![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Blood is the body's only _____ tissue.
|
fluid
|
|
|
|
Blood includes liquid plasma and formed elements such as
|

• Erythrocytes
• Leukocytes • Platelets • Plasma |
|
|
|
Hemocrit
|
% of RBCs out of total blood volume (normally ~45%)
|
|
|
|
What are erythrocytes?
|
red blood cells (RBCs)
|
|
|
|
What are leukocytes?
|
white blood cells (WBCs)
|
|
|
|
What are platelets?
|
membrane bound cell fragments (w/ enzymes); involved in blood clotting
|
|
|
|
What is plasma?
|
non-living fluid matrix (H₂O + electrocytes), proteins, glucose, etc
|
|
|
|
What are the blood plasma components?
|
1) water ~ 92% of plasma
2) > 100 dissolved solutes: a) plasma proteins b) non-protein solutes |
|
|
|
What are plasma proteins?
|
(~7% plasma), most produced in the liver
1) Albumin - most abundant (60% of plasma proteins) 2) Globulins - (35% plasma proteins) 3) Clotting proteins (4% plasma proteins) 4) Enzymes and Hormones (< 1% of plasma) |
|
|
|
What are non-protein solutes?
|
(~ 1% of plasma)
1) Nutrients/waste products 2) Electrolytes (ions) 3) Gases (O₂/CO₂) |
|
|
|
All formed elements are from stem cells in _____
|
bone marrow
|
|
|
|
Only _____ are "complete" cells
|
WBCs
|
|
|
|
What formed element has no nuclei, few organelles; platelets are just cell fragments?
|
RBCs
|
|
|
|
Most formed elements survive in the bloodstream for a few/many days.
|
few
|
|
|
|
Most blood cells do not divide are renewed by cells in _____.
|
bone marrow
|
|
|
|
Describe the structure of an erythrocyte.
|
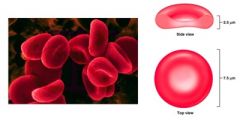
• Biconcave discs
• Increased surface area for gas exchange (~30% more than a round cell) • enables RBCs to bend & flex - squeeze through capillaries • Anucleate - not a "true cell" and few organelles • filled with hemoglobin (Hb) - protein that functions in gas transport |
|
|
|
What is hemoglobin?
|
transports oxygen and carbon dioxide; makes RBCs red
|
|
|
|
Describe the structure of RBCs
|

Structure - complex, quaternary structure
• Globin (protein) + Heme (pigment complex) • Globin = 2 alpha chains and 2 beta chains of polypeptides • Each chain has 1 heme molecule with iron at the center • 1 heme unit "holds" iron in a way that iron can interact with 1 oxygen molecule |
|
|
|
Oxygen loading of hemoglobin occurs in the _____.
|
lungs
|
|
|
|
O₂ diffuses from ______ to blood, then through RBC to bind with hemoglobin
|
lung air sacs
|
|
|
|
When O₂ binds to iron, Hb becomes _____.
|
oxyhemoglobin changes to new 3-d shape → becomes ruby red
|
|
|
|
When O₂ detaches to iron, Hb becomes _____.
|
deoxyhemoglobin color changes to dark red
|
|
|
|
Hb transports ______ of oxygen in the blood (bound to iron of heme group)
|
~ 98.5%
|
|
|
|
Hb transports _____ of carbon dioxide in the blood (bound to globin)
|
~ 20%
|
|
|
|
What is carbaminohemoglobin?
|
when CO₂ bind to glob in's amino acids
|
|
|
|
Carbon dioxide loading occurs at the _____.
|
tissues
|
|
|
|
What is hematopoiesis?
|
blood cell formation in the red bone marrow
|
|
|
|
What is hemocytoblasts?
