![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
What are the 4 effector T cell types a CD4 t cell can become?
|
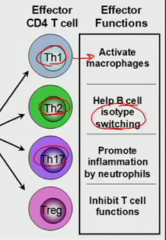
TH17 is adaptive immune response that is using neutrophils (NOT acute inflammation)
Treg is inhibiting immune responses (reg for regulation) |
|
|
Which cytokines are each effector CD4 T cells releasing?
|
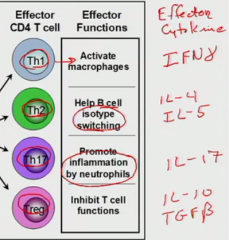
Th1 IFNdelta
Th2 - IL-4, IL-5 class switching and B cell proliferation Th17 - IL-17 strong chemoattractant for neutrophils Treg- transforming growth factor beta - most potent inhibitor (IL-10 is potent too) |
|
|
Who determines the kind of effector cell the t cell becomes?
|
the dendritic cell cytokines
|
|
|
Which cytokines make which cd4 effector T cell?
|
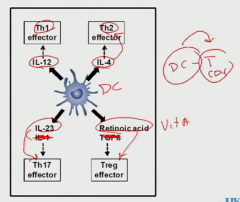
IL-4 is easy because it's associated with B cells
Retinoic acid is derivative of Vit A |
|
|
outline all the cytokines to form and that are released from various CD4 t cells
|
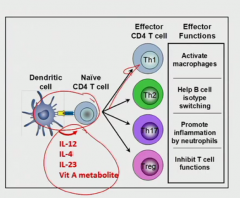
(cytokines released in order)
Th1 IFNdelta Th2 - IL-4, IL-5 class switching and B cell proliferation Th17 - IL-17 strong chemoattractant for neutrophils Treg- transforming growth factor beta - most potent inhibitor (IL-10 is potent too) |
|
|
How does stimulating CD8 t cells work?
include CD8's receptors |
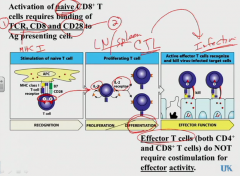
Note it uses MHC I
CTL = cytotoxic T lymphocyte |
|
|
When the CTL is out at the site of infection, how is it stimulated to act on cells?
|
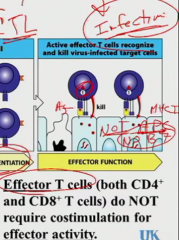
These are NOT APC so they're NOT going to have B7. When cell is in effector T cell mode, it only needs signal 1 (from the 3 point contact MHC Class I) to act
(this is true for activated CD4 T cells too) |
|
|
What other special variation is there to naive CD8 T cell activation?
|
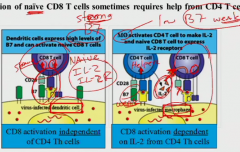
if it's activated by a dendritic cell which has high levels of B7 -> strong co-stimulatory signal 1 and 2 (lots of molecules interacting) -> lots of IL-2 and strong IL-2R
macrophages have low B7 -> fine signal 1 but weak co-stimulatory signal 2 -> CD4 T cell (less demanding, activated fine from macrophage) emits extra IL-2 -> CD8 T cell uses that IL-2 to help get stimulated to activated |
|
|
So your T cells are activated to effectors. How do they find the site of infection? (same process for both CD4 and CD8)
|
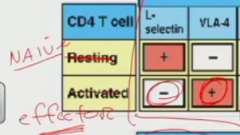
There's a bunch of cell-surface molecules on activated endothelium (from being acted on by proinflammatory cytokines: IL-1, TNFalpha, IL-6, the usual characters). Endothelium now has VCAM-1. Effector T cell has VLA-4 which matches.
Also, we need to know on T cell, L-selectin (low affinity) (lectin binds to CHO) which helps it roll in naive state to get lymph node-- Activated T cell loses L-selectin, so doesn't go inside LN |
|
|
So how do you kill a virus-infected cell with CD8 effector T cell?
|
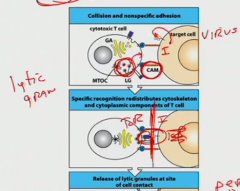
Use TcR and CD8 (signal 1). Doesn't need signal 2.
Infected cell is putting infection Ag out with MHC Class I. To have CTL get near to look, infected cell has CAM for CTL to dock- it's weak and will let go if CTL doesn't match MHC I. When TcR-MHC I happens, CTL lets out lytic granules. |
|
|
What is in a lytic granule?
|
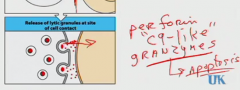
perforin- perforates membrane of target cell by opening pores
it is "C9-like" (C9 being complement). It doesn't make a big MAC. Through the pores, granzymes go in and causes apoptosis (no inflammation!) By magic the CTL doesn't kill itself with the perforin. |
|
|
how many target cells can a CTL kill?
|
no limit really
|
|
|
how does an NK kill? (like mechanism)
|
same mechanism with perforin and granzyme
|
|
|
How does a virus evade immune system?
What are we going to do!? |
downregulates MHC I so CTL can't ID the sick cells
use the NK |
|
|
Natural killer cells are part of the ___ immune system
it has what receptors on surface? how do they work? |
innate
activating receptor. If something binds to it right, NK kills. Inhibitory receptor- says, don't do it! Things like MHC class I bind to this. So if it has both activating and inhibitory receptor, NK won't act. If no inhibitory (since virus playing games), then NK pulls the trigger |
|
|
one of the effector T cells stimulated macrophages. Which one?
|
Th1
|
|
|
What's happening to activate macrophages and what are they like?
|
Th1 go to site of infection and use TcR to interface with macrophage that is infected with bug intravesicular -> MHC class II. So Th1 has signal 1 from MHC class II and makes lots of interferon gamma. (there's CD40L-CD40 Mphi too, but don't worry)
The IFN gamma makes the macrophages become really microbicidal to kill the microbes inside its vesicles. |
|
|
What happens in "partial activation" of macrophage?
|

macrophage is activated just fine, but it still can't kill the material (could be unkillable or a substance like coal dust that just can't be digested). It makes an immune granuloma.
|
|
|
so how are macrophages getting activated exactly?
|
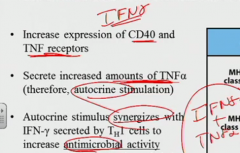
TNFgamma increases CD40 and TNF receptors and increases TNF alpha secretion. So it autocrines itself with TNFalpha and the IFNgamma together makes it go super sayan antimicrobial.
|
|
|
What is different inside activated macrophages that makes them more antimicrobial?
|
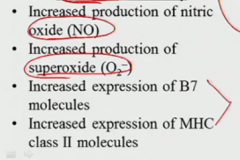
the last two are so it interacts with T cells better (both activated and naive to keep immune response going)
|

