![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
83 Cards in this Set
- Front
- Back
|
Adenodypophysis
|
Anterior Pituitary
|
|
|
Neurohypophysis
|
Posterior Pituitary
|
|
|
Connects the hypothalamus to the pituitary gland
|
Infundibular stalk
COMPRESSION OF STALK will cause decreased dopamine-->Increased Prolactin!!! Macroadenoma |
|
|
List the Anterior Pituitary Hormones (synthesized and secreted)
|
Prolactin
Growth Hormone ACTH LH TSH |
|
|
List the Posterior Pituitary Hormones that are STORED and secreted (Made in the hypothalmus: supraoptic and paraventricular nuclei)
|
Vasopressin (AVP) or antidiuretic hormone
Oxytocin |
|
|
What regulates prolactin and where does it come from?
|
Dopamine; comes from hypothalamus
|
|
|
What stimulates Prolactin synthesis and secretion?
|
reduced dopamine availability to the
lactotroph thyrotropin‐releasing hormone (TRH) estrogen vasopressin vasoactive intestinal polypeptide (VIP) oxytocin epidermal growth factor. |
|
|
What are the functions of prolactin?
|
Breast differentiation
Duct proliferation and branching Glandular tissue development Milk protein and lactogenic enzyme synthesis |
|
|
What drugs can raise the prolactin levels?
|
Metoclopramide and Risperidone
They are dopamine antagonists Increase prolactin >200 ng/ml Also could be estrogens, methyldopa, antipsychotics that block dopamine receptors A prolactinoma has a concentration >250 |
|
|
Mild to moderate hyperprolactinemia (25-100 ng) is typically d/t?
|
Nonprolactin-secreting tumor with infundibular stalk compression and inhibition of dopamine transport to the lactograph
|
|
|
What are the physiological causes of hyperProlactinemia?
|
Pregnancy
Lactation |
|
|
Clinical presentation of Hyperprolactinemia
|
young menstruating women present with menstrual irregularities, galactorrhea, and infertility
Men have decreased libido and ED (d/t inhibition of prolactin inhibiting FSH and LH) Macro more common in Men then women (menstual sx show early) Can have vision changes d/t optic chiasm compression |
|
|
Tx of Hyperprolactinemia
|
Dopamine agonist-->Cabergoline (preferred) or Bromocriptine (patients undergoing fertility induction; requires more dosing)
Both reduce tumor size and restore gonadal function Other Tx: resection, asymptomatic=no tx, Radiation therapy (unresectable; no dopamine) |
|
|
Somatostatin
|
Major inhibitory factor for GH release
|
|
|
GHRH
|
Stimulates GH release
|
|
|
What does GH stimulate? and function
|
IGF-1 (insulin-like growth factor-1); is mostly bound to a protein called IGFBP-3; made in the liver
critical in determining longitudinal skeletal growth and skeletal maturation; carb, lipid and protein metabolis,; increase lypolysis and free fatty acid production; increase protein synthesis |
|
|
unrestrained hypersecretion of GH in adulthood
|
Acromegaly
d/t a GH-secreting pituitary tumor (usually secrete prolactin too) |
|
|
Excessive GH secretion prior to closure of epiphyseal growth plate
|
Gigantism
d/t a GH-secreting pituitary tumor (usually secrete prolactin too) |
|
|
Clinical presentation of Acromegaly
|
Usually present for years; Enlargement of bones and soft tissues of hands and feet; mandible enlargement,, HTN, Viscermegaly, Menstrual abnormalities, hypogonadism, DM type 2, cardiomyopathy, Headache
|
|
|
Diagnosis of Acromegaly
|
Measure serum IGF-1 (usually in excess; has a longer 1/2 life than GH) False negs could include: estrogen ingestion, liver disease, uncontrolled DM, malnutrition
ORAL GLUCOSE tolerance test; usually glucose suppresses GH, but with acromegaly GH levels wont decrease substantially |
|
|
Tx of Acromegaly
|
Transsphenoidal surgery (primary therapy)
Radiation (remission high; can cause Hypopituitarism; need to treat for 5-15 years) Drug: Octreotide and Lanreotide (GH receptor antagonists; somatostatin; cause diarrhea and abd cramping); Pegvisomant (dopamine antagonist (can cause elevated LFTs and increase tumor size!) |
|
|
Deficiency of all anterior pituitary hormones
|
Panhypopituitarism
|
|
|