|

blood stem cells
• produce all formed elements (RBCs, WBCs, and platelets) |
|
|
|
Regulation & Requirements for Erythropoiesis
|
Circulating Erythrocytes - number remains constant and reflects balance between RBC production/destruction
• too few RBCs leads to tissue hypoxia • too many RBCs causes high blood viscosity |
|
|
|
Erythropoiesis is _____ controlled
|
hormonally
|
|
|
|
Erythropoietin (EPO) released by the kidneys is triggered by:
|
• Tissue hypoxia (due to decreased RBCs)
• Decreased O₂ availability • Increased tissue demand for O₂ |
|
|
|
↑ erythropoiesis increases the:
|
• RBC count in circulating blood
• O₂ carrying ability of the blood |
|
|
|
Erythropoietin Mechanism
|
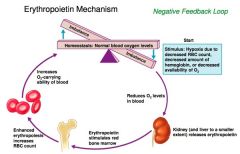
Homeostasis: Normal blood oxygen levels
Stimulus: Hypoxia due to decreased RBC count, decreased amount of hemoglobin, or decreased availability of O₂ |
|
|
|
What are two erythrocyte disorders?
|
anemia and polycythemia
|
|
|
|
What is anemia?
|
blood has normally low oxygen-carrying capacity
**It is a symptom rather than a disease itself • Blood oxygen levels cannot support normal metabolism • Signs/Symptoms include fatigue, paleness, shortness of breath, and chills |
|
|
|
What is polycythemia?
|
excess RBCs that increase blood viscosity
Three main polycythemias are: 1) polycythemia vera (up to 80% hematocrit), bone marrow cancer 2) secondary polycythemia (decrease oxygen availability/excess EPO) 3) blood doping |
|
|
|
Blood plasma can't transport enough O₂ or CO₂ to meet physiological needs
|
• O₂ & CO₂ have limited solubilities in blood plasma
• Tissues need more O₂ & generate more CO₂ than can be absorbed or transported |
|
|
|
Blood plasma can't transport enough O₂ or CO₂ to meet physiological needs and the problem is solved by:
|
Red Blood Cells (RBC)
• Transport O₂ to, and CO₂ from peripheral tissues • Remove O₂ and CO₂ from plasma, allowing more gases to diffuse into blood |
|
|
|
O₂ Transport
Molecular O₂ is carried in the _____: |
blood
• bound to hemoglobin (in RBC) • dissolved in plasma |
|
|
|
O₂ Transport
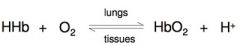
O₂ binds to iron in hemoglobin (Hb) molecules: |
in a rapid & reversible reaction
|
|
|
|
O₂ Transport
Each RBC has about _____ million Hb molecules: |
280 million
• each binds 4 oxygen molecules |
|
|
|
O₂ Transport
• Hb-O₂ combination is |
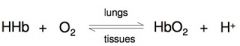
oxyhemoglobin (HbO₂)
|
|
|
|
O₂ Transport
• Hb that has released O₂ is |
deoxyhemoglobin (HHb)
|
|
|
|
O₂ Transport
Each RBC has about _____ million Hb molecules: |
280 million
• each binds 4 oxygen molecules |
|
|
|
What is hemoglobin saturation?
|
percentage of heme units (collectively) in a hemoglobin molecule with bound O₂
|
|
|
|
O₂ Transport
• Hb-O₂ combination is |
oxyhemoglobin (HbO₂)
|
|
|
|
All 4 heme units bound with O₂ is _____ saturation
|
100%
|
|
|
|
O₂ Transport
• Hb that has released O₂ is |
deoxyhemoglobin (HHb)
|
|
|
|
Each Hb (on average) carries 2 O₂ molecules is _____ saturation
|
50%
|
|
|
|
What is hemoglobin saturation?
|
percentage of heme units (collectively) in a hemoglobin molecule with bound O₂
|
|
|
|
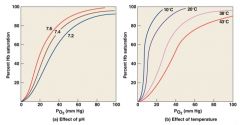
What are the environmental factors affecting the rate of Hb binding/releasing of O₂?
|
1) PO₂ of blood
2) Blood pH 3) Temperature 4) Metabolic activity within RBCs |
|
|
|
All 4 heme units bound with O₂ is _____ saturation
|
100%
|
|
|
|
How does hemoglobin and PO₂ affect the rate of Hb binding?
