![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Position of bones after fracture: Non displaced vs Displaced fracture |
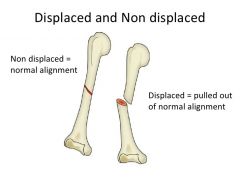
Non displaced fracture - bones aligned Displaced fracture - bones out of alignment |
|
|
Completeness of break: Complete vs Incomplete fracture |
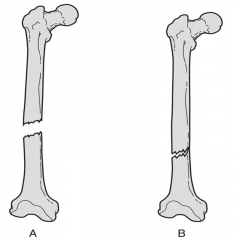
Complete fracture - bone broken through Incomplete fracture - part of bone still attached |
|
|
Orientation of break: Linear vs Transverse |

Linear - parallel to long axis Transverse - perpendicular to long axis |
|
|
Skin penetration: Open (compound) vs Closed (simple) |
Open (compound) - penetrates skin (requires surgery; bone displaced) Closed (simple) - most cases |
|
|
Common fractures: Comminuted |

Bone fragments into three or more pieces. Particularly common in the aged, whose bones are more brittle |
|
|
Common fractures: Compression |
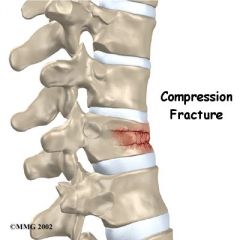
Bone is crushed. Common in porous bones (i.e., osteoporotic bones) subjected to extreme trauma, as in a fall |
|
|
Common fractures: Spiral |
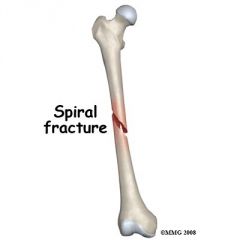
Ragged break occurs when excessive twisting forces are applied to a bone. Common sports fractures |
|
|
Common fractures: Epiphyseal |
Epiphysis separates from the diaphysis along the epiphyseal plate. Tends to occur where cartilage cells are dying and calcification of the matrix is occurring (Happens in younger - disturbs epiphyseal/growth plate) |
|
|
Common fractures: Depressed |
Broken bone portion is pressed inward. Typical of skull fracture |
|
|
Common fractures: Greenstick |

Bone breaks incompletely, much in the way a green twig breaks. Only one side of the shaft breaks; the other side bends. Common in children whose bones have relatively more organic matrix and are more flexible than those of adults |
|
|
Bone disorders: Symptoms |
Bones weaker Pain |
|
|
Bone disorders: Osteomalacia |

Soft bones Ca 2+ is not deposited so bones are weak Symptom - pain |
|
|
Bone disorders: Rickets |
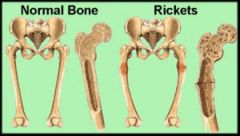
Most common Bones deform - pelvis, skull, ribcage Legs bow Lack of vitamin D and/or Ca 2+ Occurs in children in 3rd world countries |
|
|
Bone disorders: Osteoporosis |
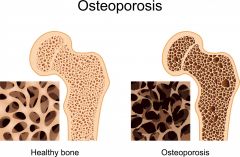
Older people-more so in women than men Bone mass reduced Bones porous and lighter Spongy bone of spine is the most vulnerable Sex hormones restrain the osteoclast activity In menopause: Lower osteocyte = Higher Osteoclast activity |
|
|
Joints: Functional classification - amount of movement |
Synarthroses - immoveable Amphiarthroses - slightly moveable Diarthroses - freely moveable joins |
|
|
Joints: Structural classification - material binding bones together |
Fibrous - immoveable/slightly moveable Cartilaginous - rigid/slightly moveable Synovial - freely moving |
|
|
Joints: Fibrous joints |
Bones joined by fibrous tissue No joint cavity Most immovable 3 types |
|
|
Fibrous joints: Sutures |
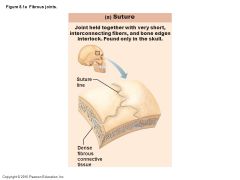
Only skull bones Wavy edges interlock Filled with minimal amount of very short connective tissue Short CT fibers continuous with periosteum Tightly bind bones but allow growth Ossifie in adults, bones fuse to single unit Now called syntheses (body junction) |
|
|
Fibrous joints: Syndesmoses |
Bones connected by a ligament (band) of fibrous tissue Vary in length (longer than in suture) - length determines movement E.g. ligament connecting tibia and fibular - functionally immoveable - Tibiofibular joint (kind of immoveable) |
|
|
Fibrous joints: Gomphoses |
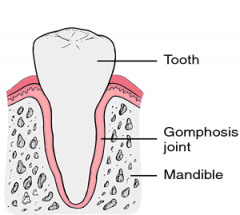
A peg-in-socket fibrous join Tooth in bony alveolar socket only Held in by short periodontal ligament |
|
|
Cartilaginous joints: Synchondroses |
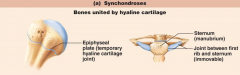
Bone-to-bone joint Hyaline cartilage unites bones Virtually all are synathrotic (immoveable) E.g. epiphyseal plates Are temporary joints - become synostoses (ossified, completely fused) |
|
|
Cartilaginous joints: Symphyses |
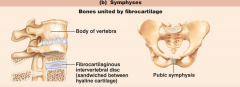
Hyaline (articular) cartilage is fused to a pad of fibrocartilage Allows limited movement of joint (amphiarthrotic) Designed for strength, shock, absorption, flexibility |
|
|
Synovial joints |
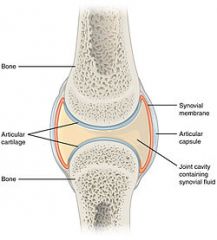
Bones DO NOT touch Articulating bones are separated by a fluid-filled joint cavity Allows a lot of movement (diarthrotic) All limb joints (most joints of the body) 5 distinguishing features (see page 78/79) |

