![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
9 Cards in this Set
- Front
- Back

Excision of the 1 centimeter talar fragment shown in Figure A would lead to complete incompetence of which of the following structures?
1. Bifurcate ligament 2. Inferior peroneal retinaculum 3. Lateral talocalcaneal ligament 4. Arcuate ligament 5. Posterior talofibular ligament |
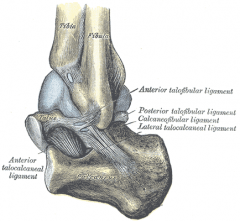
Figure A shows a lateral process talar fracture. Excision of a fragment of approximately 1 cubic centimeter is reported for acute injury as well as painful nonunion/fibrous union. Excision of this piece is shown to sacrifice the entire lateral talocalcaneal ligament as well as 10% of the anterior and posterior talofibular ligaments.
Langer et al performed a cadaveric biomechanical analysis of such an excision and found that ankle and subtalar instability were not created with simple excision of this fragment.Ans3 |
|

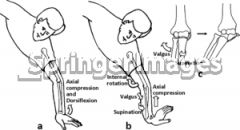
A 34-year-old male has persistent anterolateral ankle pain after a snowboarding injury 1 week ago and is unable to bear weight. Ankle radiographs are negative for fracture. What is the next step in management?
1. MR arthrogram of the ankle 2. Bone scan 3. CT scan 4. Diagnostic injection 5. Repeat radiographs |

Fractures of the lateral process of the talus are frequently overlooked and should always be considered in the differential diagnosis of ankle pain in snowboarders. The common mechanism for fracture is dorsiflexion of the ankle and inversion of the hindfoot. The reference by Vlahovich et al is a case report of a talus fracture in a snowboarder and argues the importance of CT scans in evaluating these injuries as radiographs may fail to show the injury and amount of displacement and comminution of the fracture.Ans3
|
|
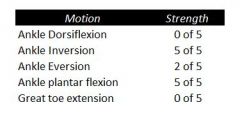
A 45-year-old man has had the gait disturbance shown in Video A ever since a total hip replacement two years ago. Since then he has undergone physical therapy and nerve exploration without any clinical improvement. Extensive AFO bracing was attempted but was not tolerated by the patient. A recent ankle radiograph is shown in Figure A. The Silfverskiold test reveals dorsiflexion of 20 degrees with knee flexion, and 10 degrees with full knee extension. The results of muscle testing using a Cybex dynamometer are shown in Figure B. What is the most appropriate next step in in treatment.
1. Ankle arthrodesis in 30 degrees of dorsiflexion 2. Posterior tibial tendon transfer to the lateral cuneiform through the interosseous membrane 3. Split anterior tibial tendon transfer to the cuboid 4. Peroneus longus transfer to the navicular and gastrocnemius recession 5. Flexor hallucis transfer to the navicular and tendo Achilles lengthening (TAL) |
The clinical presentation is consistent with a sciatic neuropathy following THA in a patient that does not tolerate AFO bracing. Posterior tibialis tendon transfer is the next most appropriate step in treatment. Sciatic neuropathy, especially involving the common peroneal branch, is a known complication of total hip arthroplasty. Typically a patient is adequately treated with an AFO. In some clinical situations an AFO is not tolerated, and a tendon transfer is required. The posterior tibial tendon is the most commonly used donor muscles. Ans 2
|
|
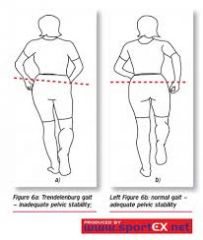
A 66-year-old female underwent a surgical procedure 6 weeks ago, and video A demonstrates her gait during ambulation. Based on her gait pattern, which reconstructive procedure did the patient most likely have?
1. Right total hip arthroplasty through Smith-Petersen approach 2. Left total hip arthroplasty through Smith-Petersen approach 3. Left total hip arthroplasty through modified Hardinge approach 4. Right total hip arthroplasty through modified Hardinge approach 5. Left L2-L3 decompression foraminotomy |
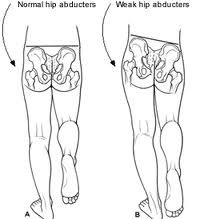
The video demonstrates a left sided Trendelenberg gait resulting from left sided gluteus medius weakness. Left-sided abductor muscle weakness is most likely found in the setting of a left total hip arthroplasty performed through a lateral approach, of the options listed. Ans3
|
|

