![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
What are 3 other names of Type III hypersensitivity reactions?
|
-immune complex mediated
-indirect target -innocent bystander |
|
|
What is type III hypersensitivity a result of?
|
-formation of circulating antigen-antibody complexes that deposit in vessel walls and activate complement
|
|
|
Can Type III reactions form IC's that are both within circulation and in situ?
|
YES
|
|
|
What are three types of systemic TYPE III hypersensitivity reactions and 1 type of localized immune complex disease?
|
systemic: serum sickness, systemic lupus arythematosis, post-infectious (post-streptococcus glomerulonephritis)
local: Arthus reaction |
|
|
Describe the history of discovery of serum sickness:
|
Von pirquet in 1911 injected horse seru (horses exposed to diphtheria) into children; 10 days afterward found sickness in children from horse serum injected (whether horse was exposed or not exposed previously to diphtheria)
|
|
|
What clinical findings did Von Pirquet discover in children injected with horse serum? (4)
|
joint inflammation (arthritis and arthralgia); skin rash (urticaria); fever; glomerulonephritis
|
|
|
What caused these symptoms?
|
antigen-antibody deposition in vasculature
|
|
|
-When do IC's become deposited in tissues and cause disease?
|
-ICs produced in excessive amounts
-not efficiently cleared by phagocytic system |
|
|
What are three physicochemical properties of Ags and Abs that can determine the extent and location of IC deposition?
|
-charge, valence, and antibody avidity
-local vascular factors (filtering at high pressure; urine and synovial fluid) -affinity of Ag to tissue compartments |
|
|
What are two clinical outcomes for patients who developed serum sickness?
|
-acute serum sickness (if single large exposure the IC's are catabolized)
-chronic serum sickness: repeated or prolonged exposure to an antigen |
|
|
Describe the three phases in the pathogenesis of Type III hypersensitivity disease:
|
1.) Phase 1: immune complex formation
2.) Phase II: immune complex deposition via complement and Fc receptor-mediated leukocyte recruitment and activation 3.) Phase III: immune complex-mediated inflammation and tissue injury |
|
|
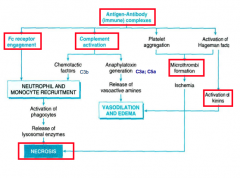
Reconstruct the robbins flow chart image of the pathogenesis of type III reactions:
|
|
|
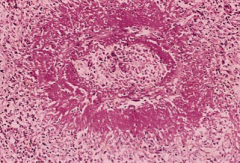
What is this a picture of? and what type of necrosis is it?
|
picture of immune complex vasculitis; necrotic vessel wall is replaced by smudgy, pink "fibrinoid" material: fibrinoid necrosis caused by protein deposition
|
|
|
deposition of IC in vessel wall leads to activation of ______ and recruitment of _____
|
complement, polys
|
|
|
What is SLE and what organs does it affect an in what age group/ sex?
|
systemic lupus erythematosis (SLE): chronic autoimmune inflammatory disease that affects every organ of the body;
-most prevalent in women from 16-64 years of age ; waxing and waning course |
|
|
What kind of antibodies does SLE make?
|
antinuclear antibodies
|
|
|
What two reasons explain the development of autoantibodies in SLE? What is the fundamental defect?
|
-susceptibility genes -> B an T cells specific for self-nuclear antigens
-external triggers (UV radiation ) --> defective clearance of apoptotic bodies and increased burden of nuclear antigens fundamental defect = failure of mechanisms that maintain self-tolerance |
|
|
What three factors may promote the development of ANA:
|
genetic factors; immunologic factors; environmental factors:
|
|
|
what are four categories of antinuclear antibodies and OTHER additional antibodies in SLE?
|
-antibodies to DNA, histones, non-histone proteins bound to RNA, nucleolar antigens
-others: against RBC, WBC, platelets; and antiphospholipid antibodies produced in 40-50% of patients with SLE |
|
|
what is the principle screening test for SLE? How sensitive and specific is it? What antibodies are SPECIFIC for SLE?
|
positive ANA lab test: 95% sensitive but not specific because 5-15 of healthy people have positive ANA
-antibodies to DS DNA and anti-smith ABS (small nuclear ribosomal Ag = specific for SLE) |
|
|
give four sample clinical manifestations of SLE:
|
1.) skin rashes, arthritis, glomerulonephritis and CNS involvement
|
|
|
What is the most commonly involved visceral organ in SLE?
|
kidney (50% patients develop renal disease)
|
|
|
What is difference between glomerulonephritis in Goodpasture's vs SLE?
|
in SLE, antibody deposits along the glomerulus not specific whereas for Goodpasture's, the complexes is specific to the basement membrane collagen type IV
|
|
|
Give two other systemic immune complex diseases not already mentioned:
|
1.) poststrep glomerulonephritis
2.) polyarthritis nodosa with viral hepatitis |
|
|
describe classic scenario of post-strep glomerulonephritis (clinical presentation, time of appearance, labs, kidney appearance)
|
-malaise, nausea, oliguria, hematuria, proteinuria 1-4 weeks after strep infection
-occurs only in nephritogenic strains -immune complexes may be circulating or antigen may be planted -low complement lab levels and granular deposits of IgG on the GBM |
|
|
When does post-infectious polyarteritis nodosa occur and in what age group?
|
-occurs following infection with Hep B or C virus infection; systemic vasculitis of medium size arteries
-average of of 40; |
|
|
What is the treatment of post-infectious polyarteritis nodosa and what happens if no treatment occurs?
|
-immunosuppressive treatment
-if no treatment, death in 2-5 years |
|
|
What is the Arthus reaction and when does it occur/peak? Give example of type of reaction.
|
-it is a localized area of tissue necrosis resulting from acute immune complex vasculitis
-peaks 4-10 hours after injection -example is a tetanus booster |

