![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
The fusion gene resulting from the chromosomal translocation t(X;18)(p11;q11) is chararcteristically found in which malignancy? |
The SYT-SSX1 & SYT-SSX2 fusion genes resulting from the chromosomal translocation t(X;18)(p11;q11) are chararcteristically found in synovial sarcoma. Synovial sarcoma occurs MC in pts 15 to 40 yrs of age & affects M > F. It is a slow growing tumor that has a propensity for the juxta-articular regions around the knee, shoulder, arm, elbow, and foot. tx for synovial sarcoma is wide resection and radiation +/- chemotherapy with a 10 year survival of approximately 25%.
Incorrect Answers: 2-BCR-ABL is an oncogene assoc w/ chronic myelogenous leukemia (CML), the result of a reciprocal translocation between chrom 9 & 22. 3-The EWS (EWSR1) gene is involved in translocations in Ewing's sarcoma, clear cell sarcoma, desmoplastic small round cell tumor & myxoid liposarcoma. The Ewing sarcoma family of tumors is characterized by recurrent translocations that fuse EWS to one of the following genes FLI1 (>90% of cases), ERG, ETV1, E1AF and FEV. 4-4-PAX3-FKHR is a gene fusion in Alveolar RhAns1 |
|
|
Which of the following statements regarding rhabdomyosarcoma is true? |
Rhabdomyosarcoma is the most common soft tissue sarcoma in a child. The most common soft tissue sarcoma in the foot, and a sarcoma which commonly shows calcification on plain radiographs is a synovial cell sarcoma. Hemangiomas are commonly associated with Maffucci's syndrome (multiple enchondromas and hemangiomas). Finally, rhabdomyosarcoma does not dedifferentiate from benign myxomatous tumors. Pappo et al. retrospectively evaluated their cohort of children with rhabdomyosarcoma and tried to evaluate prognostic factors associated with poor prognosis after recurrence. They determined that histologic subtype, stage, and timing of diagnosis were directly related to survival after recurrence. Wexler and Helman review diagnosis and treatment of pediatric soft tissue sarcomas. Ans1
|
|
|
|
|
|
|
|
|
what is the most common and the common associated injury pattern on there with pelvic ring fractures |
|
|
|
regarding prognosis there is a problem to poor functional outcome in chronic pain with injuries associated with what findings – 7 |
|
|
|
what injury pattern do pediatric pelvic ring fractures have
|
children open triradiate cartilages the iliac wing is weaker than an elastic pelvic ligaments therefore the bone fails reported pelvic ring disruption in these fractures really require surgical treatment |
|

|
|
|

|
1=3: sacrospinous ligament; 2=4: sacrotuberous ligament; 1: iliolumbar ligament; 2: posterior iliac sacral ligaments; 5: obturator membrane; 6: lesser sciatic foramen; 7: greater sciatic foramen; 8: interosseous sacroiliac ligaments |
|

patient presents to the emergency room after trauma high speed and there is a leg length discrepancy
|

|
|

|
|
|

|
|
|

|
|
|

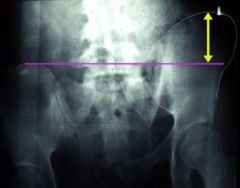
what are the radiographic signs of instability |
|
|

|

|
|
|
|
|

|
|
|
|

|
|
|
was the indication for ORIF of pelvic ring fracture |
|
|
|
|
|
|
|
|
|
|
|
|
lateral compression type III |
|
|
which fracture is also known as crescent fracture located on the side of impact |
lateral compression type II |
|
|
which fracture pattern is most likely cause bladder rupture and urethral injury |

