![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
679 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Tremorgenic mycotoxins
|
-20 mycotoxins are tremorgens
-Most are associated with Penicillium species -Toxins are Penitrem A and roquefortine C -Intoxications occur in cattle, dogs, sheep, rappits, rodents, poultry |
|
|
|
Mechanism of Action for Tremorgenic mycotoxins
|
-Can vary between specific toxins and individual susceptibilities in species
-Penitrem-A inhibits glycine (inhibitory NT) in mice -Verruculogen decreases GABA concentrations in the brain |
|
|
|
Tremorgenic Mycotoxin Toxicities Diagnosis
|
-Submit sample of suspicious food or stomach contents for analysis
-Convulsants screen --penitrem A --roquefortine C --strychnine |
|
|
|
Tremorgenic Mycotoxin Treatment
|
-Diazepam to control seizures
--alone may not effectively control mycotoxin-induced tremors and seizures -Methocarbamol for severe tremors -Severe seizures not responding to diazepam, give barbiturate IV to effect |
|
|
|
Tremorgenic Mycotoxin Decontamination
|
-gastric lavage in patients that have not already vomited
-Treat for shock -IV fluid support -Prognosis is good with early and aggressive treatment -No long-term sequelae are expected |
|
|
|
Toxicology
|
-Exploring mechanisms by which chemicals produce adverse effects
-Apply safety evaluation and risk assessment -Uses basic science and direct applications at the same time -Originated in animal venom and plant extracts for hunting, warfare, assassinations |
|
|
|
Dose Response Relationship
|
-There is some measurable effect proportional to the amount of chemical received
-Experiments are needed to determine different responses to chemicals -Differentiation between therapeutic and toxic responses -May be distinguishable by the dose only -Can determine degree of specificity to therapeutic or toxic effect |
|
|
|
Percival Pott
|
-Connection between occupational hazards and diseases
-Chimney sweeps and scrotal cancer |
|
|
|
Federal Insecticide, Fungicide, and Rodenticide Act
FIFRA |
-Non-food, non-drug substances have to be safe and efficacious
-Flea and tick treatments have to be safe and efficacious -Act has been changed as recently as 2011 --make rodenticides safer, limit products that can be used around residences |
|
|
|
Delaney Clause
|
-Added amendment to the Food, Drug, and Cosmetic Act
-Any chemical found to be carcinogenic cannot be added to the food supply - |
|
|
|
Thalidomide
|
-Caused birth defects in the 1960s
-Given for nausea to pregnant women -Now given as treatment for lepers |
|
|
|
Recent Toxicology in the News
|
-Pet food contaminants
-Aflatoxins -Melamine and cyanuric acid -Elevated Ca levels in chicken and turkey feed |
|
|
|
Toxicant
|
-Alternate term for poison
-Any agent capable of producing a deleterious response in a biological system |
|
|
|
Toxin
|
-Poison that originates from a biological process
-Biotoxin -Has come from an animal or a plant |
|
|
|
Toxicity
|
-Quantity or amount that causes a toxic effect
|
|
|
|
Toxicosis
|
-Disease state that results from exposure to a poison
|
|
|
|
Hazard or Risk
|
-Liklihood that a chemical or drug will cause harm under certain conditions
|
|
|
|
Dose
|
-Amount of toxicant received per animal
-Total finite amount |
|
|
|
Dosage
|
-Amount of toxicant per unit of animal mass or body weight
-How medications are generally given |
|
|
|
Route of exposure
|
-Most commonly inhalation, PO, or derma
|
|
|
|
Threshold Dose
|
-Highest dose of toxicant at which toxic effects are not observed
-Point at which something becomes dangerous |
|
|
|
LD50
|
-Lethal Dose 50%
-The dose at which 50% of the animals die -Median Lethal Dose -Different compounds/toxicants have different LD50 |
|
|
|
NOEL
NOAEL |
NOEL: No Observed Effect Level
NOAEL: No observed adverse effect level -see change, but not an adverse change |
|
|
|
LOEL
|
LOEL: Lowest observed effect level
LOAEL: Lowest observed adverse effect level |
|
|
|
Therapeutic Index
|
-LD50/ED50
-Compares lethal dose to effective dose -Characterizes relative safety -Larger the therapeutic index, the more safe a chemical is |
|
|
|
Standard Safety margin
|
-LD1/ED99
-Characterizes relative safety -larger standard safety margin is safer -Bigger difference between lethal dose and effective dose |
|
|
|
Duration of Exposure
|
-Acute: single or multiple doses during a 24-hour period
-Sub-acute: multiple doses over more than 24 hours, for as long as 30 days -Sub-chronic: exposure for 1-3 months -Chronic: 3 months of exposure or longer A chemical that produces severe effects with a single dose may have no effects if the same total dose is given as multiple exposure over time |
|
|
|
Cause of Chronic toxic effects
|
-Chemical acumulates
-Toxic effects produced are irreversible -Insufficient recovery time between exposures |
|
|
|
Interaction of Chemicals
|
1. Additive effect: combined effect of 2 chemicals is equal to sum of each given alone
--2+3=5 2. Synergistic effects: combined effect of 2 chemicals is greater than the sum of each given alone --2+3=20 3. Potentiation: one otherwise non-toxic chemical becomes toxic when added to another chemical --0+2=20 4. Antagonism: 2 chemicals administered together interfere with the action of the other --4+0=1 --4+4=0 |
|
|
|
Assumptions of Dose-Response
|
1. Chemical interacts with a molecule or receptor site to produce a response
2. The production of the response or degree of the response is correlated to the concentration of the chemical at that receptor site 3. Concentration of the chemical at the site is related to the dose of the chemical received |
|
|
|
Hormesis
|
-Some xenobiotics impart beneficial or stimulatory effects at low doses, but have adverse effects at higher doses
-Ex: selenium, vitamin A -Necessary at one dose, toxic at a different dose |
|
|
|
Route of exposure and toxicity
|
-Route of exposure may determine the target organ
-Cadmium PO causes renal lesions --Inhalation goes to lungs first, eventually causes kidney issues --dermal exposure produces little if any toxicity |
|
|
|
Selective Toxicity
|
-Injury is produced in one tissue or organism and not another
-Ex: pesticide sand sulfonamides |
|
|
|
Interspecies differences to Toxoids
|
-Species have differences in intensity of toxic response
-Affected target organ can also differ -Cats have limited glucuronidation capability --rely on less-efficient metabolism pathways --sulfate and cysteine conjugation pathways |
|
|
|
Gender and Reproductive status differences with Toxoids
|
-Testosterone: increases rates of metabolism
--can be good if clears system from toxin --can be bad if metabolism increases concentration of toxic metabolite -Pregnancy and lactation cause hormonal and metabolic changes --affect mother and offspring |
|
|
|
Young animal susceptibility to Toxoids
|
-GI mucosa and BBB are less developed, less of a barrier
-Drug-metabolizing enzymes are generally less active -Higher proportions of body water -Lower proportion of body fat -Differences in distribution and storage of drugs and chemicals |
|
|
|
Pre-existing conditions and toxoids
|
-Liver diseases, results in fewer protective binding molecules
-Kidney disease can alter excretion and secretion capabilities -GI disease can reduce or enhance absorption |
|
|
|
Toxicokinetics
|
-Applying pharmacokinetics to determine the relationship between exposure and toxicity
-Absorption -Distribution -Metabolism -Excretion |
|
|
|
Absorption
|
-Chemical is transferred from the site of exposure into systemic circulation
