![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
The four (4) classes of lipoproteins, where they are synthesised and their role in lipid transport. (SN)
|
Chylomicrons:
enterocyte cells in small intestine in the fed state Synthesised in small intestine (enterocytes) 100 – 1000nm Transport dietary TG VLDL: Synthesised in liver 30 - 90nm Transport endogenous TG LDL: Liver Formed from hydrolysis of VLDL 20nm Transport cholesterol to tissues HDL: Liver and small intestine Transport cholesterol from tissues to liver 7 – 10nm |
|
|
(SN) The two (2) lipoprotein classes that contain the greatest amounts of cholesterol and the two (2) classes that play major roles in triglyceride transport.
|
Cholesterol Lipoproteins: LDL, HDL
Triglyceride Lipoproteins: Chylomicrons, VLDL Chylomicrons enterocyte cells in small intestine in the fed state Synthesised in small intestine (enterocytes) 100 – 1000nm Transport dietary TG VLDL Synthesised in liver 30 - 90nm Transport endogenous TG LDL Liver Formed from hydrolysis of VLDL 20nm Transport cholesterol to tissues HDL Liver and small intestine Transport cholesterol from tissues to liver 7 – 10nm |
|
|
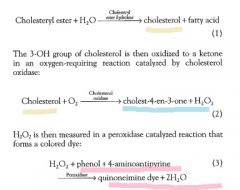
(SN) The basis of the routinely performed assays to measure total cholesterol.
|
1. Enzymatic assays
2. Enzymes in single photometric agent 3. Mixed with serum/plasma 4. incubated controlled conditions for colour development 5. 1. Hydrolysing step 6. Cholesterol esterase frees cholesterol from cholesterol esters 7. Cholesterol esters → (cholesterol esterase) → free cholesterol 8. 2. Oxidation Step 9. Cholesterol oxidase oxidises the cholesterol to cholestenone 10. Cholesterol + O2 → (cholesterol oxidase) → Cholesterone + H2O2 11. Measurement Step: 12. 2H2O2+ Phenol + 4-Aminophenazone → 4H2O + Quinoneimine dye 13. – Use of a Catalase reaction also used H2O2+ Ethanol → Acetaldehyde and H2O → Aldehyde dehydrogenase → → Acetaldehyde + NADP → Acetate + NADPH + H+ |
|
|
(SN) The basis of the routinely performed assays to measure triglycerides
|
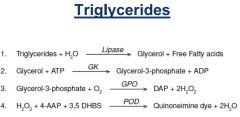
1. Enzymatic
2. Lipase splits the glycerol from TG 3. Glycerol kinase then take glycerol and ATP to Glycerol-3-phosphate 4. Measurement of glycerol-3-phophate can be done via - Glycerol Phosphate Oxidase reaction: colormetric measurement of the quinoneimine dye formed (Trinder) - Pyruvate Kinase Reaction Decrease in NADH at 340nm - Glycerol-3-Phophate Dehydrogenase Reaction Colormetric measurement of formazan |
|
|
Lipid profile commonly seen in diabetic patients
|
Diabetics (especially T2DM patients) are at more risk of CVD than those who don’t have diabetes. Of primary concern is secondary hyperlipidaemia as a result of their diabetes. They also run the risk of having elevated Chylomicrons and VLDLs in their blood. Uncontrolled DM patients also run a high risk of having elevated levels of Lipoprotein (a) in their blood. Patients with elevated Lp (a) have been shown to have a significantly higher risk of atherosclerotic disorders forming.
|
|
|
In the small intestine, _____ is (are) emulsified by bile acids to form micelles.
a) Lipase b) Cholesterol c) Starch d) Monosaccharides |
b) Cholesterol
Cholesterol is first solubilised through a process called emulsification, which occurs by the formation of micelles that contain unesterified cholesterol, fatty acids, monoglycerides, phospholipids, and conjugated bile acids. Bile acids, by acting as detergents, are the most critical factor in micelle formation. |
|
|
Cholesterol is transported in the blood as cholesterol esters mainly in
a) chylomicrons. b) very low-density lipoprotein (VLDL). c) high-density lipoprotein (HDL). d) low-density lipoprotein (LDL). |
LDL carries about 70% of total plasma cholesterol, but very little triglyceride.
