![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
Ten minutes after an 85-yr-old woman collapses, paramedics arrive and start CPR for the first time. The monitor shows fine (low-amplitude) VF. Which actions should they take next?
|
Beginning cycles of CPR while preparing the defibrillator to use as soon as possible
|
|
|
A cardiac arrest patient arrives in the ED w/ PEA and a heart rate of 30/min. CPR continues, proper ET tube placement is confirmed, and IV access is established. Which medication is most appropriate to give next?
|
Epinephrine 1mg IV
|
|
|
What is an advantage of using hands-free defibrillation pads instead of defibrillation paddles?
|
Hands-free pads allow for a more rapid defibrillation
|
|
|
Which action is performed as you prepare for defibrillator discharge?
|
Continuing compressions while charging the defibrillator
|
|
|
A woman with a history of narrow-complex SVT arrives in the ED. She is alert and oriented but pale. Heart rate is 165/min, and the ECG shows SVT. Blood pressure is 105/70 mm Hg. IV access has been established. Which is the most appropriate initial treatment?
|
Vagal maneuver
|
|
|
What is a common but sometimes fatal mistake in cardiac arrest management?
|
prolonged interruptions in chest compressions
|
|
|
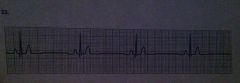
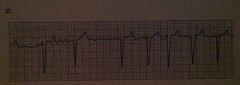
sinus bradycardia
|
|
|
You have attempted endotracheal intubation for a patient in respiratory arrest. When you attempt positive pressure ventilation, you hear stomach gurgling over the epigastrium but no breath sounds. Waveform capnography is zero or flat. Which of the following is the most likely explanation for these findings?
|
intubation of the esophagus
|
|
|
Which statement about IV administration of medications during attempted resuscitation is true?
|
follow IV medications via peripheral veins with a fluid bolus
|
|
|
a 60-yr-old man with recurrent IVF now has a wide-complex rhythm with no pulse after administration of epinephrine 1 mg IV and a third shock. Which drug is most appropriate to give next?
|
Amiodarone 300 mg IV push
|
|
|
while treating a patient in persistent VF arrest after 2 shocks, you consider using IV vasopressin. Which guideline for use of vasopressin is true?
|
Vasopressin is an alternative to a first or second dose of epinephrine in pulseless arrest
|
|
|
which cause of PEA is most likely to respond to immediate treatment?
|
Massive acute myocardial infarction
|
|
|
which drug-dose combination is recommended as the initial medication for a patient in asystole?
|
Epinephrine 1 mg IV
|
|
|
A patient with a heart rate of 40/min reports chest pain. He is confused, and the pule oximeter shows oxygen saturation is 91% on room air. After oxygen administration, what is the first drug you should administer to this patient?
|
Atropine 0.5 mg IV bolus
|
|
|
Which statement correctly describes the ventilations that should be provided after ET tube insertion, cuff inflation, and verification of tube position?
|
Deliver 1 ventilation every 6 to 8 seconds (8-10 ventilations per min) without pauses in chest compressions
|
|
|
A patient in the ED reports 30 mins of severe, crushing, substernal chest pain. Blood pressure is 110/70 mm HG, heart rate is 58/min, and the monitor shows regular sinus bradycardia. The patient has received aspirin 325mg orally, oxygen 4L/min via nasal cannula, and 3 sublingual nitroglycerin tablets 5 minutes apart, but he continues to have severe pain. Which agent should be given next if there are not contraindications?
|
Morphine 2 to 4 mg IV
|
|
|
Which agent is used frequently in the early management of acute coronary ischemia?
|
chewable aspirin
|
|
|
a 50-yr-old man who is profusely diaphoretic and hypertensive reports crushing substernal chest pain and severe shortness of breath. He has a history of hypertension. He chewed 2 low-dose aspirins at home and is now receiving oxygen. Which treatment sequences is most appropriate at this time?
|
Nitroglycerin and then morphine, but only if nitroglycerin fails to relieve the pain and no contraindications exist
|
|
|
a 50-yr-old man has a 3-mm ST elevation in leads V2 to V4. Chest pain has been relieved with sublingual nitroglycerin. Blood pressure is 130/80 mm Hg, and heart rate is 65/min. Which treatment is most appropriate for this patient at this time?