-Has to get into systemic circulation |
|
|
|
Routes of Exposure
|
-Oral
-Inhalation -Dermal |
|
|
|
Inhalation Exposure
|
-Inhaling toxoid
-Some absorption can occur in the nasal passages before the chemical reaches the trachea, bronchi, and alveoli -Chemicals that reach the alveoli enter the blood -Solubility of toxoid in blood depends on the blood/gas partition coefficient |
|
|
|
Oral Exposure
|
-Most common exposure in veterinary medicine
-Inhaled substances can also enter GI tract (tracheal migration) -Chemical can be destroyed or absorbed in the acid environment of the stomach (good thing) -In small intestine chemicals can also be degraded or absorbed into portal circulation -Large molecules bay be degraded in the large intestine and eliminated in feces |
|
|
|
Dermal Exposure
|
-Chemical must be in soluble form and able to penetrate the keratinized epidermis
-Eventually needs to reach blood vessel -Skin is a great barrier, keeps many things out |
|
|
|
Relative effectiveness of Routes of exposure
|
-IM
-Inhalation -Intraperitoneal -SQ -IM -Intradermal -PO -Dermal |
|
|
|
Passive Transport
|
-No energy expenditure
-Diffusion rate is proportional to the concentration gradient across a cell membrane -Non-saturable, cannot be saturated -Simple diffusion and filtration |
|
|
|
Simple diffusion
|
-Passive transport
-Way most chemicals pass through biological membranes -non-ionized molecules have greater lipid solubility --can traverse phospholipid bilayers easier than ionized/charged molecules -Higher Ratio of non-ionized:ionized particles, greater potential for membrane absorption across lipid membrane --More non-ionized particles, more diffusion across the membrane -Non-ionized particles can leave compartments |
|
|
|
Filtration
|
-Form of passive diffusion
-Water flowing in bulk across a porous membrane -Any solute small enough to pass through pores flows with water |
|
|
|
Active Transport
|
-Requires energy
-Generally moves things across concentration gradients -Saturable process, not driven by concentration gradients |
|
|
|
Facilitated Transport
|
-Uses energy
-Movement of solutes is along concentration gradient |
|
|
|
Bioavailability
|
-Quantity or percentage portion of total chemical that was absorbed and available to be processed
-For IV administration, F=100% --all of drug gets into bloodstream -For PO, rarely 100% absorption |
|
|
|
Distribution
|
-Rate at which chemicals leave the blood and enter organs and tissues
-Depends on rate of blood flow to the tissue or organ -Chemical's ability to pass through capillary endothelium is a factor -Physiochemical properties are also important (lipid solubility) -When toxicants are bound to plasma proteins, they do not cross capillary walls and are not distributed into extravascular space to to kidneys --only free drug is able to be filtered by kidneys |
|
|
|
Blood Brain Barrier and Toxicoids
|
-Prevents some toxicants from entering the CNS
-Only free, un-bound toxicants can equilibrate with the brain -increased lipid solubility enhances penetration to CNS -Ionized particles are less able to cross BBB -Capillary endothelial cells of CNS are tightly joined --few or no pores between cells -Cells have ATP-dependent Multi-drug resistant protein that pumps chemicals back into the blood -CNS capillaries are surrounded by glial cell processes (astrocytes), provides tight barrier -Protein concentration in CNS interstitial fluid is lower than that of other body fluids --limits movement of protein-bound water-insoluble compounds |
|
|
|
Volume of Distribution
|
-Volume of fluid that is needed to contain the amount of chemical in the body if concentration were equal to what is found in the blood
-Does drug hang around in the blood stream, or does it go into tissues -As chemical is biotransformed or excreted, more is released from storage sites |
|
|
|
Storage depots for Toxicoids
|
-Plasma proteins: albumin, transferrin, globulins, lipoproteins
-Live and kidney: concentrate more toxins than all other organs combined -Fat: especially store lipophilic toxicants -Bone: lead, fluoride, and radioactive strontium store in bone |
|
|
|
Ideal metabolic System
|
-Produces metabolites that are water soluble and can be excreted in urine/bile
-Metabolites are non-toxic -Enzymes used to produce metabolites have broad enough substrate specificity to handle any new substances that get into the body |
|
|
|
Phase I Metabolism
|
-Converts apolar, lipophilic chemicals into more polar and more hydrophilic metabolites
-Introduces or breaks off a functional group -Hydrolysis -Oxidation -Reduction |
|
|
|
Oxidizing enzymes
|
-Alcohol dehydrogenase
-Aldehyde dehydrogenase -Monoamine oxidase -Cytochrome P-450 |
|
|
|
Phase II Metabolism
|
-Conjugates chemicals or metabolites formed during phase I metabolism with a functional group
-Adding a functional group results in a BIG increase in water solubility -Glucuronidation (not in cats) -Sulfation -Amino acid conjugations -Acylations -Methylations |
|
|
|
Excretion of Toxicants
|
-removal in urine is most common route of excretion
-Chemicals/metabolites formed in the liver can be excreted in bile (then into feces) --Can also undergo enterohepatic re-circulation and be re-absorbed in the intestine -Exhalation -Milk excretion -CSF excretion -Sweat and Saliva -Toxicants distributed to the skin can be eliminated via normal skin sloughing |
|
|
|
1st order kinetics
|
-Most chemicals re eliminated via 1st order kinetics
-Rate of elimination is proportional to the amount of chemical in the body at that time -Non-saturable pathways -Amount eliminated is always the same proportion over time |
|
|
|
Zero order kinetics
|
-Elimination is through a saturable pathway
-At some point, only a fininte amount of chemical can be eliminated over a certain period of time |
|
|
|
Elimination Half-life
|
-Time required for chemical concentration to decrease by half
-With 1st order kinetics, half-life is constant and independent of dose --after 7 half-lives, 99% of chemical is eliminated -With zero order kinetics |
|
|
|
1 part per million equivalents
|
1ppm = 1 mg/kg
1ppm = 0.91 g/ton 1ppm = 1 ug/ml 1ppm = 0.0001% 1ppm = 1000 ppb 1ppm = 1,000,000 ppt |
|
|
|
1 oz equivalents
|
1 oz = 30g = 30 ml
|
|
|
|
Tsp and Tbs equivalents
|
1 tsp = 5 ml (2 mini marshmallows)
1 Tbs = 15 ml 2 Tbs = 1 oz = 30 ml (one large marshmallow) |
|
|
|
Top 10 common dog poisons
|
-Chocolate
-Rodenticides -Vitamins and minerals (vitamin D3, Iron) -NSAIDs -Cardiac medications -Cold and allergy medications -Antidepressants -Xylitol -Acetaminophen -Caffeine pills |
|
|
|
TOp 10 common cat poisons
|
-Topical spot-on insecticides
-Household cleaners -Antidepressants -Lilies -INsoluble oxalate plants -NSAIDs -Cold and flu medications -Glow sticks -ADD/ADHD medications -Rodenticides |
|
|
|
Information to obtain following toxicant exposure
|
-Full trade name of product
-Active and inert ingredients and concentrations -Amount and dilution of the product -Clinical signs or progression of disease -Any treatments administered |
|
|
|
Toxicant consultants
|
-ASPCA: $65 fee
-Pet Poison Hotline: $39 fee |
|
|
|
Decontamination Treatment Strategy
|
-Emesis, induce vomiting
-Gastric lavage -Activated charcoal -Cathartic -Enema |
|
|
|
General Toxicant Treatment strategies
|
-Decontamination
-GI protectants (H2 blockers, PG analogs, sucralfate) -Anti-emetics (5HT3 antagonistis) -Anti-epileptics (Benzodiazepines, barbiturates, anesthetics) -Muscle relaxants (methocarbamol) |
|
|
|
When to suspect a Toxin
|
-ANY TIME!
