![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
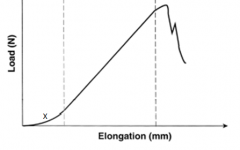
A load-elongation curve for a tendon is shown in Figure A. Which of the following statements accurately describes the region labeled "X"? |
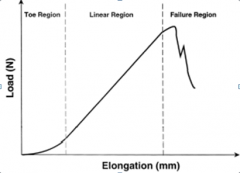
Region "X" in the illustration is the toe region of the load-elongation curve. This region represents the initial elongation during which a small amount of tension causes crimped, randomly arranged fibrils to become aligned parallel along the direction of loading. Magnusson et al looked at the properties of tendon in relation to muscular activity and training. Collagen composition of tendon is organized in a very hierarchical manner along parallel bundles. Tendon collagen bundles have a more parallel orientation along the long axis than ligaments, making their toe region smaller. Illustration A shows all the regions of the load-elongation curve.Ans5
|
|
|
All of the following are independent risk factors for dislocation after total hip arthroplasty EXCEPT?
1. Female gender 2. Osteonecrosis 3. Inflammatory arthritis 4. Post traumatic osteoarthritis 5. Age >70 |
The incidence of dislocation is highest in the first year after arthroplasty and then continues at a relatively constant rate for the life of the arthroplasty. showed that patients at highest risk are female patients (relative risk 2.1),
those with a diagnosis of AVN of the femoral head (relative risk 1.9), an acute fracture or nonunion proximal femur treated with THA (relative risk 1.8), history of inflammatory arthritis (relative risk 1.5), -age greater than 70 (relative risk 1.3). The relative risk of dislocation for patients with posttraumatic arthritis of the hip was not significantly different from that for patients with osteoarthritis (relative risk, 1.3; 95% confidence interval, 0.6 to 2.8) (p = 0.59). Purely post traumatic arthritis should not have an increased risk of dislocation. However, if the post traumatic arthritis occurred after acetabular fixation or proximal femur fractures(mal unions/non unions), then the risk of dislocation is higher than primary OA. Ans4 |
|

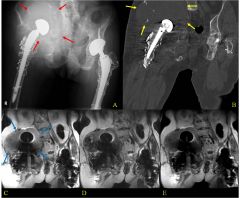
A 60-year-old male had a total hip replacement 8 years ago. Radiographs are shown in Figure A. When discussing the treatment options of acetabular revision versus isolated polyethylene exchange with the patient, what is the most common complication of polyethylene exchange that should be disclosed?
1. Sciatic nerve injury 2. Intraoperative acetabular fracture 3. Postoperative hip instability 4. Infection 5. Catastrophic implant failure |
The radiographs show retroacetabular osteolysis with a well fixed acetabular component. Treatment options include isolated polyethylene exchange versus acetabular revision. patients who had an isolated polyethylene liner exchange for wear or osteolysis and found six patients (25%) dislocated and another 4 patients complained of instability.
isolated polyethylene exchange versus acetabular revision and found a 10% failure rate when retaining the acetabular component. Their cohort had no dislocations, which they attribute to their direct lateral approach. Therefore, although both implant failure and instability are known complications of isolated polyethylene exchange, it is currently believed that hip instability and dislocation are the most common. ANs3 |
|
Varus malalignment after a talar neck fracture with medial comminution causes a decrease in what motion?
1. Tibiotalar dorsiflexion 2. Tibiotalar plantarflexion 3. Subtalar eversion 4. Subtalar inversion 5. Internal rotation |
Varus alignment at the talar neck results in a decrease in subtalar eversion before impingement occurs. Varus talar neck alignment can cause a fixed internal rotation position of the midfoot as the navicular follows the talar head. This can lead to a more rigid hindfoot which is specifically manifested as a decreased eversion range of motion.Ans3
|
|
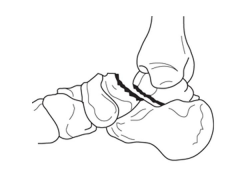
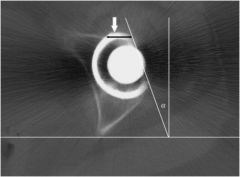
A 34-year-old female is involved in a motorcycle crash. She sustains a talus fracture with associated dislocation of the subtalar joint and maintained congruence of the tibiotalar and talonavicular joints as shown in Figure A. The fracture has healed and she now has symptomatic impingement of the dorsal surface of the talus on the distal tibia and restriction of ankle dorsiflexion. What is the most likely deformity causing these symptoms?
1. Combined varus and plantar malunion 2. Isolated varus malunion 3. Isolated valgus malunion 4. Isolated dorsal malunion 5. Isolated plantar malunion |
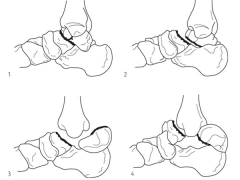
Figure A displays a Hawkins Type 2 talar neck fracture. (Hawkins classification shown in Illustration A). Malunion after inaccurate reduction of talar neck fractures has a reported incidence as high as 32%, with varus malunion occurring most frequently. Dorsal malunion can occur when the body is not properly derotated during reduction and the head fragment remains dorsal to the body. Dorsal malunion can lead to symptomatic impingement of the dorsal surface of the talus on the distal tibia and restriction of ankle dorsiflexion. Canale found that 3 of the 4 patients with dorsal malunion improved following dorsal beak resection of the talar neck. Patients with varus malunion have decreased subtalar range of motion(especially eversion), walk with the foot internally rotated, and often complain of excessive weight bearing on the lateral border of the foot.
Level 4 evidence from Canale and Kelly found that varus malunion occurred most frequently in Hawkins type 2 fractures that had been treated in a closed manner.Ans4 |
|