|
• Hb is almost completely saturated at a PO₂ of 70 mm Hg
• further increase in PO₂ = small increases in O₂ binding |
|
|
|
Each Hb (on average) carries 2 O₂ molecules is _____ saturation
|
50%
|
|
|
|
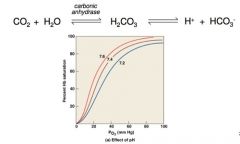
What is oxygen-hemoglobin saturation curve?
|
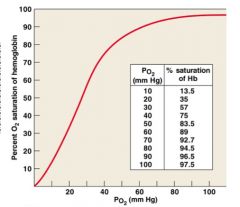
a graph relating the saturation of hemoglobin to PO₂
• rightward shift means more O₂ will be unloading from Hb at a given PO₂ • in active tissues, ↑ temperature, ↓ pH and ↑ PCO₂ promote unloading of O₂ |
|
|
|
What are the environmental factors affecting the rate of Hb binding/releasing of O₂?
|
1) PO₂ of blood
2) Blood pH 3) Temperature 4) Metabolic activity within RBCs |
|
|
|
Hemoglobin and PO₂ is a curve rather than a straight line because
|
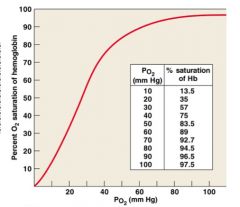
• Hb changes its shape each time O₂ molecule binds
• allows Hb to bind O₂ when O₂ levels are low |
|
|
|
How does hemoglobin and PO₂ affect the rate of Hb binding?
|
• Hb is almost completely saturated at a PO₂ of 70 mm Hg
• further increase in PO₂ = small increases in O₂ binding |
|
|
|
What is oxygen-hemoglobin saturation curve?
|
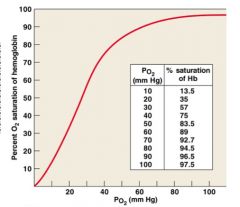
a graph relating the saturation of hemoglobin to PO₂
• rightward shift means more O₂ will be unloading from Hb at a given PO₂ • in active tissues, ↑ temperature, ↓ pH and ↑ PCO₂ promote unloading of O₂ |
|
|
|
Hemoglobin and PO₂ is a curve rather than a straight line because
|
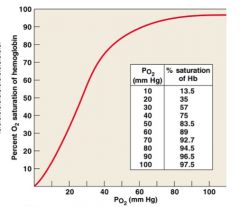
• Hb changes its shape each time O₂ molecule binds
• allows Hb to bind O₂ when O₂ levels are low |
|
|
|
Hemoglobin and PO₂
Carbon monoxide (CO) from burning fuels: |
• binds strongly to hemoglobin and takes place of O₂
• can result in carbon monoxide poisoning |
|
|
|
How does hemoglobin and pH affect the oxygen-hemoglobin saturation curve?
|
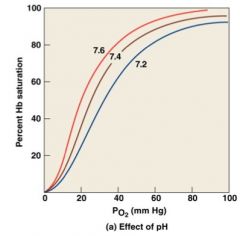
standarized for normal blood (pH 7.4, 37°C)
• When pH drops → more O₂ is released (curve shifts to right & downward) ∙ causes a decrease in oxygen's binding affinity • When pH rises → less O₂ is released (curve shifts to the left & upward) |
|
|
|
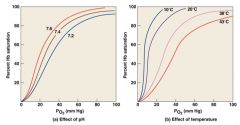
How does hemoglobin and temperature affect the oxygen-hemoglobin saturation curve?