-Young, healthy animals with acute onset of signs -Otherwise healthy animal with acute organ failure -Exposure to hazard -Multiple animals with similar issues |
|
|
|
Organs most commonly affected by household hazards
|
-GI system
-CNS -Kidneys (acute renal failure) -Neuromuscular system |
|
|
|
Acids
|
-Cleaning agents, anti-rust products, pool sanitizers, car batteries
-Toxicity depends on concentration -Produce localized coagulative necrosis -IMMEDIATE severe pain --can prevent animal from getting too high of a dose -Can be oral, dermal, inhalation, ocular exposure |
|
|
|
Clinical signs of Acid Toxicity
|
-Clinical signs depend on route of exposure
-Oral exposure: vocalization, dysphagia, vomiting, abdominal pain, ulcerations -Dermal exposure: pain, ulcerations -Inhalation: dyspnea, edema, inflammation -Ocular: corneal ulcers |
|
|
|
Acid toxicity Treatment
|
-Dilute dilute dilute!
-DO NOT neutralize -Gastric lavage or induction of emesis are bad ideas --damage GI tract, cause further irritation -Activated charcoal is not effective -Supportive care is best -Strictures are possible, esophageal damage and scar tissue leading to stricture |
|
|
|
Alkali exposure
|
-NaOH, KOH, Ammonium hydroxide, potassium permanganate
-Drain openers, car washing detergents, alkaline batteries, toilet bowl cleaners, pool products, radiator cleaning agents -Cause rapid tissue liquefactive necrosis --melting of the tissue -Litlte pain initially, develops over 1-12 hours --animal can consume more of product initially -Can be oral, dermal, inhalant, ocular exposure |
|
|
|
Alkali exposure treatment
|
-Supportive care
-Do not induce vomiting -Do not do a gastric lavage |
|
|
|
Long-term risk of acid or alkali exposure
|
-Strictures
-Damage to esophagus or other area of GI tract and resultant scar tissue formation |
|
|
|
Chocolate as a Toxin
|
-Contains methylxanthines, stimulant medications
--caffeine and theobromine -Amount of drug in chocolate varies --white chocolate has least, cocoa powder has most -Can see clinical signs with doses far below LD50 -LD50= 100-300 mg/kg |
|
|
|
Methylxanthines
|
-Inhibit intracellular Ca sequestration
-Competitively antagonize cellular adenosine --causes vasoconstriction, tachycardia, CNS stimulation -Inhibit phosphodiesterase --accumulation of cAMP, enhances catecholamine effects |
|
|
|
Methylxanthine absorption
|
-VERY rapidly absorbed
-Within 30-60 minutes of ingestion animal will have absorbed toxins --caffeine is fast, theobromine is a little slower |
|
|
|
Methylxanthine Effects
|
-Stimulatory effects
-Stimualtes CNS, cardiac muscle -Diuresis -Induces smooth muscle relaxation -CNS signs: agitated/hyperactive, increased mental alertness, increased response to normal stimuli -Can cause pancreatitis |
|
|
|
Clinical signs of Methylxanthine Toxicity
|
-Mostly CNS and cardiac signs
-GI signs at lower doses -Vomiting, diarrhea -Restlessness, hyperactivity, hyperreflexia (early) -Muscle twitching, seizures (late) -PU/PD due to diuresis -Tachycardia, tachyarrhythmia, severe arrhythmias -Panting -Electrolyte changes (hypokalemia) -Hyperthermia -Increased BP due to vasoconstriction -Coma |
|
|
|
Diagnosis of Methylxanthine Toxicity
|
-Usually based on history and clinical signs
-Can detect methylxanthine in tissues, serum, urine, stomach contents -Can detect caffeine --hard to do, quickly metabolized |
|
|
|
Methylxanthine Exposure Treatment
|
-Decontamination
-Induce vomiting -Multiple doses of activated charcoal to get everything from enterohepatic recirculation -Control hyperreactivity and seizures -Treat tachycardia and VPCs (b-blockers, lidocaine) -Urinary catheterization? -Promote diuresis through fluid therapy |
|
|
|
Grapes and Raisin toxicity
|
-Cause renal failure in susceptible dogs
-0.7-1 oz/kg toxic dose? -Unknown pathogenesis, unknown location of toxin --within flesh of the friut |
|
|
|
Grape and raisin toxicity Treatment
|
-Emesis, decontamination
-Charcoal and diuresis for 36-72 hours -Monitor renal values for 3 days -Hospitalization is needed! -If animal makes it through first 2-3 days, should be fine -If animal develops signs of acute renal failure, prognosis is guarded |
|
|
|
Xylitol toxicity
|
-Sugar substitute, most common in gum
-Strongly stimulates insulin release in dogs, causes hypoglycemia within 5 minutes to 18 hours -Can cause hepatic necrosis in 8-12 hours -1 or 2 pieces of gum with xylitol can be toxic to a 10kg dog |
|
|
|
Xylitol toxicity clinical signs
|
-Looks like hypoglycemia early, liver failure late
-Ataxia -Collapse -Seizures -Liver failure --bleeding, icterus -DIC |
|
|
|
Xylitol toxicity Treament
|
-Decontamination
-Activated charcoal is not effective in binding xylitol -Supportive care --Hospitalize and monitor for 12 hours |
|
|
|
Mold Food Toxicity
|
-Dairy, nuts, grains, legumes
-Trash! Compost! -Tremorgens in molds are usually produced by penicillium species -Lots of mechanisms of action, all lead to similar clinical signs --action potential --NT action or release --NT levels |
|
|
|
Diagnosis of Moldy Food/Tremorgenic toxicity
|
-Test food or gastric contents, vomitus
|
|
|
|
Clinical signs of Moldy food exposure
|
-Muscle tremors leading to seizures (can lead to death)
--death will occur quickly after ingestion if it is going to happen --Death is usually due to respiratory failure -Metabolic acidosis and cellular destruction -Hyperthermia secondary to tremors -Vomiting -Behavioral/mental status changes -Tachycardia -Signs may last for days to a week --metabolized very slowly |
|
|
|
Moldy food exposure treatment
|
-Asymptomatic: emesis or GI lavage with charcoal/cathartic
-Neurological signs: treat seizures and tremors --supportive care |
|
|
|
Mothball Toxicity
|
-Napthalene or paradichlorobenzene
-Napthalene is most toxic, causes Heinz bodies, hemolysis --methemoglobinemia |
|
|
|
Naphthalene Toxicity clinical signs
|
-Vomiting
-Weakness, secondary to anemia -Icterus secondary to hemolysis -Collapse if anemia is severe enough |
|
|
|
Paradichlorbenzene Toxicity Clinical Signs
|
-Affects liver and CNS
-Can cause heinz body anemia, more often liver signs -GI upset -Drooling -Depression -Ataxia -Disorientation -tremors -Seizures |