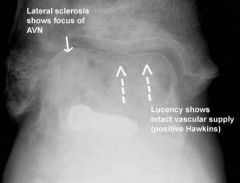
A 30-year-old male undergoes successful surgical fixation of a displaced talar neck fracture. Which of the following is the most likely long-term complication even after anatomic reduction and stable fixation is achieved?
1. Tibiotalar and/or subtalar arthritis 2. Loss of forefoot supination 3. Osteonecrosis 4. Nonunion 5. Infection |

It is important to counsel patients regarding these devastating injuries and their poor prognosis, as osteonecrosis, subtalar and tibiotalar joint degeneration, and talar collapse are not infrequent.
In a series by Lindvall et al, subtalar joint arthritis was reported as more common than osteonecrosis of the talus at 4 year follow-up after fixation. Osteonecrosis of the talus was the next most common complication following surgery.Ans1 |
|

A 14 year-old girl has chronic foot pain which has failed to respond to previous surgical coalition resection and soft tissue interposition. A radiograph of her foot is shown in Figure A. A CT scan demonstrates a talocalcaneal coalition with almost complete involvement of the subtalar joint. What is the treatment of choice?
1. revision coalition resection and extensor digitorum brevis interposition 2. revision coalition resection and fat interposition 3. tibiotalocalcaneal arthrodesis 4. talonavicular arthrodesis 5. triple arthrodesis |
For symptomatic coalition before degenerative changes have occurred, resection is the usual treatment; however, this is not indicated if the patient has failed previous coalition resection surgery, and has greater than 50% involvement of the subtalar joint. Triple arthrodesis involves fusion of the subtalar, calcaneocuboid, and talonavicular joints and is the most effective procedure for fixed hindfoot and forefoot deformities. Subtalar fusion can be performed in select cases with no significant hindfoot deformity. This procedure is contraindicated in young children (10-12 years) because of the limitation it puts on foot growth. Wilde et al found fair or poor results in all ten feet with preoperative CT scans showing an area of relative coalition to be >50% and heel valgus > 16 degrees. Scranton reported consistently successful resections of talocalcaneal coalitions if the coalition was less than one-half of the surface area of the talocalcaneal joint and there was no degenerative arthritic changes in the talonavicular joint.
Ans5 |
|
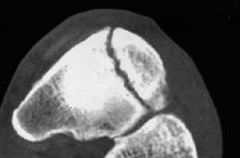
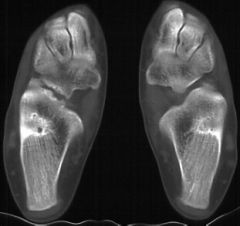
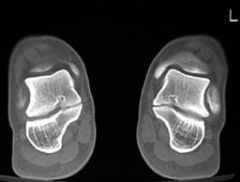
A 24-year-old female who is training for her first marathon presents with six weeks of increasing foot pain. An AP radiograph and representative axial cut of her CT scan of her injury are seen in figures A and B. Management should consist of which of the following?
1. Weight bearing as tolerated in a hard soled shoe 2. Non weight bearing cast immobilization 3. Fragment excision and posterior tibial tendon advancement 4. Percutaneous screw fixation 5. Open reduction with autologous bone graft |