|
|
|
Which one of the following formulae is the correct calculation for indirectly measuring LDL
cholesterol (Friedewald’s formula)? a) LDLc = HDLc + (0.45 x triglyceride) b) LDLc = total cholesterol - HDL - (0.45 x triglyceride) c) LDLc = total cholesterol + HDL + (0.45 x triglyceride) d) LDLc = HDLc - (0.45 x triglyceride) |
LDLc = total cholesterol - HDL - (0.45 x triglyceride)
|
|
|
There is an inverse relationship between which one of the following cholesterol-containing
lipoproteins and increased risk of CHD? a) VLDL b) LDL c) Chylomicrons d) HDL |
HDL
In contrast to LDL cholesterol, increased HDL cholesterol concentrations have been shown to be protective for CHD. |
|
|
The initial step in the analysis of serum triglyceride concentration is
a) hydrolysis of esters to form free triglyceride and fatty acids. b) oxidation of triglyceride to form glycerol-1-phosphate. c) hydrolysis of triglyceride to form glycerol and fatty acids. d) reduction of triglyceride to form triglyceride esters and cholesterol. |
a.
hydrolysis of triglyceride to form glycerol and fatty acids. In all methods of triglyceride analysis, the first step is the lipase-catalysed hydrolysis of triglycerides to glycerol and fatty acids |
|
|
In the preceding question, what enzyme is responsible for the correct initial step in triglyceride analysis to occur?
a) Amylase b) Lipase c) Glycerase d) Esterase |
Lipase
|
|
|
The lipoprotein that contains mostly triglyceride in the fasting state is
a) chylomicron. b) VLDL. c) LDL. d) HDL. |
VLDL
Response Feedback: In the fasting state, most plasma triglycerides are present in VLDL. Chylomicrons, which also carry triglycerides, appear transiently in blood after a meal. |
|
|
In a direct method of HDL cholesterol analysis, the initial step would involve
a) hydrolysis of cholesterol esters by cholesterol oxidase to form free cholesterol. b) hydrolysis of cholesterol esters by lipase to form glycerol and free fatty acids. c) precipitation of non-HDL lipoproteins. d) measurement of the rate of oxygen consumption |
precipitation of non-HDL lipoproteins.
Response Feedback: After the non-HDL lipoproteins are first physically removed by precipitation or are effectively masked, total cholesterol is then measured to give a concentration of HDL cholesterol. |
|
|
Which apolipoprotein is affected in dysbetalipoproteinaemia?
a) Apo B-100 b) Apo A1 c) Apo CII d) Apo E |
Apo E present on the surface of lipoprotein remnant particles interacts with specific hepatic receptors and facilitates the removal of lipoprotein remnant particles. Homozygosity for the apo E2 form does not effectively remove these particles.
|
|
|
What is the specific result of dysbetalipoproteinaemia?
a) Loss of the reverse-cholesterol transport pathway, which involves the efflux of cholesterol from cells b) Defective removal of lipoprotein remnants from both chylomicrons and VLDL c) Increased LDL accumulation with proportional HDL decrease in the plasma d) Decreased lipoprotein lipase activity with concomitant decreased removal of VLDL |
Defective removal of lipoprotein remnants from both chylomicrons and VLDL
Response Feedback: Dysbetalipoproteinemia, also termed type III hyperlipoproteinemia, is caused by a defect in the removal of lipoprotein remnants from both chylomicrons and VLDL. Some individuals with dysbetalipoproteinemia are homozygous for the apo E2 isoform, which does not efficiently bind to hepatic remnant receptors. |
|
|
The protein component of a lipoprotein is referred to as a(n)
a) terpene. b) apolipoprotein. c) prostaglandin. d) phospholipid. |
apolipoprotein
Response Feedback: Definition: an apolipoprotein is any of the protein constituents of lipoproteins. |
|
|
What distinguishes lipoprotein(a), or Lp(a), from LDL?
a) Lp(a) contains more core lipids, triglyceride and cholesteryl ester, and a smaller percent of protein. b) Lp(a) interacts with ABCA1 in peripheral cells, such as the macrophages, to remove additional cholesterol. c) Lp(a) contains a carbohydrate-rich protein called apo(a) that is covalently bound to apo B-100 through a disulfide linkage. d) Lp(a) does not contain any apo B-100 |
Lp(a) contains a carbohydrate-rich protein called apo(a) that is covalently bound to apo B-100 through a disulfide linkage.