|
|
|
Mothball Toxicity Diagnosis
|
-Test body fluids or tissues for Naphthalene or paradichlorobenzene within 24 hours of ingestion
|
|
|
|
Mothball Toxicity Treatment
|
-Emesis
-Activated charcoal -Cathartic -Supportive care --packed RBCs, treatment for methemoglobinemia |
|
|
|
Coins/Pennies as Toxicity
|
-Pennies since 1983 contain Zinc, zinc causes toxicity
-Stomach acids leach zinc out of pennies -Causes intravascular hemolysis |
|
|
|
Clinical signs of Penny/Zinc toxicity
|
-GI signs
-Weakness/collapse -Anemia -Icterus -Hemoglobinemia, hemoglobinuria -Acute renal failure |
|
|
|
Diagnosing Penny/Zinc toxicity
|
-Measure zinc levels
-Take abdominal radiographs, look for a penny! |
|
|
|
Zinc/Penny toxicity Treatment
|
-Induce vomiting if penny was eaten recently
-Remove zinc source --endoscopy -Chelation by binding zinc -Supportive care for severe anemia |
|
|
|
Lead Toxicity
|
-Paints, toys, fishing tackle, car batteries, golf balls, plumbing materials
-Decreases the stability of RBC membranes --makes RBCs very fragile --RBCs are destroyed and removed from circulation early -Will see regenerative anemia, basophilic stippling, nucleated RBCs -Causes GI, renal, neuronal damage -Younger animals are more susceptible, more permeability in BBB to absorb the lead |
|
|
|
Lead toxicity clinical signs
|
-Take a while to develop, takes the body time to respond
-Signs appear 3-15 days post ingestion -Vomiting -Anorexia -Vocalization -Seizures -Strange neurologic behavior, paresis -Megaesophagus |
|
|
|
Lead toxicity Diagnosis
|
-Full body radiographs, look for metallic foreign bodies
-Measure Pb levels in the blood or tissue post-mortem |
|
|
|
Lead toxicity treatment
|
-Decontamination
-Cathartic -remove source of Pb -Chelate Pb -Supportive care |
|
|
|
Chelation Therapy
|
-Give mediation that will bind the toxin in the system
-Most are expensive -Oral or SQ medication -Succimer (DMSA) oral therapy: chelated Pb is excreted in urine --very expensive! -Ca EDTA: SQ --do not use in patients with renal disease, will make patient hypercalcemic -D-penicillamine: PO, cannot use for Pb in GI tract -If Pb levels increase after chelation therapy, look for continued exposure -Animal may act as a marker for human exposure! |
|
|
|
Ethylene Glycol Toxicity
|
-In a lot of household products
--Automobiles, toilets, industrial solvents, rust removers, film processing, heat exchangers -Tastes sweet, attractive to animals -Has narrow margin of safety, lethal doses in a small amount --Dog: 2-6 ml/kg --Cat: 2-4 ml/kg --Humans: 1.5 ml/kg |
|
|
|
Ethylene Glycol
|
-Ethylene glycol itself is relatively non-toxic
--causes inebriation and mild gastritis -Metabolized in liver via alcohol dehydrogenase -Ethylene glycol ⇒ glycoaldehyde (CNS dysfunction) ⇒ glycolic acid (metabolic acidosis) ⇒ glyocylic acid ⇒ hippuric, oxalic, and formic acid -Ca oxalate causes renal dysfunction |
|
|
|
Glycoaldehyde
|
-Formed from metabolism of ethylene glycol via alcohol dehydrogenase
-Causes CNS dysfunction -Can be further metabolized to glycolic acid (Causes metabolic acidosis) |
|
|
|
Metabolism of Ethylene Glycol toxicity and Mechanisms of Damage
|
-Clinical signs follow progression of metabolism
1. Ethylene Glycol: CNS depression, narcotic or euphoric effect 2. Glycoaldehyde: affects cell respiration, affects on metabolism of different products --metabolic acidosis 3. Acid intermediates: metabolic acidosis 4. Ca oxalate: crystalluria, blockage of renal tubules, hypocalcemia, epithelial necrosis |
|
|
|
Clinical signs of Ethylene Glycol toxicity
|
-Clinical signs follow progression of metabolism of ethylene glycol
1. 1-12 hours post-ingestion --nausea, emesis, CNS depression, ataxia, tachycardia, PU/PD, dehydration, hypothermia 2. 4-24 hours post ingestion --severe acidosis, hyperventilation, cardiac conduction disturbances, coma, convulsions, death 3. 24-72 hours post-ingestion (earlier in the cat) --oliguric renal failure, anorexia, vomiting |
|
|
|
Approach to a Toxic patient
|
1. put in IV catheter
2. Collect blood and urine for analysis 3. ECG 4. Blood pressure |
|
|
|
Early laboratory changes with Ethylene Glycol toxicity
|
-Increased anion gap due to lactic acid, glycolic acid, glyoxylic acid, oxalate
1. Increased in unmeasured ions --ions from ethylene glycol --Increased anion gap does not last that long, increases by 3 hours, peaks by 6 hours, remains elevated for at most 48 hours 2. Increased osmolar gap 3. Ca oxalate crystals in urine within 3-5 hours of ingestion 4. Ethylene glycol metabolites in serum/plasma or urine 5. Isosthenuria, decreased concentrating ability --osmotic diuresis 6. Hyperphosphatemia due to rust inhibitors in ethylene glycol product 7. Hyperglycemia 8. Hypocalcemia |
|
|
|
Increased Anion Gap
|
-More negatively charged unmeasured ions
-Decreased bicarbonate, bicarbonate is being used to buffer other negative molecules -Indicates ethylene glycol toxicity or other metabolic acidosis |
|
|
|
Osmolar gap
|
-Should be about 10
-Increase osmolar gap indicates increase in uncharged particles in the plasma -Increases within 1 hour of ingestion --parallels increase in serum ethylene glycol -May see gap of up to 150 in 3 hours -Can reach up to 450 -Calculating osmolar gap, and multiplying by 5 gives approximation for serum ethylene glycol concentration |
|
|
|
Osmolality
|
-Count of the total number of osmotically active particles in a solution
-Equal to the sum of all of the molalities of the solutes present in the solution -Na, BUN, and Glucose are major contributors to blood osmolality |
|
|
|
Calculating Osmolality
|
(Nax2)+(BUN/2.8)+(Glucose/18)
|
|
|
|
Major causes of Metabolic Acidosis
|
1. Renal failure
2. Diabetic ketoacidosis 3. Lactic acidosis 4. Toxin (exogenous acids, ethylene glycol) 5. Loss of bicarbonate/base |
|
|
|
Ethylene Glycol Toxicity Late laboratory changes
|
1. Renal impairment
--increased BUN and creatinine --Hyperkalemia 2. Ca oxalate crystals in urine --monohydrate or dihydrate |
|
|
|
Oliguric renal failure with Ethylene Glycol toxicity
|
-Increased BUN and creatinine