The patient presents with symptoms and imaging studies consistent with a navicular stress fracture. Initial mangement of these injuries consists of non weight bearing cast immobilization.
Khan et al found that patients managed with a minimum of 6 weeks of non weight bearing (NWB) had significantly improved rates of return to sport (86%) compared with patients that were allowed to weight bear as tolerated (26%). After failure of weight bearing management, 6/7 patients who were then NWB in a cast were able to return to sports. Ans2 |
|

a 21-year-old male has 6 months of increasing knee pain and has recently noticed a mass at his knee. Radiographs are shown in Figures A and B. A biopsy specimen of the proximal tibia mass is shown in Figure C. What is the most appropriate first step in management? |
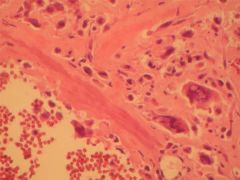
This patient's presentation, radiographs, and biopsy are consistent with telangiectatic osteosarcoma. Treatment is similar to classic osteosarcoma and initially includes multi-agent neoadjuvant chemotherapy (ex. adriamycin, cis-platinum, methotrexate, and ifosfamide) for 8-12 weeks followed by surgical resection (limb-salvage or amputation), followed by additional adjuvant chemotherapy for 6-12 months.
Capanna et al emphasizes that aneurysmal bone cyst's (ABC) occur in the same locations as telangiectatic osteosarcomas, and their radiographic appearances can be confused with each other. The treatment of ABC's are much different and includes intralesional curettage and bone grafting.Ans1 |
|
|
what of the 5 common total hip complications |
|
|
|
|
|
|
|
|
|
was most, is revision for litigation following total hip arthroplasty |

leg length discrepancy |
|
|
most common reason for patient to feel like there is a limp limb length discrepancy |
sensation of feeling long because the abductors are weak using takes 3–6 months to a resolve postop |
|
|
patient presents postop with a feeling of limb length discrepancy
|

|
|
|
patient presents to the office after total hip replacement complaining of groin pain
|
|
|
|
complication can limit the function after total hip replacement |

heterotopic ossification |
|
|
male patient presents to the office after difficult total hip replacement complains of limited function, history of clubbing of the digits, ossifying periostitis and arthritis of the other joints
|
|
|
|
|
|
|
A 45-year-old man has had the gait disturbance shown in Video A ever since a total hip replacement two years ago. Since then he has undergone physical therapy and nerve exploration without any clinical improvement. Extensive AFO bracing was attempted but was not tolerated by the patient. A recent ankle radiograph is shown in Figure A. The Silfverskiold test reveals dorsiflexion of 20 degrees with knee flexion, and 10 degrees with full knee extension. The results of muscle testing using a Cybex dynamometer are shown in Figure B. What is the most appropriate next step in in treatment 1. Ankle arthrodesis in 30 degrees of dorsiflexion 2. Posterior tibial tendon transfer to the lateral cuneiform through the interosseous membrane 3. Split anterior tibial tendon transfer to the cuboid 4. Peroneus longus transfer to the navicular and gastrocnemius recession 5. Flexor hallucis transfer to the navicular and tendo Achilles lengthening (TAL) |
The posterior tibial tendon is the most commonly used donor muscle. Incorrect Answers: |
|

