![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Myogenic
|
Myocyte contraction that originates from the myocyte itself
|
|
|
How are signals conducted in myocytes?
|
Gap junctions
|
|
|
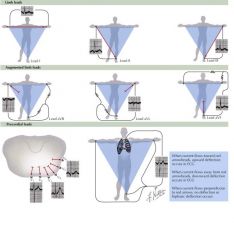
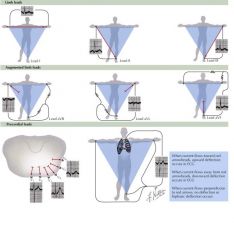
If the electrical wave is passing towards the positive electrode in what direction does the tracing deflect?
|
Upward
|
|
|
If the electrical wave is passing towards the positive negative in what direction does the tracing deflect?
|
Downward
|
|
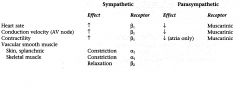
Sympathetic Effects on HR
|
NE release at sympahtetic ending
Causes increased sinus node discharge Increases rate of conduction of impulse Increases force of contraction in atria and ventricles |
|
|
Parasympathetic Effects on HR
|
Vagal nerves release ACh; innervate SA node and AV junctional fibers proximal to AV node
Cause hyperpolarization bc of increase K permeability in response to acetylcholine which causes a decreased transmission of impulses Hyperpolarize the cell via increasing potassium conductance in SA nodal cells. Thus, it takes longer to reach threshold and the intrinsic firing rate decreases; there may also be a decrease in the slope of the prepotential |
|
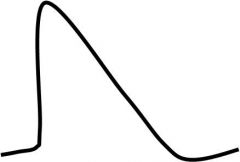
Which cardiac action potential does this describe?
|
AP at the SA node
|
|
Which cardiac AP does this describe?
|
Ventricular action potential
|
|
|
Describe the cardiac conduction pathway
|
SA node -> atrial muscle -> AV node (delay) -> Purkinje fibers -> ventricular muscle
|
|
|
What is the fastest cardiac conducting fiber?
|
Purkinje Cell
|
|
|
What is the slowest conducting fiber?
|
AV node
|
|
|
Where are gap junctions located on caradiac cells?
|
intercalated disks
|
|
|
what is a unique contracticle feature of cardiac cells?
|
require extracellular calcium to replace depleted intracellular from SR
|
|
|
Is there summation in muscle contraction?
|
NO; this allows for orderly blood flow
There is a long refractory period so a secondary contraction can't sum on top of the first; thus the heart won't tetanize |
|
|
T tubules in cardiac muscle compared to skeletal muscle
|
T tubules are 25x larger in cardiac muscle
|
|
|
What is the correlation between extracellular calcium concentration and strength of the contraction
|
Direct relationship;
|
|
|
What happens to calcium after a contraction?
|
Cytosolic calcium is pumped out of the cardiac muscle into the t-tubule, a small amount is pumped back into the SR
|
|
|
Describe actin based regulation of contraction
|
Calcium binds troponin to move the troomyosin off of the actin filament to allow actin and myosin to bind/crossbridge cycle
|
|
|
How is the length tension curve in cardiac muscle different from skeletal
|
In skeletal, increasing sacromere length (stretching the muscle) too far ends up decreasing muscle tension past an optimal point
In cardiac muscle, a connective tissue skeleton prevents cardiac sarcomeres from overlengthening; if the heart overfills and reaches its limit of stretching, there will be an increase in blood pressure (but NOT a lack of blood flow) |
|
|
Effects of Sympathetics
|
Slope of prepotential increases; threshold is reached sooner; the intrinsic firing rate increases (via increased calcium conductance of nodal fibers)
|
|
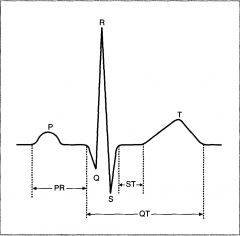
P Wave?
|
Represents atrial depolaization
Does not include atrial repolarization, which is 'buried' in the QRS complex |
|
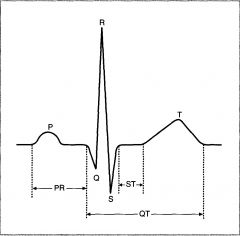
PR interval?
