![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Ventilation |
Bulk flow of gas into and from the alveolar space |
|
|
Ventilation requirements |
Patent airway Effective respiratory muscle activity Responsive neural control |
|
|
Inadequate ventilation = |
CO2 retention Lowering of blood O2 levels |
|
|
How does anaesthesia affect ventilation? |
Inhibits protective airway reflexes Suppresses mucociliary escalator -> mucus clogging Impairs ventilatory muscles Alters chemoreceptor sensitivity Abnormal body position may impair ventilation |
|
|
Advantages of endotracheal intubation |
Protects airway from foreign material Effective means of providing positive-pressure ventilation Reduces leakage of waste anaesthetic gases |
|
|
Disadvantages of endotracheal intubation |
Larnygeal trauma Excessive mechanical dead space Airway resistance (small diameter) Endobronchial intubation -> increases in V/Q inequalities Tube occlusion or kinking Ischaemic tracheitis (high cuff pressures) Chemical tracheitis (improper sterilisation technique) Upper airway functions bypassed (humidification and warming of gases) Fomite (carrying infectious particles) |
|
|
Why are pigs difficult to intubate? |
Larynx isn't linear and retained active laryngeal reflex (like cats) Local anaesthetic spray or muscle relaxant |
|
|
Rabbits? |
Anatomically difficult - narrow mouth |
|
|
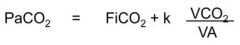
What is the relationship between PaCO2 and alveolar ventilation (VA)? |
Inversely proportional |
|
Which value varies the most? |
VA (FiCO2 = concentration of inspired CO2 VCO2 = volume of CO2 produced by body per unit time) |
|
|
Hypoventilation -> PaCO2 levels |
Increase >45mmHg |
|
|
Why are CO2 inceased pH changes more dangerous than those caused by elevated acids like lactate? |
CO2 crosses cell membranes readily, influencing intracellular pH, widespread effects |
|
|
What types of hypercapnia are there? |
Decreased alveolar ventilation Increased VCO2 - volume of CO2 produced by body Increased FICO2 - concentration of inspired CO2 |
|
|
What causes a decreased VA hypercapnia? |
Decreased respiratory rate, decreased tidal volume, increased dead space (anaesthetics, hypothermia, decreased thoracic compliance, thoracic pain, hypovolaemia) |
|
|
What causes an increased VCO2 hypercapnia? |
Surgical stimulation, pyrexia, malignant hyperthermia, hyperthyroidism |
|
|
What causes an increased FICO2 hypercapnia? |
Rebreathing |
|
|
Tidal volume |
Volume of air displaced between normal inhalation and exhalation when extra effort is not applied |
|
|
Clinical signs of hypercapnia |
Tachypnoea Increased CO (tachycardia and bounding pulse, however anaesthetics may interfere with these) Peripheral vasodilation (brick red mucus membranes, increased bleeding at surgical site) Cardiac arrythmias Extreme - respiratory and cardiac depression (narcotic) |
|
|
What is the effect of increased CO2 on the oxyHb dissociation curve? |
Right shift it - low affinity for O2 |
|
|
Why does hypoxaemia still occur even if alveolar ventilation is adequate? |
Less soluble in blood than CO2 so processes other than ventilation are required to ensure adequate O2 blood levels |
|
|
Which factors influence O2 delivery to tissues? |
Decreased FiO2 (N2O, N2, FICO2) Decreased VA V/Q mismatch (disease, pregnancy, position, hypovolaemia) Haemoglobinaemic (anaemia, methaemoglobinaemia, CO Hbaemia) Stagnant (anaesthetic overdose, cardiac disease, hypovolaemia, polycythaemia) Histiotoxic (left sided ODC, hydrogen cyanide, dinitrophenol) Demand (pyrexia, increased workload, hyperthyroidism) |
|
|
Effects of hypoxia on organs |
Brain - increased intracranial pressure - irreversible neurological damage, convulsions, stupor Myocardium - decreased contractility, dysrhythmias - severe dysrhythmias, cardiac arrest Kidney - nephrosis, oliguria - pre-renal failure, anuria Liver - increased enzymes - necrotizing hepatitis Gravid uterus - fetal acidosis - death, abortion Muscle - pain, compartmental syndrome, myositis |
|
|
Oxygenation and ventilation are not synonymous |
d |
|
|
Spontaneous ventilation |
Animal breathes by itself; anaesthetist exerts no control over tidal volume, respiratory rate and pattern |
|
|
Why is spontaneous ventilation more dangerous in anaesthetised animals? |
Chemoreceptor sensitivity reduced in anaesthetised animals -> hypoventilation |
|
|
Controlled ventilation or intermittent positive pressure ventilation |
R and Vt determined by anaesthetist Manual - compression of rebreathing bag Mechanical - mechanical ventilator |
|
|
SIghing |
Periodic delivery of abnormally large tidal volume - re-expands atalectic regions of lung |
|
|
Advantages of spontaneous ventilation |
Doesn't require mechanical ventilator or presence of anaesthetist Alterations in respiratory pattern and rate in response to surgery provide useful info. on depth of anaesthesia Beneficial effect on CV function as thocolumbar pump preserved |
|
|
Disadvantages |
Hypoventilation and hypercapnia almost inevitable Energy for breathing supplied entirely by patient's own efforts |
|
|
For which operation is IPPV required? |
Thoracotomy |
|
|
Advantages of IPPV |
Fixed volume of anaesthetic reach lungs - stable level of anaesthesia Rhythmic breathing pattern - useful for delicate operations Neuromuscular block not needed |
|
|
Disadvantages |
Animal may fight ventilator -> adverse haemodynamic effects Mechanical ventilators - complex and costly |
|
|
Adverse effects of PPV? |
Reduced cardiac output Lung damage (volutrauma) Increased ventilation/perfusion mismatches Respiratory alkalosis |
|
|
Pulmonary volutrauma |
Lung rupture - only likely if done improperly or on animals with lung pathology |
|
|
Thoracolumbar pump |
Inspiration movements of diaphragm and thoracic wall caudally and outwardly produce an increased intathoracic volume and decrease in pleural pressure. Pressure gradient created from abdomen and head to right side of heart -> facilitates venous return and enhances cardiac output |
|
|
How does PPV affect intrathoracic pressure and venous return? |
Raises intrathoracic pressure and impedes venous return (expels blood from intrathoracic veins into neck and abdomen) Decreased cardiac output and hypotension may occur |
|
|
What is the principle variable lowering cardiac output during PPV? |
Mean intrathoracic pressure |
|
|
In which animals is this a problem in? |
Animals with low compliance lungs -> increases intrathoracic pressure -> decreases CO |
|
|
How can IPPV be altered to reduce systemic vascular resistance caused by high levels of CO2 causing vasodilation? |
IPPV can be used to decrease CO2 -> may increase arterial pressure even if Qt is reduced |