-Usually occurs within 24-48 hours in dogs -Within 12 hours in cats -Hyperphosphatemia due to decrease in GFR -Hyperkalemia due to increase in K excretion --CAN BE LIFE THREATENING |
|
|
|
types of Azotemia
|
1. Pre-renal azotemia
--Due to DEHYDRATION 2. Primary renal azotemia: --toxic effect --kidney dysfunction 3. Post-renal: --obstructive process |
|
|
|
Lesions seen with Ethylene Glycol Toxicity
|
-Pale, tan, swollen kidneys
--can see on ultrasound before death, will see "halo effect" |
|
|
|
Treatment of Ethylene Glycol Toxicity
|
-Decontamination
--usually too late once patient is in hospital --may be neurologic patient, don't want to induce vomiting if patient can't control airway -Treat coma, convulsions, arrhythmias -Correct acidosis -Maintain or establish urine flow -Monitor serum Calcium levels -Dialysis -Ethanol, acts as competitive substrate for alcohol dehydrogenase -Fomepizole, alcohol dehydrogenase inhibitor (fewer side effects, does not make patient drunk) |
|
|
|
Ethanol as treatment for Ethylene Glycol Toxicity
|
-Readily available, cheap
-Acts as competitive substrate for alcohol dehydrogenase -IV vodka to treat patient -Dogs: 20% solution -Cats: 20% solution |
|
|
|
Fomepizole as treatment for Ethylene Glycol Toxicity
|
-Alcohol dehydrogenase inhibitor
-More effective than ethanol -Give loading dose and following doses -NOT approved for use in cats --if treated within 3 hours, cats do OK --if treated after 4 hours, cats die -Does not have same CNS effects as ethanol -Avoids unpredictable metabolism of ethanol -More potent and specific inhibitor of liver alcohol dehydrogenase |
|
|
|
What to do with patient with Ethylene Glycol toxicity
|
1. Get venous access, collect blood
2. Place urinary catheter 3. administer ethanol or 4-MP 4. Dialysis 5. Monitor |
|
|
|
Diagnosing a toxin
|
-Toxins can look like other medical conditions, other medical conditions can look like toxins
-ALWAYS keep index of suspicion high for toxins -More often than not, is not a toxin and is spontaneous medical condition -Hate to diagnose a toxin because it is so treatable early, and less treatable later on |
|
|
|
Ethylene Glycol Summary
|
-Alcohol
-Has rapid absorption, distribution, metabolism, and excretion -Metabolized to acids by alcohol dehydrogenase -Diagnose based on exposure, clinical signs, acidosis, hypocalcemia, increased anion gap, increased osmolar gap, and measuring ethylene glycol in blood -Treat: decontamination, 4-MP, ethanol, dialysis, IV fluids, supportive care -Prognosis is good if caught and treated early --prognosis is bad if not caught early! |
|
|
|
Summary of Household Hazards
|
-LOTS of potential hazards in the house
-Toxin exposure is relatively rare compared to spontaneous diseases -Keep index of suspicion high! Earlier diagnosis and treatment is better prognosis for patient |
|
|
|
Types of Rodenticides
|
-Anticoagulant (most common)
-Bromethalin -Cholecalciferol (vitamin D) -Zinc phosphide -Strychnine |
|
|
|
Discovery of Anticoagulants
|
-Hemorrhagic syndrome in cattle in N. Dakota and Canada in 1920s
-Associated with sweet clover that had become moldy -Coagulopathy developed via converstion of fungus to coumarin to dicoumarol |
|
|
|
Warfarin
|
-Discovered in 1940s
-Coumarin analog that is more potent than dicoumarol -Widely used as a blood thinner in patients with thrombotic or coronary disease -AKA coumadin -Also used for rodent control in bait -All current anticoagulant rodenticides are structurally related to warfarin or indandione |
|
|
|
1st generation of Anticoagulant rodenticides
|
-Warfarin
-3-(alpha-pheyl-beta-acetylethyl-4 hydroxycoumarin -Initially very common -Products have a range of warfarin in the baits (0.025-1%) -Dogs, large animals, unintended animals like to eat bait -Chemical suffix: 4-hydroxycoumarin -Rodents rapidly became resistant --not really used anymore -Still used medically as coumadin for blood thinning |
|
|
|
Indandiones
|
-Anticoagulant rodenticide
-1,3 (2H)-dione or 1,3-indandione as active ingredient -Varies a lot in percentage of active ingredient ingested |
|
|
|
2nd generation Anticoagulant Rodenticides
|
-DEveloped in 1970s
-Have some coumarin or indandione but have increased potency -Much longer half-life -Ideally a single lethal feeding (ideal for rodents, not good for accidental ingestion) |
|
|
|
Coumarin-based 2nd generation anticoagulant rodenticides
|
-Brodifacoum
-Difenacoum -Bromadiolone |
|
|
|
Indandione-based 2nd generation anticoagulant rodenticides
|
-Diphacinone
-Chlorophacinone |
|
|
|
Exposure to Anticoagulant Rodenticides
|
-Via exposure to rodenticide formulations
-Potential to get into medicinal coumadin, less likely -Most often in dogs -Can happen in cats, pigs, ruminants, hroses, pet birds, rodents, rabbits -For large animals, bait package is usually not big enough to do much damage |
|
|
|
Anticoagulant Rodenticide Secondary Toxicosis
|
-Relay toxicosis
-Predator species eats prey species that has eaten rodenticides -Not so much with 1st generation rodenticides, can be an issue with 2nd generation rodenticides |
|
|
|
Common trade names for Anticoagulant Rodenticides
|
-Brodifacoum:
--D-com --Havoc --Hombre --Final -Diphacinone --Ditrac --Exterminator's choice --Liqua-tox --Statesman --Tomcat MUST get ahold of the ingredient list! Cannot go by trade name! |
|
|
|
Pharmacology of Anticoagulant Rodenticides
|
-Absorption: through digestive tract
-Distribution: carried through body in serum bound to albumin --concentrated by the liver -Metabolism: occurs in liver via mixed function oxidases --some inactive metabolites are excreted via kidneys -Elimination: half-lives vary between 1st and 2nd generation --Warfarin: 14.5 hours in dogs --Diphacinone: 15-20 days in humans --Brodifacoum: more than Diphacinone |
|
|
|
Acute Oral LD50 for Anticoagulant Rodenticides
|
-Fairly high amount of warfarin must be eaten
-MUCH less of brodifacoum and diphacinone need to be ingested to be lethal |
|
|
|
Predisposing factors to Anticoagulant Rodenticide Toxicity
|
-High dietary fat intake
-Prolonged oral antibiotic therapy -Liver disease (decreased vitamin K) -Biliary obstruction (decreased vitamin K) -Hypoalbuminemia (less serum protein binding capability) -Concurrent protein-bound drug administration -uremia -Aspirin therapy (decreases platelet function) |