|
Is th einterval from the beginning of the P wave to the beginning of hte Q wave (initial depolarization of the ventricle)
varies w/ CONDUCTION VELOCITY THROUGH AV NODE (if AV nodal conduction decreases the PR interval increases) Is decreased by sympathetic stimulation Is increased by parasympathetic stimulation |
|
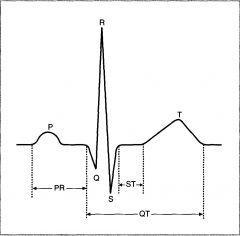
QRS complex?
|
Represents depolarization of the ventricles
|
|
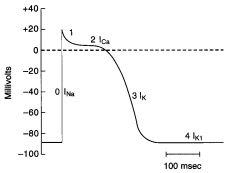
Phase 0
|
Upstroke of the AP
rapid Na influx depolarizes membrane At the peak of the AP, the membrane potential approaches the Na equilibrium potential |
|
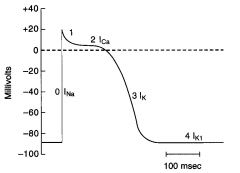
Phase 1
|
Initial repolarization; part bc of K+ ions move outward and a decrease in Na+ conductance
|
|
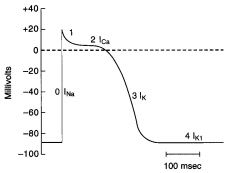
Phase 2
|
Plataeu of the action potential
Caused by a transient increase in Ca2+ conductance = inward Ca+ current During phase 2 outward and inward currents are approximately equal, so the membrane potential is stable at the plateau level |
|
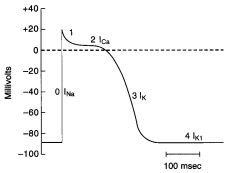
Phase 3
|
Repolarization
Ca2+ conductance decreases and K+ conductance increases and predominates The high K+ conductance results in large OUTWARD K+ current (Ik) which hyperpolarizes the membrane back toward the K+ equilibrium potential |
|
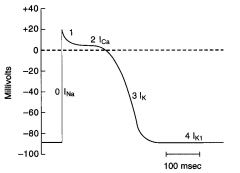
Phase 4
|
Resting membrane potential
Inward/outward currents (Ik1) are equal and the membrane potential approaches the K+ equilibrium potential |
|
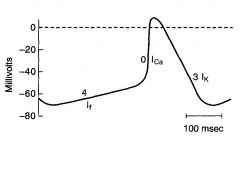
Phase 0
|
Upstroke
Inward Ca2+ current; drives membrane potential towards Ca+ equilibrium potential Note: ionic basis for phase 0 in the SA node is diff from that in ventricles, atria and purkinje fibers (where it is due to Na current) |
|
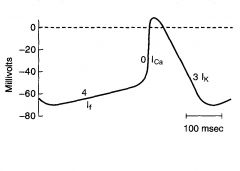
Phase 3
|
Repolarization
Outward K current |
|
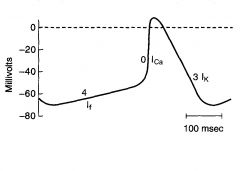
Phsae 4
|
Slow depolarization
Accounts for pacemaker activity of the SA node (automaticity) Increase in Na conductance, which results in an inward Na current called If If is turned on by repolarization of the membrane potential during the preceding action potential |
|
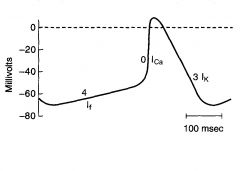
Phase 1 and 2?
|
Not present in the SA node action potential
|
|
|
Where is conduction velocity fastest?
|
in the Purkinje system
|
|
|
Where is conduction velocity slowest?