|
percutaneous coronary intervention (PCI)
|
|
|
A 70-yr-old woman reports a moderate headache and trouble walking. She has a facial droop, slurred speech, and difficulty raising her right arm. She says that she takes "several medications" for high blood pressure. Which action is most appropriate at this time?
|
Activate the emergency response system; tell the dispatcher you need assistance for a woman who is displaying signs and symptoms of a stroke
|
|
|
Within 45 mins of her arrival in the ED, which evaluation sequence should be performed for a 70-yr-old woman with rapid onset of headache, garbled speech, and weakness of the right arm and leg? History, physical examination, neurologic assessments, and then a:
|
noncontrast head CT with interpretation by a radiologist
|
|
|
which rhythm is a proper indication for transcutaneous pacing if atropine fails to work?
|
complete AV block with shortness of breath
|
|
|
which cause of out-of-hospital asystole is most likely to respond to treatment?
|
drug overdose
|
|
|
a 34-yr-old woman with a history of mitral valve prolapse presents to the ED with palpitations. Her vital signs are as follows: heart rate is 165/min, resp rate 14/min, blood pressure 118/92 mm Hg, and oxygen saturation is 98% on room air. Her lungs sound clear, and she reports no shortness of breath or dyspnea on exertion. The ECG and monitor display a regular narrow-complex tachycardia. Which term best describes her condition?
|
Stable SVT
|
|
|
a 75 yr old man presents to the ED with a history of light-headedness, palpitations and mild exercise intolerance lasting 1 wk. The initial 12-lead ECG displays atrial fib, which continues to show on the monitor at an irregular heart rate of 120 to 150/min and a blood pressure of 100/70 mm Hg. Which therapy is the most appropriate next intervention?
|
seeking expert consultation
|
|
|
you prepare to cardiovert a 48 yr old woman with unstable tachycardia. the monitor/defibrillator is in sync mode. The pt suddenly becomes unresponsive and pulseless as the rhythm changes to an irregular, chaotic, VF-like pattern. You charge to 200 J and press the SHOCK button, but the defibrillator does not deliver a shock. Why?
|
You cannot shock VF in sync mode
|
|
|
Vasopressin can be recommended for which of the following rhythms?
|
PEA
|
|
|
Chest compressions and effective bag-mask ventilations are ongoing in a patient with no pulse. The ECG shows sinus bradycardia at a rate of 30/min. Which action should be done next?
|
Giving 1 mg epinephrine IV
|
|
|
The following patients were diagnosed with acute ischemic stroke. Which of these patients might be a candidate for IV fibrinolytic therapy?
|
A 62-yr old woman presenting 1 hr after onset of symptoms
|
|
|
a 25 yr old woman presents to the ED and says she is having another episode of SVT. Her medical history includes an electrophysiologic stimulation study (EPS) that confirmed a reentry tachycardia, no Wolff-Parkinson-White syndrome, and no pre-excitation. Heart rate is 180/min. The pt reports palpitations and mild shortness or breath. Vagal maneuvers with carotid sinus massage have no effect on heart rate or rhythm. Which is the most appropriate next intervention?
|
IV adenosine
|
|
|
A pt with a heart rate of 30 to 40/min reports dizziness, cool, and clammy extremities, and dyspnea. All treatment modalities are present. What would you do first?
|
Begin immediate transcutaneous pacing, sedating the patient if possible
|
|
|
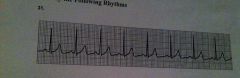
normal sinus rhythm
|
|
|
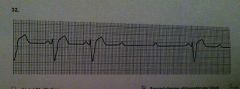
second-degree atrioventricular block
|
|
|
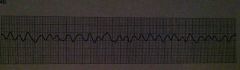
atrial flutter
|
|
|
atrial fibrillation
|
|
|
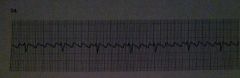
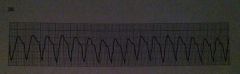
monomorphic ventricular tachycardia
|
|
|
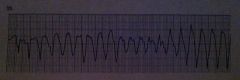
polymorphic ventricular tachycardia
|
|
|
ventricular fibrillation
|

