![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
Skeletal Structure of Thorax |
12 thoracic vertebrae 12 paris of ribs and costal cartilages (articulate with the vertebrae and sternum) |
|
|
Ribs and costal Cartilage |
Distal portion of the rbis are not completely ossified (costal cartilage) Usefull as it gives the thoracic cage flexibility (CPR) |
|
|
Parts of The Sternum (3) |
Manubrium Body Xiphoid Process- partly ossified until 40 when it completely ossifies. during CPR can snap off and puncture the diaphragm |
|
|
Landmarks of the Thoracic Cage |
Suprasternal Notch- top of the manubrium (above the sternum) Sternal Angle- angle between the manubrium and body |
|
|
Types of Ribs |
1-7 are True ribs- articulate directly with the sternum via costal cartilages 8-10 are False ribs- don't articulate with the sternum.and don't touch the sternum 11-12 are floating- don't articulate with the sternum. Inserted with the muscles of your back (quadratus lumborum) |
|
|
Features of the ribs |
Facets- for articulation with the vertebrae Lateral Sides- the area of the most curvature of the rib Costal Groove- Found on the inferior surface of the rib, a hideout for neurovascular bundles, contains a |
|
|
Features of Thoracic Vertebrae |
Have extra 2 articular processes for articulating with the ribs posteriorly. Ribs articulate via their head and tubercle body and transverse process. Also articulate with the sternum through their costal cartilages |
|
|
Articulations of the Thoracic Ribs |
Some can articulate with more than one thoracic vertebrae One Rib Only- T1, T10, T11, T12 Two Ribs- T2-T9 Have demi-facets to articulate with multiple ribs |
|
|
Intercostal Muscles and the Diaphragm |
All muscles of breathing are skeletal muscle attached to the thoracic cage, so they can create volume in the lungs. |
|
|
External Intercostals (inspiration) |
Superficial Fibres go "hands in your pockets" Actions- pull the ribs upwards towns a fixed upper rib increases volume of thoracic cage. Increases antero-posteral diameter of the thoracic cage.. so it protrudes out in front of you. |
|
|
Internal Intercostals (forced expiration) |
90 degrees to the external intercostals. Working on fixed lower rib. Actions- they depress the thoracic cage (reduce volume) |
|
|
Innermost Intercostals |
Ignore these don't have much function in terms of respiration |
|
|
Diaphragm |
Right segment of the diagram is slightly elevated to accommodate the liver sitting below. |
|
|
Muscles of Breathing (Inhalation) |
Passive Breathing- External intercostals (elevate ribs), diaphragm (pulls dome downwards to increase the superior-inferior dimensions of the lung) Forceful Inspiration- Accessory muscle recruited (sternocleidomastoid, scalenes)- these pull up on the first rib to inroad volume. Note- Asthmatics having trouble breathing recruit these muscles and they get bigger. |
|
|
Muscles of Breathing (Expiration) |
Quiet Breathing- airlift is passive, no muscles, elastic properties of the lung Active Breathing- muscles of the anterior abdominal wall ( help compress the abdomino-pelvic cavity which pushes the viscera up to the diaphragm squishing the lungs), and internal intercostals (press ribs). |
|
|
Intercostal VAN from deep to superficial....1 |
Parietal Pleura- pleura that covers the thoracic wall, reflects down onto the lungs to become the visceral pleura. Single later of epithelial cells that secrete serous fluid to lubricate the pleural cavity.
