![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
83 Cards in this Set
- Front
- Back
|
What condition can BPH lead to? |
Prostatitis |
|
|
What is the active ingredient in ypozane and how does it work? |
Osaterone. Testosterone analogue. |
|
|
2 possible adverse reactions of using ypozane? |
Elevation of liver enzymes. Patients with Addison’s can have a crisis due to reduction in cortisol |
|
|
Why are progesterone synthetic analogues no longer recommended for treatment of BPH? |
Can increase chance of squamous cell metaplasia and decrease quality of semen. Also increase risk of DM and mammary hyperplasia |
|
|
What are paraprostatic cysts? |
Cysts hat develop close to the prostate but not directly associated with it. Remnants of the Muller ducts. |
|
|
How would you treat paraprostatic cysts? 2 And when would you need to? |
If they were so enlarged they were causing urinary obstruction or infection. Surgical treatment and castration |
|
|
Do you tend to see prostatitis in entire or neutered males? |
Entire |
|
|
Is urine culture beneficial in cases of prostatic disease? |
Can be a reasonable estimate of infectious agent but discordant results are possible |
|
|
How does antibiotic therapy differ in cases of acute versus chronic prostatitis? |
Acute- the blood prostate barrier not intact so go off culture and sensitivity for 4 weeks. Chronic- go for TMPS, fluoroquinolones that have good penetration. Enrofloxacin and Marbofloxacin in first line for 4-6 weeks |
|
|
When should you castrate a dog with prostatitis? |
After a negative culture of urine or prostatic fluid is obtained, dog remains on antibiotics |
|
|
What is the recommended treatment for prostatic abscesses? |
Omentalisatiom |
|
|
What staging should be performed is prostatic neoplasia is suspected? |
Rads of lumbar vertebrae, lungs Ultrasound of iliac lymph nodes and bladder/ urethra |
|
|
Treatment for prostatic neoplasia? 3 |
Surgery- not usually indicated and can cause incontinence Chemo- partial and short term response Palliative- piroxicam +\- chemo may improve QOL |
|
|
Sporadic bacterial cystitis recommended tx |
3-5 days amoxicillin |
|
|
Sporadic bacterial cystitis recommended tx |
3-5 days amoxicillin |
|
|
Treatment course length for re-infection cystitis |
3-5 days |
|
|
Treatment course length for relapsing/ persistent UTIs |
7-14 days |
|
|
What is polypoid cystitis? Which bacteria can predispose? Treatment of? |
Sequelae of chronic UTIs leading to proliferation of intra mural mucosa which can predispose to further utis Proteus Antibiotics and surgery |
|
|
What is emphysematous cystitis? |
Presence of gas within bladder wall an lumen associated with infection with glucose fermenting bacteria. Usually underlying diabetes |
|
|
What is encrusted cystitis and what has it been associated with? Treatment |
Urease positive bacteria eg corynebacterium forms mineralised plaques on mucosa Surgical debridement |
|
|
Diagnosis of pyelonephritis? |
Definitive pyelocentesis Positive cysto sample and c/s and imaging is often used |
|
|
Antibiotics for pyelonephritis? Length of course |
Enrofloxacin (dogs) or marblfloxacin (dogs/ cats) doe 10-14 days pending culture |
|
|
Antibiotics for pyelonephritis? Length of course |
Enrofloxacin (dogs) or marblfloxacin (dogs/ cats) doe 10-14 days pending culture |
|
|
5 ecg findings usually seen with hyperkalemia |
Peaked t waves Diminished or Absent p waves Widened pr interval Widened QRS complex V tach |
|
|
What is the definition of a mixed urolith? |
<70% of a single mineral |
|
|
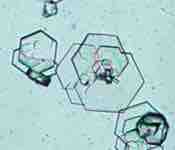
The detection of which 3 crystal types should prompt further investigation? |
Urate, xanthine and cystine |
|
|
How can you tell what Urolith is present? |
Educated guess based on breed, urine pH, location of Urolith, radiopaque/ lucent, crystals |
|
|
Which 3 uroliths are amenable to dissolution? |
Structure, cystine and urate |
|
|
How can you prevent struvite stone formation? |
Diet low in magnesium and phosphorus, acidifying |
|
|
How can you prevent struvite stone formation? |
Diet low in magnesium and phosphorus, acidifying |
|
|
How to minimise calcium oxalate recurrence? 3 |
Prevent acidifying or over concentration the urine Avoid diets with excess protein |
|
|
How to prevent urate Urolith recurrence? 2 |
Diet Consider xanthine oxidase inhibitors for dogs homozygous for genetic hyperuricosuria |
|
|
Why can extracorpeal shockwave lithotripsy not be used in cats? |
High risk of urethral obstruction with the fragments and calcium oxalate uroliths are resistant to fragmentation |
|
|
What is the most common feline nephrolith? |
92% calcium oxalate |
|
|
Ureterolith method of diagnosis? |
Ultrasound usually Rads may help but can’t see them all Contrast CT |
|
|
Medical management of ureterolith? |
Imaging alongside fluid therapy, diuretics and prazosin as long as no renal disease, infection or progression of ureteral dilation for 24-48 hours |
|
|
Could you consider dissolution of a struvite ureterolith? |
Not without placement of a stent due to risk of pyonephrosis and Uroabdomen |
|
|