Response Feedback: Lp(a) is structurally related to LDL because both lipoproteins possess one molecule of apo B-100 per particle and have similar lipid compositions. However, unlike LDL, Lp(a) also contains a carbohydrate-rich protein [apo(a)] that is covalently bound to the apo B-100 through a disulfide linkage. |
|
|
A 4-year-old girl has oedema that is most obvious around her ankles and in her eyelids. She has yellow spots on her palms.
Her laboratory findings reveal (reference intervals are in parentheses): serum albumin 18 g/L (35 to 55 g/L), total serum cholesterol 9.1 mmol/L(<4.5 mmol/L), LDL cholesterol 3.6 mmol/L (<2.5 mmol/L), serum urea 7.1 mmol/L (2.5 to 6.5 mmol/L), urine protein by dipstick: 4+ (negative), and urine blood by dipstick: negative (negative). All other values were normal. These findings are most compatible with a) acute poststreptococcal glomerulonephritis with dysbetalipoproteinaemia. b) nephrotic syndrome with secondary hyperlipidaemia. c) acute pyelonephritis and familial hypercholesterolemia. d) mild glomerular disease with lipoprotein lipase deficiency |
nephrotic syndrome with secondary hyperlipidaemia.
The decreased serum albumin and increased urea are common in renal disorders, but the cholesterol values and symptoms indicate a hyperlipidaemia that is present as well. A renal cause of hyperlipidemia is nephrotic syndrome. |
|
|
The hyperlipoproteinaemia that is observed in familial combined hyperlipidaemia (FCHL) that has elevated total and LDL cholesterol and normal triglycerides is type:
a) IIA. b) IIB. c) IV. d) V. |
IIA.
Response Feedback: Families with FCHL often have increased plasma concentrations of total and LDL cholesterol (type IIa) while apo B-100 concentrations are increased. |
|
|
An overweight 35-year-old man comes to his physician with palmar xanthomas and pain in his lower extremities. Results of
a lipid profile indicated values for both HDL and LDL were below the reference interval, whilst total cholesterol and Triglycerides were elevated. What disease might be the cause of these symptoms and lipid results? a) Familial hypercholesterolemia b) Tangier disease c) Dysbetalipoproteinaemia d) Decreased lipoprotein lipase activity |
Dysbetalipoproteinaemia
Response Feedback: The most distinctive clinical feature of dysbetalipoproteinemia is the presence of palmar xanthomas. Both LDL and HDL cholesterol are lower than normal in these individuals and premature atherosclerosis commonly develops, particularly in the lower extremities. |
|
|
(SN) The basis of the routinely performed assays to measure total cholesterol.
|
**
|
|
|
Describe Secondary Lipidaemia
|
Alcohol
- alcohol is straight to the liver and stored as fat Overweight & obese Diabetes - Secondary hyperlipidaemia - high TG, low HDL - insulin resistance -high Chylomicrons and VLDLs in their blood. - elevated levels of Lipoprotein (a) in their blood --> higher risk of atherosclerotic disorders forming Hypothyroidism - increase in lipid levels Nephrotic syndrome - Basement membrane has charge - larger medium MW is lost to the urine - Larger MW is retained - more albumin and proteins is produced - more lipoproteins are produced - decrease in albumin - increase in lipoprotein Obstructive Liver Disease - high bile means more cholesterol in the blood. Chronic Renal Failure - same as nephrotic syndrome. |
|
|
Describe alcohol abuse as a cause of secondary lipidaemia
|
- alcohol is straight to the liver and stored as fat
|
|
|
Describe hypothyroidism as a 2'of lipidaemia
|
increased production of lipoproteins
|
|
|
Describe nephrotic syndrome as a 2'cause of lipidemia
|
Basement membrane has charge
larger medium MW is lost to the urine Larger MW is retained more albumin and proteins is produced more lipoproteins are produced decrease in albumin increase in lipoprotein |
|
|
Describe obstructive liver disease as a 2' lipidemia
|
high bile means more cholesterol in the blood.
|
|
|
Describe Chronic renal failure as 2' lipidemia
|
Basement membrane has charge
larger medium MW is lost to the urine Larger MW is retained more albumin and proteins is produced more lipoproteins are produced decrease in albumin increase in lipoprotein |
|
|
Describe primary lipidemias from secondary lipidemias
|
**
|
|
|
List primary hyperlipidaemias
|
DH FFF AA
- Dysbeta lipoproteinemia - Hypertriglycerideridemia - Familial cholesterolaemia - Familial Ligand - Defective ApoB -100 - Familial Hypobetalipoproteinaemia - Abetalipoproteinemia - Analphalipoproteinemia |