|
|
|
Intercostal VAN from deep to superficial....2-4 |
2. Innermost intercostal. 3. Ribs- infant of innermost intercostals 4. Costal Groove- in the infer aspect of the rib, protects the VAN) |
|
|
Intercostal VAN from deep to superficial....5 |
5. Intercostal VAN- in the groove is the VAN, in between the internal and innermost intercostals, and sitting in the the costal groove VAN contains- intercostal vein, artery, nerve (thoracic spinal nerve) Segmental Innervation- for each intercostal space there is a separate thoracic level os a spinal nerve |
|
|
Intercostal VAN from deep to superficial....6 |
6. Internal intercostals- span the spaces between the ribs, deepest muscle group |
|
|
Note of Clinical Importance |
If you want to pull fluid off the heart (tamponade) or pneumothorax (collapsed lung with air in the pleural space), the safest way is to aim for the superior aspect of a rib, so that you avoid damaging the intercostal VAN |
|
|
Thoracic Cage-Blood Supply |
There is anatomies for both the arterial and venous blood circuits. |
|
|
Anteries- anastomosis |
Anterior Intercostal Artery- L/R interal thoracic arteries supply it. Also known as internal mammary artery. POsterior Intercostal Artery- Arise from descending aorta, which gives off branches as it passes each go the intercostal spaces |
|
|
Veins-anastamosis |
Anterior intercostal vein, posterior intercostal vein Venous Drainage- There is also an anastomotic venous drainage. Front- for anterior intercostal veins-internal thoracic vein which dumps into the subclavian vein. Back- Left Side (hemiaszygous--1/2 of azygous--- vein will drain into the azygous), Right Side ( azygous vein dumps into the SVC) |
|
|
Where does the diaphragm originate? |
Origin- inferioir dormer of the thoracic cage (along inferior margin of last floating rib across the coastal cartilages) Anterior- Attach to the inferior margin of the ribcage out front, and across the xiphoid process. Posterior- Runs along the inferior margin of the 12th thoracic rib |
|
|
Anatomy of the Diaphragm |
Skeletal Muscle- On the outer margin Central Tendon- Broad flat tendon in the centre The tendon/muscle is suppose by the phrenic nerve (C3-5). travels through the fibrous pericardium to enter to diaphragm. These are voluntary LMNs Note- there is a L/R phrenic nerve |
|
|
Structures that pass through the diaphragm |
They pass through the opening in the diaphragm either the central tendon and the muscle. Structure: Aorta, Esophagus, Inf. Vena Cava |
|
|
Inspiration and the Diaphragm |
Diaphragm moves inferiorly.. helps bring air into the lungs. Shape of the tendon never changes it's the muscle that shortens when the diaphragm contracts |
|
|
Openings of the Diaphragm |
Aortic Hiatus- Descending aorta and thoracic duct pass through here Esophageal Hiatus- Vagus Nerve follows the esophagus though the muscle of the diaphragm. Caval Opening- IVC passes here, its the only structure that pierces the central tendon. |
|
|
Upper Respiratory System (Nose) |
Nasal meatus (nostrils) is the opening here, and it has the vibrissa (hairs) which filter out out particulate matter |
|
|
Upper Respiratory System (Nasal Cavity) |
Lined by mucous membrane. Surround the superior, middle and inferior nasal meatuses in between the conchae. Roles- Protects the lower respiratory system, warms the air, humidifies the air, filters the air |
|
|
Nasal Chonchae |
Bony protrusions (superior, middle, and inferior). Sets up turbulent flow, forcing air to the sides of the nasal cavity, forcing mucous membranes that line it. |
|
|
Cells of the Nasal Cavity |
Lined by pseudostratified, ciliated columnar epithelium. |
|
|
Upper Respiratory System (Sinuses) |
Skull sinuses communicate with the nasal cavities. Sinuses: Frontal (above the nose), Sphenoid (in spheroid bone), Maxillary Sinuses (in upper jaw), Ethmoid Sinuses ( bunch of sinuses in the midline around your nasal bone). |
|
|
Upper Respiratory System (Pharynx) |
Subdivide into 3 regions. Air passes from the nasal cavities into the..... 1. Nasopharynx- (upper most region, associated with the nasal cavity) 2. Oropharynx- Behind the oral cavity, represents a structure that is a conduit of both air and food 3. Laryngopharynx- Structure that is a conduit of air and food, found in the region go the larynx. |
|
|
Pathway of Air vs. Food |
Air- enters through the nasal cavity, don through the pharynx, and past the epiglottis, to get into the larynx, and eventually the trachea Food- enters through mouth and only oropharynx, and laryngopharynx (not nasopharynx) and into the esophagus. The epiglottis has to be closed |
|
|
Upper Respiratory System (Esophagus) |
Trapped between the trachea and the vertebral column at the backWhen you swallow food the esophagus will protrude into the trachea which has an incomplete C-shaped cartilaginous ring so that it can accommodate the food bolus. |
|
|
Larynx |