Manifestations of ACTH deficiency
maybe dont need to know |
Unintentional weight loss
Generalized weakness Lethargy and fatigue Nausea/vomiting/anorexia Abdominal pain Diffuse arthralgias and myalgias Orthostatic hypotension Hyponatremia Hypoglycemia Normal potassium and no hyperpigmentation with secondary adrenal insufficiency |
|
|
Manifestations of TSH deficiency
Same exact symptoms in secondary hypothyroidism maybe dont need to know |
Weight gain
Generalized weakness Fatigue and lethargy Diffuse arthralgias and myalgias Cold intolerance Constipation Dry skin and hair Diffuse edema with periorbital edema Bradycardia |
|
|
GH deficiency in adult manifestations
|
Abnormal body composition with increased visceral fat and decreased lean muscle mass
Psychological impairment with reduced energy, social isolation, emotional lability, depressed mood. Reduced muscle strength and exercise performance Reduced bone mineralization Abnormal lipid profile with elevated LDL and TG and decreased HDL |
|
|
Gonadotropin deficiency or hypogonadotropichypogonadism manifestations
Males and females maybe don't need to know |
Adult males: presents with decreased libido, sexual dysfunction, testicular atrophy, decreased
body or facial hair, decreased muscle mass, reduced bone mineralization Adult females: amenorrhea is the hallmark of hypogonadotropichypogonadism in a premenopausal woman, infertility, vaginal dryness, breast atrophy, reduced bone mineralization, decreased libido |
|
|
Lab levels in panhypopituitarism
|
Low free T4 with low or inapp. normal TSH
ACTH or Insulin stim test to see if cortisol response is <18 Low Testosterone/estradiol with low or inapp. LH and FSH Low IGF-1 (insulin tolerance test, GHRH-arginine stimulation test, glicagon stim test) |
|
|
Panhypopituitarism tx
|
Hormone replacement
TSH-->LEVOTHYROXINE or T4 Estrogen and progesterone (female) also fertility drug Gonadotropin Testosterone; fertility is HCG injections GH is a subQ injection Hydrocortisone in ACTH or Cortisol deficiency |
|
|
Neonate GH deficiency clinical signs
|
Jaundice
Hypoglycemia Microphallus Traumatic delivery (contributing factor) |
|
|
GH deficiency clinical signs in the child
|
Propensity for hypoglycemia
Increased fat High‐pitched voice Microphallus Absent or delayed puberty in the adolescent Weight less affected than height central single tooth |
|
|
GH deficiency in children tx
|
Recombinant human growth hormone; check IGF-1 to determine dose changes
Need smaller does of GH b/c they are more sensitive |
|
|
Histological feature of Pituitary adenoma
|
Loss of mixture of cells seen in the normal anterior pituitary
Chromophobic staining Supporting RETICULIN network is LOST |
|
|
What is the most common pituitary tumor?
|
Prolactin cell adenoma
Chromophobic staining More common in Women than men Will have immunostaining against specific hormones |
|
|
Acidophilic staining
|
Growth hormone adenoma
|
|
|
Chromophobic staining
|
Prolactin cell adenoma
|
|
|
Basophilic Staining
|
ACTH cell adenoma
Cushings disease |
|
|
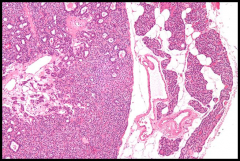
Craniopharyngioma age peaks
and symptoms |
–Children (5 to 14yrs): usually adamantinomatous type
–Adults (65 to 74 yrs): usually papillary type Visual abnormalities; hypopituitarism |
|
|
Microscopy of craniopharyngioma
Adamantinomatous and Papillary type |
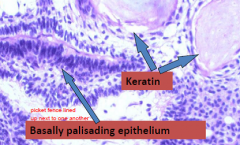
Adamantinomatous-->Cystes filled with dark brown fluid (motor oil) and cholesterol crystals; PALISADING SQUAMOUS EPITHELIUM; ABUNDANT KERATIN
Papillary type-No Keratin formation |
|
|
Postpartum pituitary necrosis caused by ischemia of the pituitary gland
|
Sheehan syndrome
|
|
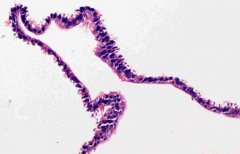
Cysts lined by ciliated cuboidal cells with scattered goblet cells and anterior pituitary cells
|
Ranthke cleft cyst
|
|
|
Hormones synthesized in hypothalamus and transported via axons
|
Oxytocin and Antidiuretic hormone
Syndromes inclue SIADH and Diabetes insipidus |
|
|
What are the cell types in the parathyroid?