|
|
|
Anticoagulant Rodenticide mechanism of Action
|
-Liver produces clotting factors (pro-zymogens)
-Converted into active clotting factors by vitamin-K dependent carboxylase -Vitamin K is needed to convert clotting factors from inactive to active form -Vitamin K Epoxide reductase converts used vitamin K back into active form -Anticoagulant rodenticides prevent the function of Vitamin K epoxide -Liver is still making clotting factors, but they cannt be activated |
|
|
|
Vitamin K epoxide
|
-Converts vitamin K used in clotting factor activation pathway back into active form
-"Recycles" vitamin K -Inhibited by anticoagulant rodenticides |
|
|
|
Treatment for Anticoagulant Rodenticide toxicity
|
-Give vitamin K
-Body cannot recycle vitamin K that is already present, but adding more can activate clotting factors |
|
|
|
Clotting factors relying on Vitamin K
|
-II, VII, IX, X
-2, 7, 9, 10 -Factor 7 has shortest half-life -Protein C and Protein S are important also |
|
|
|
Clinical signs of Anticoagulant Rodenticide Toxicity
|
-Signs take 3-5 days to appear
-Acute death can happen, but not common --hemorrhage into CNS and other vital organs -Depression, anorexia, anemia -Respiratory signs -Pale mucus membranes -Coughing or vomiting blood -Can see bleeding anywhere --scleral, intraocular, conjunctival, nasal, oral, urogenital, SQ hemorrhages |
|
|
|
Anticoagulant Rodenticide Presenting Complaint
|
-Lethargy or collapse
-Anorexia, decreased appetite -Vomiting -Dyspnea -Cough |
|
|
|
Clinical Laboratory Results with Anticoagulant Rodenticide Toxicity
|
-Prolonged prothrombin time (PT)
--within 24-48 hours of ingestion -Prolonged Activated partial thromboplastin time (PTT) --after 48 hours -Platelet count is usually normal to low normal --can be extremely low when there is significant hemorrhage -PCV and TS may be decreased secondary to blood loss -Albumin and globulin both decreased, indicates blood loss -Values vary greatly!! |
|
|
|
Thoracic Radiographs for Patients with Anticoagulant Rodenticide Toxicity
|
-Thoracic cavity is the main place where bleeding happens
-Increased mediastinal soft tissue opacity -Narrowing of the trachea -Pleural effusion -Alveolar patterns -interstitial patterns -Can bleed into lungs, around lungs, or into ariway |
|
|
|
Abdominal Radiographs for Patients with Anticoagulant Rodenticide Toxicity
|
-Loss of abdominal detail
-Loss of detail of retroperitoneal space -Loss of distention of retroperitoneal space |
|
|
|
Abdominal Ultrasound for Patients with Anticoagulant Rodenticide toxicity
|
-Free fluid and effusion
-Echogenic, cellular effusion (blood) |
|
|
|
Diagnosis of Anticoagulant Rodenticide Toxicity
|
-History of exposure
-Ask if there is rodenticide on the property -Coagulopathy, Prothrombin time is prolonged more than prolonged activated partial trombopastin time -Responds to vitamin K1 therapy -Green feces -Find anticoagulant in whole blood, serum or liver -Can do anticoagulant rodenticide screen if there is a strong suspicion |
|
|
|
Anticoagulant Rodenticide Toxicity Screen
|
-Samples can be identified for a variety of products
-brodifacoum -Bromodiolone -Chlorophacinone -Coumafuryl -Dicoumarol -Difenacoum -Warfarin -Valone Only need a trace amount to identify, none should be present in normal blood |
|
|
|
Post-mortem findings of Anticoagulant Rodenticide toxicity
|
-generalized hemorrhage in thoracic or abdominal cavity
-Hemorrhage into mediastinum, pericardium, periarticular spaces, joints, subcutaneous tissues -Hemorrhage into sub-dural space -Hemorrhage into GI tract is less common, more primary hemostasis -Flaccid and hemorrhagic heart -Centrilobular hepatic necrosis secondary to aniema and blood loss |
|
|
|
Coagulation Cascade
|
PT: measures extrinsic pathway and factor VII
|
|
|
|
Treatment for Anticoagulant Rodenticide Toxicity
|
-Dosage ingested determines treatment
-Less than 1/10 of LD50 ingested, only have to observe --do PT 48-72 hours post ingestion -More than 1/10 of LD50 or unknown dose: --less than an hour or unknown after ingestion, induce emesis and give activated charcoal and catharic --more than several hours after ingestion, activated charcoal and cathartic -Give vitamin K 2.5 mg/kg PO q12 for 4 weeks -Check PT 40-72 hours post ingestion, if prolonged give vitamin K -DO NOT start vitamin K and then test PT, will be normal regardless |
|
|
|
Treatment of an actively bleeding animal with Anticoagulant Rodenticide Toxicity
|
-NEED PLASMA!!
-Anemic: fresh whole blood, packed RBCs, Fresh frozen plasma --need active clotting factors right away -Not anemic: fresh frozen plasma -Vitamin K 5mg/kg SQ -Continue vitamin K 2.5mg/kg SQ or PO q12 for 4 weeks -Monitor PT |
|
|
|
Vitamin K Administration
|
-IV: can cause anaphylaxis
-IM can increase risk of bleeding (no clotting factors) -Give PO if not needed quickly, has best bioavailability -Give SQ for fast absorption |
|
|
|
Prognosis for Anticoagulant Rodenticide Toxicity
|
-Depends on extent and area of hemorrhage
-Bleeding mildly, good prognosis -Severe Itracranial hemorrhage, severe respiratory compromise, bad prognosis -Most dogs will survive |
|
|
|
Anticoagulant Rodenticide Differential Diagnoses
|
-Liver disease, not producing adequate clotting factors
--usually comes with other signs (hypoglycemia, BUN is affected, SICK animal) -Inadequate vitamin K intake or absorption, GI disease -Hereditary bleeding disorders -DIC secondary to infection, neoplasia -Trauma -Immune-mediated Hemolytic anemia or thrombocytopenia --usually bleed in GI tract, mucosal surfaces, epistaxis |
|
|
|
Most important thing to do with Anticoagulant Rodenticide toxicity
|
1. Identify toxin ingested (anticoagulant rodenticide vs. other rodenticide)
2. If acute ingestion, induce emesis, give activated charcoal and cathartic -Give vitamin K 2.5 mg/kg PO q12 for 4 weeks -Check PT at 48-72 hours post ingestion, give vitamin K if prolonged 3. Recheck PT 48-72 hours after last dose of vitamin K -treat for 2 more weeks if still prolonged |
|
|
|
Most important thing for actively bleeding anticoagulant rodenticide toxicity
|
-Provide active clotting factors!
