![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
What is insulin released by? |
Beta cells of the islets of langerhans in the pancreas. |
|
|
What is the effect of insulin secretion? |
Stimulated peripheral glucose uptake. |
|
|
Where is glucagon released from? |
Alpha cells of the pancreatic islets of langerhans. |
|
|
What is the effect of glucagon on the body? |
Antagonises insulin action and increases gluconeogenesis. |
|
|
Describe the physiological processes which occur following a meal. |
After a meal blood glucose levels are high 1. This stimulates the secretion of insulin into the blood 2. Cells are stimulated to uptake glucose 3. Blood glucose falls 4. Insulin secretion decreases |
|
|
Describe the physiological processes which occur when exercising or during a fasting period. |
During a fasting period / during exercise blood glucose levels are low 1. This stimulates glucagon secretion 2. glucagon causes cells to release glucose - via gluconeogenesis + glycogenolysis 3. Blood sugar levels of glucose rise 4. Glucose secretion decreases |
|
|
Biochemically, how does insulin increase glucose uptake into cells? |
Insulin promotes transmembrane transport by binding GLUT4 transporters onto cell membranes. |
|
|
Describe the mechanism by which insulin attaches GLUT4 glucose transporters to cell membranes. |
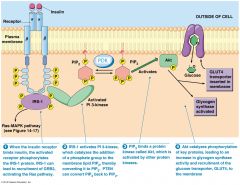
1. Insulin binds to the Insulin Receptor - a tyrosine kinase receptor which autophosphorylates. 2. This activates a signalling pathway via IRS-1 3. IRS1 goes on to activate Pl3 - Kinase, in turn activating PDK (transports PIP3) and finally Akt (which also activates glyogen synthase) 4. The activated signalling pathway causes the translocation of the intracellular GLUT4 transporter to the cell surface 5. GLUT4 binds to the cell surface importing glucose across the membrane into the cell |
|
|
What is the difference between the types of diabetes mellitus? |
1. Primary Diabetes mellitus - Insulin resistance i) Type I - genetic ii) Type II - accrued over time 2. Secondary Diabetes mellitus - Islet of Langerhans pathology i) Congenital rubella ii) Pancreatitis iii) Drugs - corticosteroids |
|
|
What is the cause of primary type I diabetes? |
Antibodies attack beta cells of the islets of langerhans (90% reduction) |
|
|
What is microangiopathy? |
A disease which affects the small blood vessels in the body. |
|
|
What causes microangiopathy? |
Glycosylation of vital proteins - Type IV collagen Overglycosylation of type IV collagen results in its excess deposition into the basement membrane. |
|
|
What is the result of microangiopathy on the function of the blood vessels? |
1. Thick + leaky blood vessels 2. Organ damage 3. Choroid Ischemia and protein loss into tissues |
|
|
How is microangiopathy diagnosed? |
Diagnosed by: 1. Urine tests 2. Blood glucose tests |
|
|
What is the aim of the HbA1C test? |
Aims to measure the long term average of blood glucose levels. |
|
|
Insulin can now be taken as a drug. How has insulin drug efficiency been honed since the leaps in genetic technology? |
Recombinant DNA technology allows creation of differing insulin efficiencies by the creation of modified insulin analogs. |
|
|
What insulin properties be modified? |
1. Activity of the insulin 2. Length of action of insulin |
|
|
What types of drugs can be used to treat type II diabetes? |
1. Sulfonylureas - stimulate beta cells 2. Biguanies - improves cells ability to intake glucose 3. Thiazlidinediones 4. Alpha glycosidase inhibitors - block starch digesting enzymes 5. Meglitinides - stimulates beta cells |
|
|
What is the mechanism of action of sulphonylureas? |
1. Interacts with beta cell receptors to block ATP sensitive K+ channels 2. Blocking of K+ channels causes the opening of Ca++ channels 3. Insulin released |
|
|
What is the mechanism of biguanides? |
1. Inhibits glucose production in liver and increases amount of GLUT4 moved to the cell membranes |
|
|
What is the mechanism of action of thiazolidines? |
1. Binds to and activates the gamma isoform of the peroxisome proliferator activated receptor - 2. The resultant complex controls many glucose / FA metabolism genes |
|
|
What is the mechanism of action of alpha glycosidase inhibitors? |
Block action of enzymes which help to digest starches |
|
|
What surgical treatments exist for diabetes? |
1. Pancreas transplant 2. Islet cell transplants 3. Stem cells |