|
In the AV node (seen as the PR interval on the ECG); allows time for ventricular filling before ventricular contraction
if conduction through AV node is increased, ventricle filling may be compromised |
|
|
Einthoven's Law
|
I + III = II
If the electrical potential of any two leads is known the potential of the third can be determined |
|
|
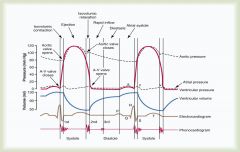
Cardiac Cycle; know it
|
|
|
Systole
|
Heart squeezing blood out; increases pressure in the arterial system
|
|
|
Diastole
|
Heart relaxes and refills; pressure decreases during this time bc the heart isn't pushing any blood into the system
|
|
|
Wave perpendicular to ECG vector
|
no deflection
|
|
|
Wave moving away from ECG vector
|
Needle moves down; moves down less if wave is moving away at an angle
|
|
|
Wave moving in the same direction from ECG vector
|
Needle moves up; moves less if wave is moving with it at an angle
|
|
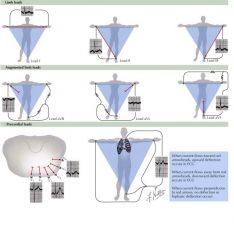
Right shoulder negative -> left shoulder positive
|
Lead I; since vector is down and to the left you get a smaller positive PQRS complex
|
|
Right shoulder negative -> left leg as positive
|
Lead II; depolarization vector parallel so large positive PQRS complex
|
|
Right shoudler negative -> right leg positive
|
Lead III; wve of depolarization almost perpendicular but still aligned so decrease PQRS complex
|
|
|
Which precordial leads are considered the septal leads (record heart activity from septum)
|

V1 and V2
|
|
|
Which precordial leads capture the anterior wall of the heart, and which is the apical lead?
|

V2, V3, V4
V4 is considered the apical lead |
|
|
Which precordial leads are considered the lateral leads which give a view of the sidewall of the heart?
|

V4, V5, V6
|
|
|
What does the left main coronary give rise to?
|
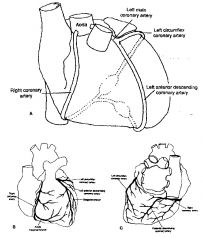
LLC
LAD |
|
|
What does the right coronary give rise to
|
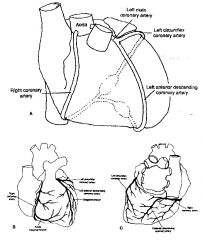
Posterior Descending Coronary Artery; supplies the inferior posterior portion of the heart
|
|
|
Which leads view the bottom of the heart?
|
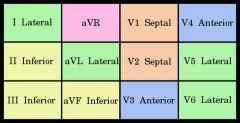
|
|
|
Which leads view the antero-septal wall, supplied by the LAD?
|
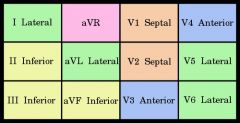
|
|
|
What does the LLC give rise to?
|
Obtuse marginal branch; supplies lateral wall
|
|
|
Which leads view the lateral wall?
|
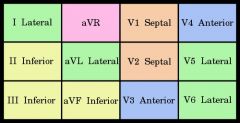
V5, V6 (low lateral)
I, aVL (high lateral) |
|
|
Myocardial infarction
|
Type of IHD; ischemia causes the death of heart muscle
|
|
|
Angina pectoris
|
Type of IHD; ischemia is of insufficient severity to cause infarction but may be a harbinger of MI
|
|
|
paroxysmal and usually recurrent attacks of substernal or precordial chest discomfort (variously described as constricting, squeezing, choking, or knifelike) caused by transient (15 seconds to 15 minutes) myocardial ischemia that falls short of inducing myocyte necrosis.
|
Angina pectoris (literally chest pain)
|
|
|
Stable Angina and EKG changes
|
Imbalance in coronary perfusion (due to chronic stenosis coronary atherosclerosis) relative to myocardial demand; relieved by rest and administering nitro
ST segent depression |
|
|
Retrosternal chest pain on exertion
|
Stable angina
|
|
|
ST segment depression
|
Stable angina
|
|
|
What causes prinzmetal/variant angina?
|
Coronary artery spasm; episodic myocardial ischemia
the anginal attacks are unrelated to physical activity, heart rate, or bp |