A 62-year-old female has persistent activity related anterior groin pain 10 months after total hip arthroplasty (THA). Infection workup is negative. New radiographs are unchanged compared to the intial films provided in Figures A and B. Pain is temporarily relieved following an injection of lidocaine and cortisone into the iliopsoas tendon sheath. What is the next appropriate treatment option? 1. Indefinite activity modification 2. Iliopsoas tendon release 3. Femoral component revision 4. Acetabular component revision 5. Femoral and acetabular component revision |
After diagnosis of iliopsoas impingement, iliopsoas muscle tenotomy or resection is the treatment of choice if radiographs are within normal limits. In contrast, if imaging shows anterior acetabular overhang (as shown in Illustration A), then acetabular revision would be the next appropriate step in management. |
|
|
A 66-year-old female underwent a surgical procedure 6 weeks ago, and video A demonstrates her gait during ambulation. Based on her gait pattern, which reconstructive procedure did the patient most likely have? (in video the patient is seen from behind and she walked away from the camera and the RIGHT hemipelvis drops)
1. Right total hip arthroplasty through Smith-Petersen approach 2. Left total hip arthroplasty through Smith-Petersen approach 3. Left total hip arthroplasty through modified Hardinge approach 4. Right total hip arthroplasty through modified Hardinge approach 5. Left L2-L3 decompression foraminotomy |
The video demonstrates a left sided Trendelenberg gait resulting from left sided gluteus medius weakness. Left-sided abductor muscle weakness is most likely found in the setting of a left total hip arthroplasty performed through a lateral approach, of the options listed. |
|
|
Risk factors for a motor nerve palsy following primary total hip arthroplasty include all of the following EXCEPT? 1. Developmental dysplasia of the hip 2. Limb lengthening 3. Posttraumatic arthritis 4. Obesity 5. Posterior approach |
Certain pre-operative risk factors may place patients at increased risk for the development of nerve injury during primary total hip arthroplasty (THA). These include a history of developmental dysplasia of the hip (DDH), limb lengthening, posttraumatic arthritis, cementless femoral fixation, and the posterior approach. ans4 |
|
|
|
|

|

|
|
|
|
|

patient comes to the office with hip pain unable to ambulate after total hip prosthesis, patient states he was tying his shoe
|
|
|
|
the patient had a total hip and it needs replacing because of soft tissue deficiency or dysfunction will type surgery is done |
hemiarthroplasty with a large head |
|
|
when a psychiatric patient has multiple hip dislocations for secondary gain what is the treatment or there is significant bone loss and soft tissue deficiency |
resection arthroplasty |
|
|
technique used to increase the tension for the abductor complex |
trochanteric osteotomy and advancement |
|
|
technique you with recurrent instability and a well-positioned acetabular component due to soft tissue deficiency or dysfunction |
constrained acetabular component |
|
|
All of the following are independent risk factors for dislocation after total hip arthroplasty EXCEPT? 1. Female gender 2. Osteonecrosis 3. Inflammatory arthritis 4. Post traumatic osteoarthritis 5. Age >70 |
Dislocation continues to be a problem for patients undergoing total hip arthroplasty. The incidence of dislocation is highest in the first year after arthroplasty and then continues at a relatively constant rate for the life of the arthroplasty. ans4 |
|
|
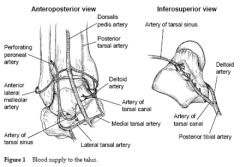
what of the 3 sources of blood supply to the talus |
|
|
|
was the purpose of the Canale view when shooting the foot |
optimal view of the talar neck |
|