|
Chief cells (main cell type)-secret PTH
oxyphilic cells (darker stained) NORMAL parathyroid has a large amount of intervening stromal fat |
|
|
How is hormone secretion controlled in the parathyroid gland
|
Calcium; related to bone disease-->osteitis fibrosia cystica; erosion of bone matrix by osteoclasts
Brown tumor-->reactive giant cells, hemorrhage (picture) |
|
|
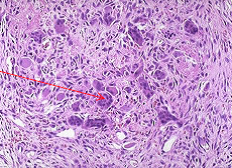
Parathyroid adenoma histology
|
Most common
solitary nodule in a SINGLE parathyroid gland Loss of normal adipocytes A rim of compressed normal parathyroid at periphery (on right in image) Other glands may become atrophied |
|
|
Difference between parathyroid hyperplasia and adenoma
|
Hyperplasia doesnt have a rim of normal gland at periphery and all 4 glands are involved
|
|
|
Parathyroid carcinoma characteristics
|
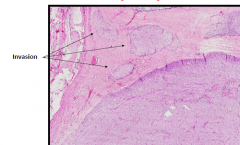
Firm (adenomas are soft); adheres to surrounding tissue d/t infiltration outside of the parathyroid capsule
Invade of surrounding tissue/metastasis Look for mitotic activity, fibrous bands, and capsular/vascular invasion Difficult to remove |
|
|
Cystic lesions within bone caused by bone resorption leading to thinned cortex and
marrow fibrosis with cystic degeneration |
Osteitisfibrosacystica
Bone lesion caused by hyperparathyroidism |
|
|
Brown tumors of hyperparathyroidism
|
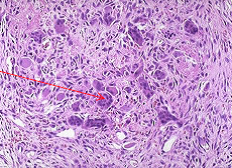
Aggregates of osteoclasts, reactive giant cells, and hemorrhagic debris form these
benign masses that can be mistaken for bone neoplasms |
|
|
Where is Ca mainly absorbed
|
Duodenum and jejunum
|
|
|
How is Calcium absorption regulated
|
regulated by 1,25(OH)2D
Synthesis of 1,25(OH)2D is regulated by PTH |
|
|
Calcimimetic (cinacalcet) treats
|
hyperparathyroidism' Will decrease PTH (neg feedback)
|
|
|
Loss of CaSR function
|
Familial hypocalciuric hypercalcemia (FHH)
|
|
|
Gain of CaSR function
|
Autosomal dominant hypocalcemia (ADH); excrete too much calcium; not enough Ca+2 in the blood
|
|
|
Plant vit D
|
D2
|
|
|
PTH stimulates what reaction?
|
1-hydroxylation of 25(OH)D in the kidney
|
|
|
Symptoms of hypercalcemia
|
Fatigue
Nausea, constipation Anorexia Polyuria, polydipsia Memory impairment Thinning of the bone cortex (can also cause Hyperparathyroid osteitis) Can lead to a vicious cycle of hypercalcemia |
|
|
Primary Hyperparathyroidism can be d/t
|
Sporadic (carcinoma, single gland disease)
Multiple endocrine neoplasias (MENs) Hyperparathyroidism jaw tumor syndrome FHH Familial isolated hyperparathyroidism |
|
|
Familial Hypocalciuric Hypercalcemia
|
Asymptomatic, modest LIFELONG (cant be aquired) hypercalcemia
Hypocalciuria PTH not suppressed Autosomal dominant Surgery not indicated THE KIDNEY IS GOING TO HOLD ONTO THE CALCIUM (receptors in the kidney too) |
|
|
Genetics of FHH
|
– FHH1 Most families - CaSR (chromosome 3)
(~2/3) • Codominant - neonatal severe hyperparathyroidism Not all FHH have CaSR mutations Recent discovery of FHH2 and FHH3 |
|
|
Causes of PTH-Independent Hypercalcemia
|
Malignancy-->cone metastases, osteoclast activating factors, etc
Calcitriol mediated (inflammatory) Hyperthyroidism Milk/calcium-alkali syndrome Immobilization |
|
|
Parathyroid-Hormone related peptide
|
Humoral hypercalcemia of malignanc (breast, lung, kidney, squamous); Not measured on PTH assays
important in fetal development found in high concentrations in milk |
|
|
Calcitriol (1,25[OH]2D)-Mediated Hypercalcemia
(Non-renal/unregulated expression of 1-hydroxylase) |
Sarcoid, Lymphoma
|
|
|
Treatment of Hypercalcemia
|
IV fluids
Loop diuretics-Furosemide (augment Ca+2 excretion; need to make sure that the pt is hydrated) Calcitonin (Escape from the hormone) Bisphosphophonates (inhibit osteoclastic bone resorption; preferred medication) |
|
|
Sx of Hypocalcemia
|
Neuromuscular irritability (paresthesias, cramps, tetany)
Lowered seizure threshold Mental status changes Cardiac (prolonged QT, arrhythmias) Basal ganglia calcification Cataracts Positive Chvostek's and Trousseau's sign |
|
|
Short stature
Round face Short metacarpals (esp 4th) Subq ossifications |
Albright's Hereditary Osteodystrophy (AHO)
|
|
|
Hypoparathyroidism can be d/t
|
• Genetic disorders
• Autoimmune • Infiltrative • Pseudohypoparathyroidism (PTH resistance; GNAS mutation and Albright's) – Type 1a has GNAS mutation and Albright’s Hereditary Osteodystrophy (AHO) |
|
|
Tx of hypocalcemia
|
Acute hypocalcemia is initially managed with IV calcium gluconate.