--fresh frozen plasma --fresh whole blood -Vitamin K 5 mg/kg SQ -Continue Vitamin K 2.5 mg/kg SQ or PO q 12 4 weeks -Monitor PT 48-72 hours after last dose of vitamin K |
|
|
|
Types of Rodenticides
|
-Anticoagulants
-Cholecalciferol-based -Bromethalin -Zinc and Aluminum phosphate -Strychnine -Aldicarb -May baits have multiple active ingredients |
|
|
|
Cholecalciferol-based rodenticides
|
-Vitamin D is active ingredient
-Cholecalciferol is rapidly absorbed in stomach, transported to liver -Activation is via vitamin D transport proteins in liver -Cause hypercalcemia, increase serum Ca and P |
|
|
|
Effects of Hypercalcemia and hyperphospahatemia
|
-Will cause tissues to excite (nerves, muscles, myocardial cells)
-Soft tissue mineralization -Ca is important for a normal coagulation cascade -Can be due to cholecalciferol rodenticide toxicosis |
|
|
|
Ca on a blood panel
|
-Look for total serum calcium
-Serum calcium can be: --bound to protein (albumin) 40-45% --Complexed calcium, with anions (phosphate, citrate, bicarbonate, lactate) --ionized Ca, biologically active, 50% |
|
|
|
Ionized Calcium
|
-Bioactive calcium in the blood
-50% of Ca in blood is ionized -Under the influence of parathyroid hormone and calcitriol (vitamin D3) -Tightly controlled in animals --1.25-1.5 mmol/L in dogs --1.1-1.4 mmol/L in cats |
|
|
|
Calcitriol regulating Ca in GI tract
|
-Main impact is on the GI tract, small intestine
-Calcitriol stiulates enterocytes to produce calbindin-D --proteins help transport calcium from intestinal lumen into the blood --act on enterocytes -Increases P absorption via GI epithelium -Ca and P increase in serum, are absorbed from GI tract |
|
|
|
Calcitriol on Bone
|
-Enhances PTH action on osteoclasts, causes bone resorption
-Ca and P are liberated from the bone and into the blood |
|
|
|
Calcitriol in the Kidneys
|
-Increases Ca and O absorption by renal epithelial cells in renal tubules
|
|
|
|
Calcitriol and Calcium
|
-Acts to increase serum Ca
-Acts on GI tract, bone, kidneys |
|
|
|
Cholecalciferol rodenticide Toxic doses
|
-Dogs: 0.5-3 mg/kg
-No toxic dose known in cats -Younger animals are more susceptible -Relay toxicosis is uncommon |
|
|
|
Causes of Clinical signs of Cholecalciferol Rodenticide toxicity
|
-Affects CNS< GI tract, heart, kidneys
-Effects are seen within 12-18 hours after ingestion --Can be seen as late as 36 hours post ingestion -Signs are Mostly due to ionized hypercalcemia -Changes cell membrane permeability -Changes Ca pump activity (Ca ATPases) -Causes soft tissue mineralization |
|
|
|
Clinical Signs of Cholecalciferol Rodenticide Toxicity
|
-Anorexia, weakness, depression
--Decreased excitability of skeletal muscles --Decreased excitability of neurons in CNS -PU/PD --low urine SG, impaired action of ADH within renal tubules -Vomiting and diarrhea --changes in GI motility --direct effects on CNS vomiting center -Kidney failure --azotemia, uremia, GI signs |
|
|
|
Less common clinical signs of Cholecalciferol rodenticide toxicity
|
-Cardiac effects
-Shortened Q-T interval, prolonged P-R interval -Ventricular fibrillation with severe hyperalcemia or mineralization of cardiac muscle -Hypertension in humans (vasoconstriction due to hypercalcemia and increased SVR) -Seizures, muscle twitching |
|
|
|
Cholecalciferol Rodenticide Toxicity Differential Diagnosis
|
-All based on hypercalcemia
-HARDGOINS --Hyperparathyroidism --Addison's disease --Renal Disease --Hypervitaminosis D --Granulomatous Disease --Osteolytic disease --Idiopathic/iatrogenic --Neoplasia --Spurious |
|
|
|
HARDGOINS
Hypercalcemia Differential diagnoses |
-Hyperparathyroidism
-Addison's disease -Renal Disease -Hypervitaminosis D -Granulomatous disease -Osteolytic disease -Idiopathic/iatrogenic -Neoplasia (lymphoma, anal sac carcinoma) -Spurious (measurement error) |
|
|
|
Diagnosis of Cholecalciferol Rodenticide toxicity
|
-History of ingestion or exposure from environment
-Hypercalcemia on blood panel -Hyperphosphatemia (within 12 hours) -Azotemia due to acute kidney injury and tubular dysfunction --proteinuria, glucosuria -Vitamin D metabolites in the serum -Hyperkalemia and metabolic acidosis in cats -Low Urine specific gravity |
|
|
|
Cholecalciferol Rodenticide toxicity Necropsy Findings
|
-Soft tissue mineralization
--kidneys, lungs, atria, stomach, GI mucosa, myocardium, blood vessels -Hyperplasia and hypertrophy of parathyroid follicular cells --secrete calcitonin, in over-drive trying to decrease serum Ca levels |
|
|
|
Treatment for Cholecalciferol Rodenticide toxicity
|
-Lower serum Ca concentration
-Induce emesis maybe, if recent ingestion and no other signs that will make emesis a bad idea -Volume expansion -Fluid therapy is very important |
|
|
|
Fluid therapy for Cholecalciferol Rodenticide Toxicity
|
-Animals are usually dehydrated, want to correct over 4-6 hours
-Use 0.9 NaCl fluid!!! --Saline is fluid of choice --Expands intravascular volume and causes dilution effect, decreases serum Ca -Dilution promotes movement of fluids to kidneys for Ca removal -Added Na load to kidney promotes Ca excretion -Use NaCl (Saline)!!! |
|
|
|
Diruetics for Cholecalciferol Rodenticide Toxicity
|
-make sure patient is adequately hydrated before and during diuresis
-Keep up with IV fluids while using diuretic -Furosemide is diuretic of choice --stimulates Ca excretion -Match urine volume loss to avoid dehydration -Avoid thiazide diuresis, increases Ca reabsorption from the kidney |
|
|
|
Glucocorticoids for Cholecalciferol Rodenticide Toxicity
|
-Prednisone, dexamethasone
-Decrease osteoclastic resorption of bone -Decrease Ca absorption in GI tract -Increase renal excretion of Ca -Use with caution if etiology of hypercalcemia is unknown --esp if lymphoma is possible, will treat lymphoma and will not be able to adequately diagnose lymphoma as underlying disease |
|
|
|
Calcitonin as treatment for Cholecalciferol Rodenticide Toxicity
|
-Inhibits osteoclastic resorption from bone
-Can consider if fluids, diuretics, or steroids are not working as therapy -Effects are unpredictable and short-lived -resistance can occur -Expensive! has to be special-ordered |
|
|
|
Bisphosphanate as treatment for Cholecalciferol Rodenticide
|
-Pamidronate disodium
-Inhibits osteoclastic resorption of bone, decreases Ca in serum -Takes a few days to be effective -Have long-lasting effect (7-8 days) -Good for long-term therapy of hypercalcemia |
|
|
|
Other possible treatment for Cholecalciferol Rodenticide Toxicity
|
-Hemodialysis: for acute and intrinsic renal failure
-Ca channel blockers: prevents Ca from entering cells and having effect (Diltiazem) -Sodium bicarbonate for metabolic acidosis --decreases ionized Ca -Mithramycin with significant renal toxicity -May need to treat animal for several weeks! |
|
|
|
Cholecalciferol rodenticide toxicity treatment
|
-May need to treat animal for several weeks!
