. (Can be assessed on an EKG.) *(Hyponatremia) |
|
|
Serum Electrolytes in DKA: K+:
|
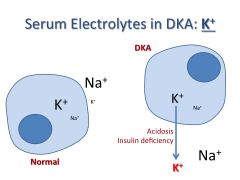
*K leaves the cells b/c blood is acidotic.
*Hyperkalemia in blood --> cardiac rhythm effects *But, overall K deficit. *Treatment: fix the DKA; K will correct itself. |
|
|
Serum Electrolytes in DKA: Na+:
|
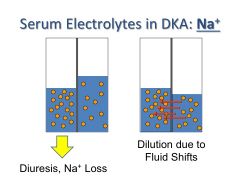
*Na deficit; lost in urine
*Need to replace it. |
|
|
Essentials of DKA Treatment:
|
1) The patient became ill because of a relative insulin deficiency – GIVE INSULIN!!! (regardless of the serum glucose level).
2) Correct deficits: Sodium, water, potassium -Lifesaving! -DKA therapy will reduce serum K+, which can be dangerous. *Standard therapy will repair the acidosis. Buffer is not needed for vast majority of patients. *Monitor and adjust the therapy. |
|
|
IV Fluid Therapy in DKA:
|
*Initial fluid therapy – Normal saline to restore plasma volume
-10 cc per kg body weight (for a normal weight individual) is typical *Continue fluid therapy with: -“Half normal saline” (0.45% NaCl) -Potassium -As serum glucose falls to below ~250mg/dL, add dextrose *Monitor fluid balance |
|
|
Bicarbonate Administration in DKA:
|
*Unnecessary in the vast majority of cases
*Increases the risk of HYPOkalemia (low K+) *Large doses my exacerbate intracellular acidosis *Main indications: -pH<7.0 -Hypotension unresponsive to fluid replacement -Respiratory depression (absence of Kussmaul respirations) |
|
|
(Usual) Insulin Administration in DKA:
|
*Intravenous regular insulin
-Bolus (0.1 U/kg) followed by... -Continuous infusion (0.1 U/kg/hr) *Monitor glycemia at regular (hourly) intervals *Fluid administration will lower serum glucose fast than the acidosis is corrected – Do not lower the insulin dose just because the glucose level is falling!!! |
|
|
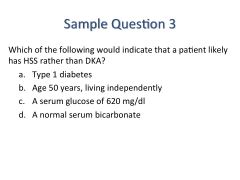
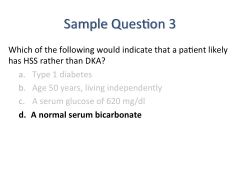
HHS: general--
|
*Hyperglycemia (serum glucose >600 mg/dl)
*Hyperosmolality (>320 mOsm/kg) -Normal, 280-300 mOsm/kg [of water] *Absence of significant ketosis *Harrison’s: “The prototypical patient is an elderly individual with type 2 DM, with a several-week history of polyuria, weight loss, and diminished oral intake that culminates in mental confusion, lethargy, or coma. The PE reflects profound dehydration and hyperosmolality and reveals hypotension, tachycardia, and altered mental status. NOTABLY ABSENT are symptoms of nausea, vomiting, and abdominal pain and the Kussmaul respirations characteristic of DKA.” |
|
|
HHS - Epidemiology:
|
*Age – typically >50 yr
*Type 2 diabetes >>> type 1 diabetes – approximately 1/3 not previously diagnosed *Associated with: -Infection -Diuretic use (worsens dehydration) -Long-term care facility *Mortality 10-40% (high!) |
|
|
HHS - Pathophysiology:
|
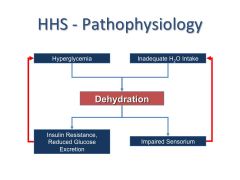
*dehydration is central*
|
|
|
What accounts for the relative absence of ketosis in HHS?
|
*Lesser degree of insulin deficiency? (Especially in the portal circulation)
*Less severe counterregulatory hormone response? *Impaired hepatic ketogenesis? Impaired lipolysis? *UNKNOWN FACTORS *Unlike DKA, these patients don’t come to medical attention until late in their course. |
|
|
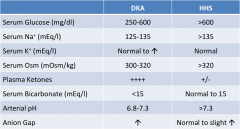
HHS vs. DKA – Lab Results:
glucose na k Osm ketones bicarb pH anion gap |
|
|
|
HHS - Treatment:
|
*Restore volume
-Main risk to patient is CEREBRAL EDEMA, especially in kids. *Provide insulin -Patient will be more insulin sensitive than in DKA -Too rapid a fall in serum glucose may contribute to cerebral edema *Falling glucose → movement of water from ECF to ICF |
|
|
|
|
|
|
|
|
|