Which of the following has been shown to increase the rate of failure of cemented femoral components in total hip arthroplasty?
1. Stems that are precoated with polymethylmethacrylate 2. Calcar contact of the collar 3. Smoother implant corners 4. Cement mantle of 2 millimeters 5. Stem material with a Young's modulus higher than 115 GPa |
Precoating a stem with PMMA adds an additional inferface at risk of failure. Stiffer stem materials (higher Young's modulus) improve performance. Titanium has a Young's modulus of 115 GPa with alloy and stainless steel having a higher Young's modulus than titanium. Calcar collar contact adds minimal strength to the construct, but does not lead to premature failure. Smoother corners decrease the rate of failure since they decrease stress risers. The ideal cement mantle is ~2mm. Obtaining less than this would decrease the strength of the construct.Ans1
|
|
TAG
What is the range of pore size of cementless porous implants to allow for optimal bony ingrowth? 1. Less than 1 micron 2. 50 to 400 microns 3. 1,000 to 5,000 microns 4. 10,000 to 50,000 microns 5. 100,000 to 500,000 microns |
The range of 50 to 400 microns is the optimal pore size for cementless porous implants to allow for optimal bony ingrowth.
Bobyn et al looked at the optimum pore size for fixation of porous surfaced metallic implants. Four different pore sizes were examined and placed in canine femurs for 4, 8, and 12 weeks and tested to measure the shear strength based porous sizes. A pore size of 50 to 400 microns provided the maximum fixation strength in the shortest time period (8 weeks), implying maximal bony ingrowth. Ans2 |
|
A 26-year-old male sustains a fall from a ladder onto his outstretched right hand. He is evaluated in the emergency room and is found to have a closed injury to his elbow without evidence of neurovascular compromise. Plain radiographs are obtained and are shown in Figures A and B. During surgery a sequential approach is used to treat each element of this injury. Which part of the procedure is felt to add the most to rotatory stability?
1. Radial head replacement 2. Radial head ORIF 3. Capsular plication 4. Lateral collateral ligament complex repair or reconstruction 5. Medial collateral ligament complex reconstruction |

The essential lesion that results in the most instability in a terrible triad injury of the elbow is rupture of the lateral collateral ligament. Repair of this lesion results in the greatest increase in elbow rotatory stability.Ans4
|
|

At the elbow, the anterior bundle of the medial collateral ligament inserts at which site?
1. Radial tuberosity 2. 3mm distal to the tip of the coronoid 3. Anteromedial process of the coronoid 4. Medial border of the olecranon fossa 5. Radial side of ulna at origin of annular ligament |
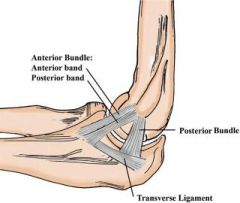
The anterior bundle of the medial collateral ligament of the elbow inserts at the anteromedial process of the coronoid, also known as the sublime tubercle. Fractures at this site have been shown to have worse results with nonoperative treatment, due to increased rates of instability and post-traumatic arthrosis.Ans3
|
|

A 50-year-old woman sustains an open both bone forearm fracture seen in Figure A and undergoes the treatment seen in Figure B. During surgery the posterior interosseous nerve was transected and primary repair was attempted. One year following surgery the patient continues to have no posterior interosseous nerve function. Which of the following treatments will best restore function?
1. Sural nerve grafting to the posterior interosseus nerve 2. Wrist fusion with transfer of the flexor carpi ulnaris to the finger extensors 3. Transfer of the flexor carpi radialis to extensor digitorum and the palmaris longus to the extensor pollicis longus 4. Transfer of the pronator teres to the wrist extensors and the palmaris longus to the finger extensors 5. Transfer of the flexor carpi ulnaris to the wrist extensors and the palmaris longus to the extensor pollicis longus |
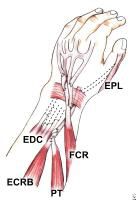
Figures A and B show a pre and post-operative radiograph of a both bone forearm fracture. The posterior interosseus nerve is at risk during surgical approaches to this fracture pattern and care should be taken.
Ropars et al retrospectively reviewed 15 patients who underwent treatment for radial nerve and PIN palsy. For PIN palsy, they concluded the most beneficial transfers included transferring the flexor carpi radialis to the finger extensors (to restore finger extension) and palmaris longus to the extensor pollicis longus (to restore extension of the thumb). In contrast with a radial nerve palsy, with a PIN palsy the patient has adequate wrist extension due to intact ECRL (providing radial wrist extension) supplied by the radial nerve proximal to the PIN.Ans3 |