|
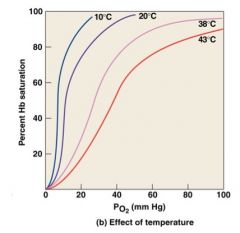
standarized for normal blood (pH 7.4, 37°C)
• When temperature rises → more O₂ is released (curve shifts to the right & down) • When temperature drops → less O₂ is released (curve shifts to the left & up) |
|
|
|
Hemoglobin and temperature
When pH drops or temperature rises: |
more oxygen is released (curve shifts to the right)
|
|
|
|
Hemoglobin and temperature
When pH rises or temperature drops: |
less oxygen is released (curve shifts to the left)
|
|
|
|
Hemoglobin and pH
active tissues generate ____ which lowers the pH of _____ |
acids; interstitial fluid
|
|
|
|
Hemoglobin and pH
A decrease in pH changes the shape of _____ |
Hb
|
|
|
|
Hemoglobin and pH
Shape change = release of ____ by Hb |
O₂ which causes the Hb saturation to decline
|
|
|
|
Hemoglobin and temperature
An increase in temperature causes Hb to release more _____ |
O₂
|
|
|
|
Hemoglobin and
A decrease in temperature causes Hb to bind to _____ more tightly |
O₂
|
|
|
|
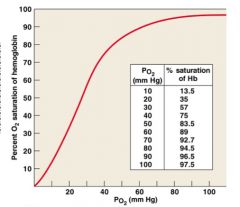
How does hemoglobin and BPG (RBC metabolic activity's effect on Hb) affect the binding and release of O₂?
|
RBC (lack mitochondria) generate ATP by glycolysis which forms lactic acid and BPG (2,3-biphosphoglycerate)
BPG directly affects O₂ binding and release ↑ BPG → ↑ O₂ release |
|
|
|
What are the key concepts of hemoglobin in RBC in O₂ Transport?
|
• carries most blood oxygen
• Hb releases bound O₂ in response to low O₂ partial pressure in surrounding plasma |
|
|
|
If PO₂ increases, hemoglobin _____ oxygen
|
binds
|
|
|
|
If PO₂ decreases, hemoglobin _____ oxygen
|
releases
|
|
|
|
At a given PO₂: hemoglobin will release additional oxygen if:
|
• pH decreases or
• temperature increases or • BPG increases |
|
|
|
What is the Bohr effect?
|
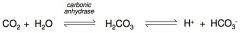
effect of pH on hemoglobin saturation curve (caused by CO₂)
1. CO₂ rapidly diffuses into RBCs once in the blood 2. in RBC, carbonic anhydrase (enzyme) catalyzes a reaction with H₂O to produce carbonic acid (H₂CO₃) 3. Carbonic acid (H₂CO₃) dissociates into hydrogen ion (H+) and bicarbonate ion (HCO₃-) 4. Increase in H+ = decrease in pH |
|
|
|
↑ CO₂ causes the reaction to proceed to the _____
|
RIGHT
|
|
|
|
↓ CO₂ causes the reaction to proceed to the _____
|
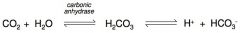
LEFT
|
|
|
|
According to the Bohr effect, how does an increase in CO₂ affect the binding affinity of O₂?
|
add answer here
|
|
|
|
CO₂ is generated as a byproduct of _____.
|
aerobic metabolism (cellular respiration)
|
|
|
|
CO₂ in the bloodstream may be:
|
1. converted to carbonic acid
2. bound to protein portion of hemoglobin 3. dissolved in plasma |
|
|
|
CO₂ in the bloodstream
___% transported as bicarbonate (HCO₃-) • carbonic acid (H₂CO₃) quickly dissociates into H+ * HCO₃- ___% bound to Hb molecule forming carbaminohemoglobin ___% transported as CO₂ dissolved in plasma |
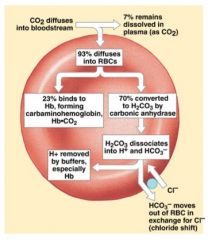
70%, 23%, and 7%
|
|
|
|
Bicarbonate ions move into plasma by an exchange mechanism called the ______ that takes in Cl- ions without using ATP
|
chloride shift
counterbalances negative bicarbonate ions from RBCs |
|
|
|
CO₂ travels in the bloodstream primarily as bicarbonate ions, which form through dissociation of carbonic acid produced by ______ in RBCs
|
carbonic anhydrase
|
|
|
|
Lesser amounts of CO₂ are bound to _____ or dissolve in the _____
|
Hb; plasma
|
|