Extends from C4-C6. Air leaves the pharynx and enter the larynx via the glottis (false vocal cord). Three main cartilages from larynx: Epiglottis - protects the lower airway from food Thyroid - sits above the thyroid gland makes the adams apple Cricoid - defines the inferior border of the larynx
|
|
|
Ligaments in the Larynx |
Vibrate to makes sound. Connective tissues from cartilage to cartilage. Represents the division of the upper to lower airways. Everything above the vocal cords is not clean, everything below is sterile. Epiglottis close during swallowing, and larynx moves superiorly to met the epiglottis. |
|
|
Functions of the Epiglottis |
Close of trachea Generate Couch/Sneeze- Irriation of nasal mucosa causes you to cough. Close off the trachea via the epiglottis and build up pressure in lungs, then open epiglottis. Cough Reflex- Irrant in lower airways. Same as above Sneeze Reflex- irratant in the upper airways. Same as above. |
|
|
Functions of the Epiglottis Cont. |
Expulsive Maneuvers- Close off the epiglottis and contract abdominal muscles, build pressure in the abdominal cavity. The pressure cant go anywhere. This allows: Micturition, Defecation, Childbirth Structural Support- if you are trying to lift something heavy with upper limbs, need thoracic cage to be stable, so close off epiglottis and provides stiffness. |
|
|
Summary of the Upper Airways |
Responsible for helping to condition the incoming air: Warming Moistening Removing particulate |
|
|
Summary of The Lower airways |
Does many of the same things as the upper airways. Still filtering, providing structural support, |
|
|
Trachea |
Right below the larynx. 12 cm long by 3 cm in diameter. Contains 16-20 C-shaped cartilage structures that are incomplete at the back. This makes it ridged.
|
|
|
Trachealis Muscles |
Smooth muscles, involuntary. Under autonomic control, finishes the circle at the back. When it contracts, the trachea gets smaller, makes more difficult to breath. |
|
|
Bifurcation of the trachea |
Divides into primary bronchi (x2) L/R Primary Bronchus- direct air into the L/R lungs. Right bronchus heads straight don where the left takes a more horizontal route. |
|
|
Carina of the trachea |
Internal ridge occurring just before the bifurcation at the bronchial junctions into the primary bronchi. Cough Reflex- ridge is highly innervated by lots of irritant receptors, this stimulates the cough reflex at the carina |
|
|
Trachae lining |
By pseudo stratified, ciliated, columnar epithelium. Help to generate mucocilliary apparatus. Mucous that traps stuff is sweated up into your mouth. |
|
|
Primary Bronchi |
Divide into the R/L lung at the hilus. Primary bronchi enter each lung at the hilus then divide into secondary bronchi. Right Primary- shorter, more vertical. Food will get stuck on this side more often. (aspirated) Left Primary- longer, more angled. Needs to make a detour around the heart |
|
|
Secondary Bronchi |
Direct air to specific lobes of the lung. 3 in the Right and 2 in the Left. |
|
|
Lobes of Fissures of the Lungs (Right) |
Right Lung- Superior, Middle and Inferior Lobes. 2 Fissures that run into the lung tissues and separate the lobes- Horizontal fissure (superior/middle), and Oblique (middle/inferior)
|
|
|
Lobes of Fissures of the Lungs (Left) |
2 Lobes Superior (larger) Lingula (little tongue) end go the superior lobe Cardiac Notch- area that has been cut out for the heart. (a vestigial middle lobe?) Inferior Lobe (smaller) 1 fissure Oblique fissure |
|
|
Iclicker Question |
The trachea is: Involved in conditioning incoming air But is NOT An upper air structure Supported by plates of cartilage Posterior to the esophagus Supported by the pulmonary circuit |
|
|
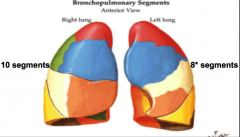
Teriary Bronchi and Bronchopulmonary Segments |
Secondary bronchi continue to divide to create territory (segmental) bronchi. send air tinto the bronchopulmonary segments. 10 tertiary bronchi in the right lung 8 in the left lung. |
|
|
Bronchopulmonary Segment |
Area supplied by tertiary bronchi. Subsections of each lobe of the lung. Functionally and anatomically independent. Have own vasculature, lymphatics and innervation. If you have cancer you can remove one segment and the other will be fine. |
|
|
Cartilage Plates |
Cartilage C-shaped rings in the trachea eventually disappear. They are replaced by cartilage plates (as soon as you get into the primary bronchi). Cartilage Plates- thick shields without the hole at the back. Get smaller and smaller and eventually are replaces with elastic tissues. |
|
|
Schematic of Bronchopulmonary Segments (pic) |
|
|
|
Bronchioles |
Tertiary bronchi divide into bronchioles. bronchioles dive up to 14x to makes terminal bronchioles. Eventually cartilage is replaced by smooth muscle only/ elastic tissue. Serial smooth muscle bands regulated by the ANS. Function of smooth muscle- there's no useful functions, maybe a regents of GI formation?) |
|
|
Innervation of bronchioles |
PSS- contraction (difficult to breath). Increase resistance in the airways. SS- relaxation (easier to ventilate lungs).