Chronic hypocalcemia due to hypoparathyroidism is treated with calcium supplements and either vitamin D2 or D3 or calcitriol (calcitrol works better especially if they have primary hypoparathyroidism) |
|
|
FGF23
|
made in bone cells
Increases Urinary Phosphate excretion Decreases renal production of 1,25(OH)2D kind of like the opposite to PTH |
|
|
Excess FGF23 causes
|
hypophosphatemia and impaired bone mineralization
|
|
|
Decreased FGF23
|
Causes hyperphospatemia and tumoral calcinosis (very difficult to treat)
Occurs in many genetic forms of Rickets |
|
|
Causes of Hypophosphatemia
|
Reduced renal tubular phosphate reabsorption
Excess FGF23 or other "phosphatonins" Impaired intestinal phosphate absorption • Shifts of extracellular phosphate into cells Intravenous glucose Insulin therapy for prolonged hyperglycemia or diabetic ketoacidosis Catecholamines (epinephrine, dopamine, albuterol) Acute respiratory alkalosis Rapid cellular proliferation • Accelerated net bone formation Intrinsic renal disease that causes phos wasting |
|
|
Causes of Hyperphosphatemia
|
• Impaired renal phosphate excretion
Renal insufficiency Hypoparathyroidism Pseudohypoparathyroidism Tumoral calcinosis • Vitamin D intoxication • Sarcoidosis, other granulomatous diseases • Massive extracellular fluid phosphate loads Rapid administration of exogenous phosphate (intravenous, oral, rectal) Extensive cellular injury or necrosis • Transcellular phosphate shifts Metabolic acidosis Respiratory acidosis |
|
|
Macroadenoma
|
Compression of infundibular stalk
|
|
|
Presentation of Macroprolactinomas
|
Headache, vision changes
|
|
|
Dx of GH deficiency in Children
|
Clonidine and Argining HCl tests
|
|
|
Sheehan's Syndrome
|
Postpartum ischemic necrosis of pituitary gland; Pituitary gland enlarges in pregnancy (d/t increased lactotrophs); obstetrical hemorrhage or shock
Sheets of dead areas in the pituitary |
|
|
Rathke Cleft Cyst Histology
|
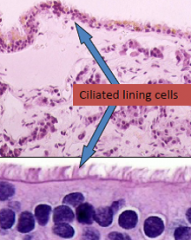
Columnar to cuboidal cells with cilia and occasionally mucin
Mass effect type lesion |
|
|
Large pituitary adenomas can cause
|
bitemporal hemianopsia
|
|
|
PTH effects
|
Kidney: Ca++ reabsorption and convert 25(OH)D to 1,25(OH)2D
Intestine: Ca++ absorption Bone: Ca++ resorption |
|
|
PTH and phosphate
|
decreases phosphate absorption; carries large amounts of Ca in the urine
|
|
|
Causes of PTH-independent Hypercalcemia
|
Bone metastases, PTH-related protein, Unregulated Calcitriol production (1,25(OH)D), Hyperthyroidism (increases bone resorption), immobilization
|
|
|
Create differential flow chart if patient has hypercalcemia
|
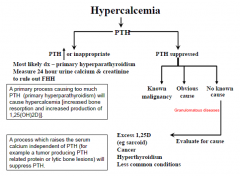
|
|
|
Create differential flow chart for Hypocalcemia with normal renal function
|
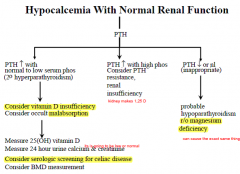
|