|
|
|

|
|
|

|
|
|
|
|
|
|
what is the most common complication with talar neck fracture |
posttraumatic arthritis – subtalar arthritis 50%, tibiotalar arthritis 33% |
|
|
|
|
|
there are two approaches talus anterior medial and anterior lateral which approach is the most important to preserve the deep deltoid ligament |
anterior medial approach |
|
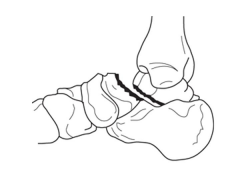
A 34-year-old female is involved in a motorcycle crash. She sustains a talus fracture with associated dislocation of the subtalar joint and maintained congruence of the tibiotalar and talonavicular joints as shown in Figure A. The fracture has healed and she now has symptomatic impingement of the dorsal surface of the talus on the distal tibia and restriction of ankle dorsiflexion. What is the most likely deformity causing these symptoms? 1. Combined varus and plantar malunion 2. Isolated varus malunion 3. Isolated valgus malunion 4. Isolated dorsal malunion 5. Isolated plantar malunion |
Figure A displays a Hawkins Type 2 talar neck fracture. (Hawkins classification shown in Illustration A). Malunion after inaccurate reduction of talar neck fractures has a reported incidence as high as 32%, with varus malunion occurring most frequently. Dorsal malunion can occur when the body is not properly derotated during reduction and the head fragment remains dorsal to the body. Dorsal malunion can lead to symptomatic impingement of the dorsal surface of the talus on the distal tibia and restriction of ankle dorsiflexion. Canale found that 3 of the 4 patients with dorsal malunion improved following dorsal beak resection of the talar neck. Patients with varus malunion have decreased subtalar range of motion(especially eversion), walk with the foot internally rotated, and often complain of excessive weight bearing on the lateral border of the foot.ans4 |
|
|

|
|
|
name to other associated conditions withmultiple tarsal coalition |
|
|
|
with the normal biomechanical function of the subtalar joint |
with the foot into internal rotation and varus in late stent |
|
patient presents with limited subtalar motion hindfoot valgus and recurrent ankle sprains
|
|
|
patient presents with paronychia of spasticity, forefoot abduction and inability to reconstitute the arch when standing on the toes
|

|
|

A 14 year-old girl has chronic foot pain which has failed to respond to previous surgical coalition resection and soft tissue interposition. A radiograph of her foot is shown in Figure A. A CT scan demonstrates a talocalcaneal coalition with almost complete involvement of the subtalar joint. What is the treatment of choice? 1. revision coalition resection and extensor digitorum brevis interposition 2. revision coalition resection and fat interposition 3. tibiotalocalcaneal arthrodesis 4. talonavicular arthrodesis 5. triple arthrodesis
|
For symptomatic coalition before degenerative changes have occurred, resection is the usual treatment; however, this is not indicated if the patient has failed previous coalition resection surgery, and has greater than 50% involvement of the posterior facet of the subtalar joint. Triple arthrodesis involves fusion of the subtalar, calcaneocuboid, and talonavicular joints and is the most effective procedure for fixed hindfoot and forefoot deformities. Subtalar fusion can be performed in select cases with no significant hindfoot deformity. This procedure is contraindicated in young children (10-12 years) because of the limitation it puts on foot growth. Wilde et al found fair or poor results in all ten feet with preoperative CT scans showing an area of relative coalition to be >50% and heel valgus > 16 degrees. Scranton reported consistently successful resections of talocalcaneal coalitions if the coalition was less than one-half of the surface area of the talocalcaneal joint and there was no degenerative arthritic changes in the talonavicular joint. ans5 |
|

A 10-year-old male presents with 6 months of bilateral foot pain at the tarsal sinus. Clinical images of standing examination and heel rise are shown in Figures A and B, respectively. Radiographs of the left foot are shown in Figure C and D. Which of the following findings most likely is associated with this patient's condition? 1. Dynamic supination during swing phase of gait 2. Limited push-off power, limited forefoot contact, and excessive heel contact during stance phase of gait 3. Recurrent ankle sprains 4. Posterior tibial tendon insufficiency 5. Weak tibialis anterior relative to the peroneus longus resulting in first ray plantar flexion |
Recurrent ankle sprains may be associated with tarsal coalition between the talus, the calcaneus, and/or the navicular. Calcaneonavicular coalitions are most common in children aged 8 to 12 years and talocalcaneal coalitions are most common in the 12 to 15 year age group. 10% to 20% of patients with tarsal coalitions have two coalitions and 50% are bilateral. Tarsal coalitions are often asymptomatic, and can present in late childhood or adolescence due to stresses transferred from the rigid hindfoot. Patients with tarsal coalition often exhibit a rigid flatfoot as shown in Figures A and B. |