How soon can medical dissolution of infection- induced structure uroliths occur? How long should you continue therapy for? |
Usually 3 months. Improvement in clinical signs in 1-2 weeks. Therapy should be continued for another 4 weeks beyond radiological resolution |
|
|
Risk of long term struvite diets? |
Calcium oxalate formation |
|
|
Recurrence rate of calcium oxalate stones? |
50% in 2 years despite preventative measures |
|
|
2 causes of canine urate uroliths |
Hepatic vascular abnormality Inherited abnormalities of the urate transporter |
|
|
Causes of cystine uroliths |
Problems with renal tubular transport of cystine |
|
|
Predisposition to cystine uroliths and therefore consideration for tx |
Male dogs 98% Castration can be part of tx |
|
|
When is voided urohydropropulsion considered? |
Female cats with uroliths no bigger than 2-3mm |
|
|
Treatment of struvite urolithiasis in cats |
Dissolution Not antibiotics unless documented uti as very rare |
|
|
2 relaxants of smooth muscle |
Prazosin Phenoxybenzamine |
|
|
Relaxant of skeletal muscle |
Dantrolene |
|
|
Location is TCC in cats? |
Variable, trigone location in only 27% |
|
|
Location is TCC in cats? |
Variable, trigone location in only 27% |
|
|
Limitations of bladder tumour antigen test? |
False positives with haematuria, proteinuria or glucosuria |
|
|
Chances of metastasis of bladder TCC? |
40% of dogs at presentation 20% of cats |
|
|
Treatment for bladder TCC in dogs? |
Piroxicam +/- carboplatin or mitoxantrone Tube cystotomy or stenting |
|
|
3 nerves involved in bladder control |
Pelvic Hypogastric Pudendal |
|
|
How common is incontinence in cats? |
Very rare |
|
|
Most common 2 causes of feline in continence? |
Congenital Spinal cord disease |
|
|
How does oestriol work? adverse reactions- 1 female, 1 male and 1 both |
Increases number and sensitivity of oestrogen receptors in the urinary sphincter Mammary and vulvar swelling Bone marrow suppression at high doses In males prostatic metaplasia |
|
|
Method of action of phenylpropanolamine |
Alpha agonist drug- Stimulates oestrogen receptors |
|
|
Side effects of propalin |
Behavioural- restless or aggressive GI problems Arterial hypertension |
|
|
Side effects of propalin-3 |
Behavioural- restless or aggressive GI problems Arterial hypertension |
|
|
Medication for male dogs and cats incontinence |
Propalin |
|
|
Which drug can be used to stimulate detrusor contraction? |
Betanechol |
|
|
2 characteristics of overactive bladder |
Good urine steam Urge to urinate |
|
|
2 meds for overactive bladder |
Oxybutinin Tricyclic antidepressants |
|
|
If a large breed Middle Ages male dog presented with incomplete bladder emptying, urine flow stops sudenly and occasional overflow incontinence, what may be considered? |
Detrusor- urethral dissynergy |
|
|
If a large breed Middle Ages male dog presented with incomplete bladder emptying, urine flow stops sudenly and occasional overflow incontinence, what may be considered? |
Detrusor- urethral dissynergy |
|
|
Detrusor- urethral dissynergy medications that may help? |
Prazosin Pheoxybenzamine Dantrolene |
|
|
Tx of UMn bladder |
Depends on underlying course Catheterise bladder to maintain small size and prevent overdistension |
|
|
How can you diagnose intra-pelvic bladder? |
Make sure bladder is full prior to x ray |
|
|
What is a persistent urachus? |
Leakage of urine through the umbilicus when the canal remains patent |
|
|
Urachal diverticulae can be an important differential in what situation? |
Cats with lower urinary tract problems eg recurrent uti |
|
|
How do you diagnose a urachal diverticulum? 3 |
Radiographic contrast, ultrasound or cystoscopy |
|
|
Difference between intramural and extramural ureters? |
Extramural enter the lower urinary tract at the level of the urethra, vagina or vestibule in females or in the ductus deferens in male Intramural can join at the level of the trigone that opens into the bladder linen after a longer intramural trajectory usually on the distal urethra |
|
|
Average age of diagnosis ectopic ureters? |
Females 10 months Males 24 months |
|
|
Clinical signs of ectopic ureters? |
Incontinence Possible utis |
|
|
What should be remembered when diagnosing ectopic ureters? |
Other developmental abnormalities are very common |
|
|
Treatment of ectopic ureters? |
Surgical or laser Medical tx post surgery often still necessary |
|
|
What is polypoid cystitis? |
Proteus Chronic UTIs can lead to proliferation of the mucosa resulting in diffuse or focal thickening of the bladder mucosa |
|
|
What 2 bacteria can cause struvite urolithiasis? |
Proteus Staph |
|
Front (Term) |
Urate |
|
Type and cause. What sex is more affected? |
Cystine Renal tubular transport possibly inherited 98% males |
|
|
What characterises fanconi syndrome? |
Progressive loss of electrolytes most notably glucose into urine resulting in pu/pd due to a renal tubular defect |
|
|
What characterises fanconi syndrome? |
Progressive loss of electrolytes most notably glucose into urine resulting in pu/pd due to a renal tubular defect |
|
|
What causes fanconi syndrome? |
Renal tubular defect Congenital in the basenji Acquires to to jerky treats, gentamicin used or idiopathic |