|
|
|
Lobule (acinus) |
Gas exchange region. The respiratory reign of the lung with its own pulmonary vasculature/lymphatics. All of these structures are has exchange structures, including: respiratory bronchiole, alveolar duct, alveolar sack. Alveoli- congregate into grape clusters to increase S.A |
|
|
Lobule Cont. |
Each terminal bronchiole forms a lobule. Represents the division between conduction zone of the lungs and the respiratory region. |
|
|
What is a Lobule composed of ?
|
Each has a terminal bronchiole, arteriole and venule (pulmonary circuit), lymphatic vessels, and elastic tissue (to give to recoil). The conducting airway tree are supplied by the systemic circulation called the bronchiole circulation. Why? These conduction airway structures are so thick you can reply on diffusion you need vasculature. |
|
|
Two Circulations in the Lung (systemic) |
Bronchial Arteries (systemic)- supply the conducting region (trachea and terminal bronchioles). The is the bronchiole circuit. Comes off the LV of the heart and feed all the conducting structure |
|
|
Two Circulations in the Lung (pulmonary) |
Service gas exchange regions. Starts at the acinus. Pulmonary arteries come off the RV of the heart and carry de-exygenate blood. Goes to a capillary bed that surrounds each alveolus, and then oxygenated blood goes back to pulmonary vein. |
|
|
Division of the Pulmonary and systemic circulation of the lungs |
The acinus portion of the lung is where the bronchiole circulation stops and the pulmonary circulation beings |
|
|
Functions of the airways (Upper) |
Structural Support- bone, cartilage, smooth muscle Air Conditioning- mucous membranes to warm the air and humidify the air Protection- mucocilliary apparatus NO GAS EXCHANGE! |
|
|
Functions of the airways (Lower) |
Protection- resident innate immune cells, wandering macrophages in alveolar sacs Gas Exchange- increases as you enter the acinus portion of the lung, most occurs at the alveoli |
|
|
Types of alveolar Cells (2) |
Type 1 Alveolar cells (pneumocyte 1)- continuous lining of alveolar wall, squamous=provide greatest S.A, primary site of gas exchange Type 2 alveolar Cells (pneumocyte II)- secrete surfactant, which has hydro-phillic/phobic ends. |
|
|
Surfactant |
Stop like liquid that has hero-phillic/phobic ends. It reduces the surface tension of the mucous which makes the alveoli less likely to collapse.Mucous has water and water likes to attract to itself. This tension is trying to collapse down to alveolus. Surfactant production does not start until 27-28 wks of gestation. Premature infants have trouble inflating lungs. |
|
|
Elastic Fibers of the lungs |
Help to keep the alveoli open. 1/3 of the recall property of the lung comes from elastic fibres, 2/3 from the surface tension of the water. |
|
|
Alveolar Macrophage (dust cell) |
Contributes to protection. Wandering macrophage sitting in airway waiting for bacterium and recognize it (TLR4) |
|
|
Gas Exchange Mechanism |
Gas exchange occurs at alveolar-capillary membrane. 300 million alveoli with S.A of 70 m^2 |
|
|
Details of the Gas Exchange Mechanism |
Gas exchange membrane is in between type 1 alveolar cells and endothelial cell of a pulmonary capillary. Only 0.5um thick. Structure of membrane- plasma membrane of type 1 alveolar call which shares a basement membrane with endothelial cell. Action- has goes between alveoli and blood, O2 in and CO2 out. O2 will load up onto hemoglobin. |
|
|
he end t |
the end |