lateral compression type III |
|
|
A 23-year-old male is involved in a motor vehicle accident and sustains a left open femur fracture, right open humeral shaft fracture, and an LC-II pelvic ring injury. Which of the following best describes the radiographic findings associated with this pelvic injury pattern using the Young-Burgess Classification system? 1. Crescent fracture located on the side of impact 2. Widened anterior SI joint, disrupted sacrotuberous and sacrospinous ligaments with intact posterior SI ligaments 3. Complete SI disruption with lateral displacement 4. Sacral compression fracture on side of impact with transverse pubic rami fractures 5. Open-book injury with contralateral sacral compression fracture |
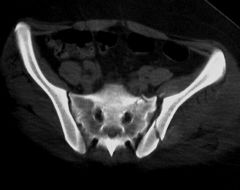
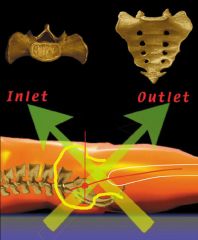
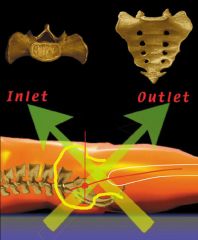
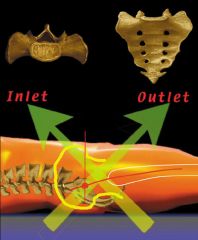
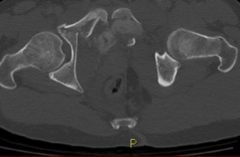
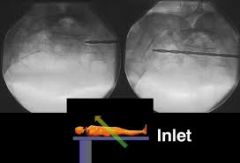
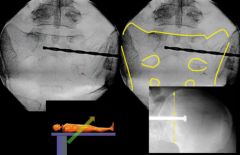
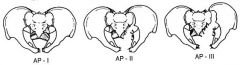
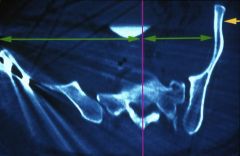
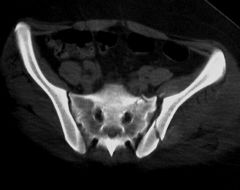
Lateral compression type II fractures (as described by the Young-Burgess Classification System) are associated with a crescent fracture of the iliac wing located on the side of impact. A representative CT scan image and illustration of this injury are shown in Illustration A and B respectively. A table describing each pelvic injury and their associated complications is shown in Illustration C. Illustration D shows each Young-Burgess pelvic injury type. Incorrect Answers: |
|
|
which classification does this description fits 2. Widened anterior SI joint, disrupted sacrotuberous and sacrospinous ligaments with intact posterior SI ligaments 3. Complete SI disruption with lateral displacement 4. Sacral compression fracture on side of impact with transverse pubic rami fractures 5. Open-book injury with contralateral sacral compression fracture |
|
|

what nerve is most at risk when of applying up pelvic ex-fix with supra-acetabular pins through the AIIS |
lateral femoral cutaneous nerve |
|

What nerve is most at risk when applying the external fixator shown in Figure A using a minimally invasive fluoroscopic technique of pin insertion? 1. Ilioinguinal nerve 2. Obturator nerve 3. First branch of the femoral nerve 4. Lateral femoral cutaneous nerve 5. Superior gluteal nerve |
Pelvic external fixation with supraacetabular pins through the AIIS can be utilized to stabilize a pelvic fracture. While using this technique, care must be taken not to injure the lateral femoral cutaneous nerve (LFCN). Gardner et al describe the technique for placement of supraacetabular external fixation pins and state that pins in this location are more stable biomechanically compared to other locations in the iliac crest. Grothaus et al performed a cadaveric study to determine the anatomic detail and variation of the LFCN and the distances it traveled from various landmarks.The found the nerve to potentially be at risk as far as 7.3 cm medial to the anterior superior iliac spine along the inguinal ligament and as much as 11.3 cm distal on the sartorius muscle from the anterior superior iliac spine. Riina et al performed a cadaveric study to define the neurovascular structures at risk with the placement of anterior-posterior locking screws in the proximal femur. They found that risks to the neurovascular structures during anterior-posterior locking in the proximal femur are diminished if locking is performed above the level of the lesser trochanter. |
|
|
What structure has been described as having a risk of injury with retractor placement on the sacrum during combined acetabular-pelvic ring surgery using the Stoppa approach with a lateral window? 1. External iliac artery 2. Pudendal nerve 3. Corona mortis 4. L5 nerve root 5. Ilioinguinal nerve |

Care must be taken when placing a retractor on the anterior aspect of the sacrum, as the L4 and L5 nerve roots are both at risk. |
|
|
was most lower form of inflammatory arthritis |
heumatoid arthritisr |
|
|
|
|

what is the diagnosis rheumatoid arthritis splenomegaly and leukopenia |
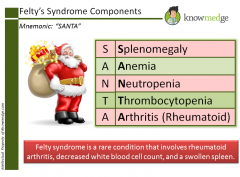
Felty's syndrome |
|
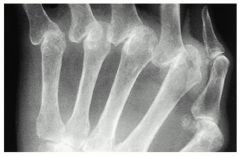
A 64-year-old female with rheumatoid arthritis has decreased functional use of the left hand for activities of daily living. On physical examination she has fixed deformities of the metacarpophalangeal (MCP) joints as demonstrated in Figure A. A radiograph is shown in Figure B. Which of the following management options for the finger MCP joints most likely lead to the least amount of extensor lag and improvement of the ulnar drift at 1-year followup? 1. Tenosynovectomies with extensor indicis proprius (EIP) to EDQ transfer 2. Tenosynovectomies with extensor reconstructions (central slip imbrication, Fowler distal tenotomy) 3. Metacarpal joint resection arthroplasties with palmaris autograft interposition 4. Extensor tendon relocation, extrinsic tendon release, and metacarpophalangeal joint collateral ligament reefing 5. Metacarpophalangeal joint arthroplasties |

