![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
What are two main types of type IV hypersensitivity?
|
-delayed type hypersensitivity
-t-cell mediated hypersensitivity |
|
|
Do the type IV type hypersensitivity reactions involve antibodies?
|
NO
|
|
|
What is the cause of cell/tissue injury in type IV?
|
cell-mediated immune response with sensitized T lymphocytes
|
|
|
Describe the mechanism of a delayed type 4 hypersensitivity reaction?
|
-APC presenting cell releases IL12 and activates Th1 CD4 which secretes three types of cytokiens
-APC also releases IL21, that activates TH17 --> recruits neutrophils |
|
|
Describe the mechanism of a T-cell mediated hypersensitivity reaction:
|
CD8 directly kill cells
|
|
|
What are the two prototypes of DTH?
|
-Tuberculosis and contact dermatitis
|
|
|
Describe the host response to a tubercolosis infection.
|
-first exposure of mycobacterium tuberculosis: macrophages engulf mycobacteria but no succeed in eliminating
-MHC2 and release of IL12 -Th cell activate and release IL2, TNF, IFN-gamma |
|
|
Three major cytokines produced by TH1 and functions?
|
IFN: activate macrophages
TNF: leakky cells IL-2 activate itself / more TH1 |
|
|
With persistent AG like Myc tuberc, when is the initial perivascular lymphocytic infiltrate replaced by macrophages?
|
2-3 weeks
|
|
|
define a granuloma:
|
epitheloid cells (morphologically transformed macrophages) surrounded by rim of lymphocytes also containing giant cells
|
|
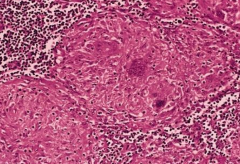
What is this?
|
Lymph node with several granulomas
|
|
|
how many weeks does it take to battle mycobacterium? how many weeks does it take to recruit macrophages and form granuloma/
|
3 weeks and 3 weeks
|
|
|
What does PPD stand for? What is another name for it -when does induration begin? when does the reaction peak?
|
-protein positive derivative or Mantoux
-begins 8-12 hours -peaks at 24-72 hours |
|
|
Give two cellular explanations to explain what is going on in a positive TB test:
|
1.) accumulation of mononuclear cells around small veins (perivascular cuffing)
2.) increased microvascular permeability --> escape of plasma proteins (dermal edema and deposition of fibrin) |
|
|
what is perivascular cuffing?
|
-accumulation of mononuclear cells (T lymphs CD4) around small veins and venules
|
|

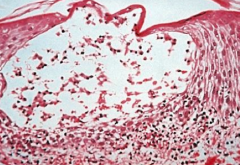
What is this?
|
immunoperoxidase staining showing perivascular cuffing
|
|
|
Why is the PPD test sometimes given as a two-step PPD?
|
-elderly person had exposure in the past and has waning reaction so negative TB test at first
-a repeat PPD 1-3 weeks after may result in a boosted reaction |
|
|
how many weeks later do you give the second PPD in a two step PPD?
|
1-3 weeks after first
|
|
|
What is contact dermatitis an example of?
|
type 4 delayed type hypersensitivity
|
|
|
What are haptens and give exampls of haptens
|
a hapten is a small molecule that can elicit an immune response only when attached to a large carrier such as a protein
1.) resins in poison ivy and oak 2.) metals such as nickel 3.) acetylates and chemicals in rubber |
|
|
-what is the antigen in poison ivy (also a type of hapten)
|
urshiol or catechol molecule
|
|
|
Why does no dermatitis result from primary contact?
|
-catechols are catabolized before sensitized T cells are produced (7-10 days produce memory cells though)
|
|
what happens during secondary contact with poison ivy? (explain the histopathology of this slide)
|
in 1-2 days, get dermatitis: Th1 cells accumulate and release cytokines that cause damage to keratinocytes; cause separation of these cells
|
|
|
T-cell mediated cytotoxicity plays a role in 4 different categories. list categories
|
-resistance to viral infections (hep b)
-tumor immunity -autoimmune diseases -graft versus host ; graft rejection |
|
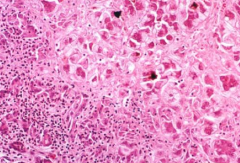
What is this and what accounts for the damage?
|
liver injury; HBV virus
-host immune response to viral AGs on infected hepatocytes leads to T-cell mediated cytotoxicity and tissue damage: |
|
|
Explain the role of type 4 sensitivity in type 1 diabetes. What is unique about this?
|
-both types of type 4: DTH and CT-mediated
-failure of self-tolerance in T cells -Damage to beta cells: 1.) Th1 cells by secreting IFN-gamma and TNF 2.) CD8 cells by directly killing Beta cells |
|
|
explain role of Type IV in MS. Is it mainly DTH or cytotoxic T-cell mediated type?
|
-mainly DTH
-TH1 and Th17 react against myelin antigens and secrete cytokines -Th1: IFN-gamma -Th17: recruitement of leukocytes |
|
|
evidence for TYPE IV in guillain bare and examples of preceding infections
|
evidence:
1.) transfer of T cells to animals: comparable lesions 2.) lymphocytes from individuals with GB: demyelination in tissue cultures of myelinated nerves preceding infections: influenza, campylobacter jejuni, CMV, EBV |
|
|
Graft versus host and Host versus graft plays role in T cell cytotoxicity? Where do we see GVH?
|
yes
-GVH in bone marrow transplants typically |
|
|
What are two mechanisms in T-cell mediated cytotoxicity?
|
FAS-FAS ligand and perforin/granyzme
|
|
|
explain the complications of hashimoto thyroiditis? What types of hypersensitivity reactions are involved? (there are 3)
|
-T-cell mediated cytotoxicity (fas-fass with CD*)
-thyrocyte injury (TH1 CD4 with IFN-gamma) -antibody dependent cell mediated cytotoxicity with N cells |