The history, clinical image, and radiograph demonstrate severe MCP joint involvement with fixed deformities. MCP arthroplasty is the procedure of choice for severe finger MCP joint arthritis involvement or fixed deformities. Thumb MCP involvement is treated with arthrodesis in most cases. ans5 |
|
|
A 45-year-old woman with rheumatoid arthritis is being scheduled for a total knee athroplasty in 2 weeks. She is currently taking sulfasalazine, Penicillamine, and etanercept, a tumor necrosis factor inhibitor (aTNF-a). What changes should be made to her medication regimen prior to surgery? 1. Discontinuation of all three medications 4 weeks prior to surgery 2. Discontinuation of sulfasalazine 4 weeks prior to surgery, continuation of etanercept and penicillamine 3. Continuation of sulfasalazine, penicillamine, and etanercept 4. Continuation of sulfasalazine and penicillamine, discontinuation of etanercept 4 weeks prior to surgery 5. Continuation of penicillamine, discontinuation of sulfasalazine and etanercept 4 weeks prior to surgery |
Anticytokine disease-modifying antirheumatic drugs (DMARD) have become increasingly popular in the treatment of RA. Immunosuppression and the risk of infection are potential complications for all anti-TNF-alpha medications. Current recommendations for cessation of immunosuppressive therapy are when the drug concentrations are at their lowest levels which include the following: 3 days after etanercept injection; 2 weeks prior to infliximab infusion; 10 days after adalimumab injection. Medications such as sulfasalazine and penicillamine may be continued during the pre and post-operative period. Recent evidence and guidelines such as those reviewed by Keith's paper, suggest that anti-TNF-alpha medications should be stopped 4 weeks prior to surgery. ans4 |
|
|
In the treatment of patients with rheumatoid arthritis, TNF-alpha is blocked by which of the following agents? 1. Tocilizumab 2. Anakinra 3. Etanercept 4. Abatacept 5. Rituximab |
Etanercept is a biochemically designed soluble p75 tumor necrosis factor receptor immunoglobulin G fusion protein, which blocks the downstream effects of TNF. ans3 |
|
|
Which of the following drugs is an IL-1 antagonist typically used as a second line agent in the treatment of rheumatoid arthritis? 1. Anakinra 2. Methotrexate 3. Leflunomide 4. Adalimumab 5. Etanercept |
IL-1 receptor antagonist (IL-1Ra) is a naturally occurring molecule that blocks the biologic effects of the pro-inflammatory cytokine IL-1. A recombinant form of human IL-1Ra, anakinra, is used to manage rheumatoid arthritis patients who are refractory to more conventional forms of treatment. Methotrexate and leflunomide are DMARD's, and are typically prescribed if low dose corticosteroids are ineffective. Adalimumab and etanercept are both TNF-alpha blockers. |
|
|
Which immunoglobulin subtype does the rheumatoid factor target? 1. IgA 2. IgE 3. IgM 4. IgG 5. Rheumatoid factor does not target an immunoglobulin |
Rheumatoid factor is an auto-antibody most commonly seen with rheumatoid arthritis. The presence of rheumatoid factor can also indicate generalized autoimmune activity unrelated to rheumatoid arthritis (e.g. tissue or organ rejection). Rheumatoid factor is itself an IgM antibody that is directed against the Fc portion of IgG antibody. Rheumatoid factor (IgM) attaches to IgG to form immune complexes which are deposited in tissues like the kidney and contribute to the overall disease process in rheumatoid arthritis. ans4 |
|
|
Infliximab is a chimeric monoclonal antibody used to treat rheumatoid arthritis. What cytokine does it target? 1. TGF-beta 2. TNF-alpha 3. CD-20 antigen 4. IL-6 5. IL-1 |
In rheumatoid arthritis, and other chronic inflammatory conditions, cytokines produced by activated T-cells/macrophages contribute to the pro-inflammatory state. TNF-alpha (tumor-necrosis factor-alpha) and IL-1b are thought to be the major cytokines involved in rheumatoid arthritis pathology. Most DMARDs (disease modifying anti-rheumatoid drugs) are directed towards blocking TNF-alpha or its receptors. ans2 |
|

A 43-year-old female with long-standing rheumatoid arthritis complains of right forefoot pain for several years. She has failed conservative treatment and radiographs are shown in Figure A. What is the most appropriate treatment? 1. Bunionectomy 2. Keller procedure with lesser metatarsal head resections 3. 1st MTP joint fusion and lesser metatarsal head resections 4. Forefoot amputation 5. 1st MTP joint interposition arthroplasty and lesser MTP joint arthroplasties
|

Surgical treatment of a rheumatoid forefoot involves fusion of the 1st MTP and lesser metatarsal head resections. The earliest manifestation of rheumatoid arthritis of the forefoot is synovitis of the MTP joints with eventual hyperextension deformity of the MTP joints including distal migration of the forefoot pad, painful plantar callosities and skin ulcerations over bony prominences. |