--Cholecalciferol and vitamin D metabolites have long half-lives -Maintenance therapy for 4 weeks -Low Ca diet -Phosphate binders -Not a quick, easy fix especially when azotemia and renal failure develops |
|
|
|
Bromethalin
|
-In lots of different rat baits
-Absorbed from GI tract quickly, reaches peak plasma concentration within a few hours -Cats are more sensitive than dogs -Undergoes extensive enterohepatic recitculation --absorbed in GI tract, absorbed in liver, put into bile and back into GI tract --Need to do multiple doses of activated charcoal! |
|
|
|
Bromethalin Pathogenesis
|
-Uncouples oxidative phosphorpylation
-Shuts down kreb's cycle -Decreased ATP production, decreased availability of ATP for ion pumps -Na/K ATPase needs ATP to put Na out of cells --Na stays in cells, H2O follows Na, cells swell -In CNS, increasing pressure due to swelling is really bad |
|
|
|
Bromethalin Rodenticide toxicity Clinical findings
|
-Edema leading to increased ICP and pressure on peripheral axons
-Ascending paralysis, ataxia -Muscle tremors, hyperexcitability, hyperreflexia -Seizures -CNS depression or Coma -Death due to respiratory muscle paralysis, brain swelling, seizures -Onset of clinical signs occurs in 4-36 hours post ingestion -Mixed inhibitory and excitatory effects |
|
|
|
Bromethalin Toxicity Differential Diagnoses
|
-Strychnine
-Metaldehyde -Insecticides -Zinc phosphide -Methylxanthines -Tremorgenic mycotoxins -Permethrin -Illicit drugs |
|
|
|
Bromethalin toxicity Diagnosis
|
-History of exposure
-Not may tests to do, have to rely on owner saying it is present in environment -Post-mortem can do residue test on kidney, liver, fat, brain -Edema in CNS and other cells on histopathology |
|
|
|
Bromethalin toxicity treatment
|
-No antidote! no real treatment
-If patient has CNS signs, might not want to induce emesis --Can do gastric lavage -Repeated doses of activated charcoal -Supportive care is big! --control tremors (benzodiazeptines, methocarbamol) --control seizures (benzodiazepines, barbiturates, propofol) --reduce CNS edema (mannitol, lasix, dexatethasone) --Maintain fluid balance, temperature, renal function, nutrition -Poor prognosis for affected animals |
|
|
|
Zinc and Aluminum Phosphide Rodenticide Toxicity
|
-Paste, powder, or grain based
-"kilrat" "rumutan" "ratoff" -0.5-10% active ingredient, high variability -Restricted use |
|
|
|
Zinc and Aluminum Phosphide Rodenticide Restricted Use
|
-Use is restricted in households, mostly industrial use
--some use illegally -Can be a risk to veterinarians and veterinary staff -Hazard to organisms that are not the target -Acute toxicity |
|
|
|
Zinc/Aluminum Phosphide rodenticide toxicity Action
|
-Activated in the stomach
--need low gastric pH, less than 5 -Zinc phosphide is liberated, form phosphine gas in acidic environment -Causes vomiting, absorption is limited in species that can vomit --limits toxicity -Stomach produces gas, patient becomes bloated, burps --gas is eructated, inhaled, directly toxic to the lungs |
|
|
|
Phosphine Gas
|
-Causes clinical signs in Zinc/Aluminum phosphide toxicity
-Released in stomach at low pH (less than 5) -Gas is rapidly absorbed -Interferes with protein and enzymatic function on a global level -Inhibits oxidative phosphrylation and ATP generation -Cytotoxic to pulmonary cells --causes pulmonary edema and pneumonitis, ARDS -Severe mucosal irritation from phosphide salts -Can be dangerous to owner, vet, and vet staff if inhaled!! stay well-ventillated! |
|
|
|
Clinical Signs of Zn/Al Phosphide Rodenticide Toxicity
|
-Fast onset of clinical signs, 15 min-4 hours
-Agitation, vocalization -Vomiting, hematemesis (vomit smells like garlic/rotten fish) -Abdominal bloating and pain -Dyspnea due to pulmonary edema -Cardia arrhythmias -Tremors, convulsions, seizures -Metabolic acidosis, hypocalcemia, coagulopathy |
|
|
|
Zn/Al Phosphide Differential Diagnoses
|
-Strychnine
-Methaldehyde -Organophosphates, carbamates -Arsenic -Primary CNS disease -Hepatic encephalopathy |
|
|
|
Diagnosis of Zn/Al Phosphide Toxicity
|
-History of exposure
-Garlic or rotten fish smell to vomitus -Clinical signs -Can do testing on stomach contents, but has to be sent out and takes time (will not help animal live) |
|
|
|
Necropsy findings of Zn/Al phosphide toxicity
|
-Post-mortem exam findings are not specific
-Congestion of organs -Acute lung injury, acute respiratory distress syndrome -Myocardial degeneration -Phosphine gas smell in stomach -Elevated Zn concentration in liver or kidney |
|
|
|
Treatment for Zn/Al Phosphide toxicity
|
-Decontaminaion/emesis depending on mentation
-Decrease production of phosphine gas --increase stomach pH, prevent formation of gas --acid suppressants, MgOH -Cardiovascular and respiratory support -IV fluids -Treat for shock -Intubate for mechanical ventilation -Seizure control -Kidney support and hepatic support, diuresis -Manage acid/base and electrolyte imbalances -Pain control -ROS scavengers, N-acetyl cysteine |
|
|
|
Strychnine
|
-Alkaloid from Strychnos-nux vomica plant
-Restricted use, only see toxicity on farms -Rodenticide that can cause significant relay toxicosis --problem for raptors and birds of prey -LD50 is low, does not take much to cause toxic clinical signs -Eliminated rapidly in urine within 24-48 hours --if animal can get through first 24-48 hours prognosis is pretty good |
|
|
|
Strychnine Mechanism of Action
|
-Cases competitive and reversible inhibition of glycine in CNS
--inhibitory NT --inhibit inhibitory NT, will see spastic response |
|
|
|
Clinical signs of Strychnine toxicity
|
-rapid onset, seen 10-120 minutes post ingestion
-Clinical signs related to inhibition of inhibitory glycine NT -Animal has excessive sensory input -Exaggerated motor responses -Tonic-colonic seizures -Rigid muscle extension --can lead to respiratory arrest if diaphragmatic muscles are arrested/spastic -Refractory seizures, cerebral swelling -Clinical signs progress quickly, lead to tonic rigidity of the limbs |
|
|
|
Outward clinical signs of Strychnine toxicity
|
-Anxiety, apprehension, tense, stiff animal
-Progression to tonic extensor rigidity of all 4 limbs --sawhorse stance -Light, noise, and touch sensitive -Tetanic seizures -Opisthotonus -Sardonic grin -Respiratory muscle paralysis -DEath |
|
|
|
Strychnine Differential Diagnoses
|
-Rabies
-Distemper -Tetanus -Organophosphates -Ethylene glycol -Lead -Metaldehyde -CNS disease -Lots of others |
|
|
|
Strychnine Diagnosis
|
-History of exposure and clinical signs
-Can test for strychnine in stomach contents or urine before death -On necropsy, animal will have intense onset of rigor mortis, then will relax |
|
|
|
Strychnine Toxicity Treatment
|
-Emesis and activated charcoal before clinical signs
-After clinical signs, do not induce emesis --gastric lavage instead -Main goal is to reduce and control seizures as animal eliminates the toxins -Dark, quiet environment -Muscle relaxation (methocarbamol) -IV fluids -O2 support or mechanical ventilation -Temperature control |
|
|
|
Strychnine Seizure control
|
-Supportive CNS therapy
-Diazepam or midazolam 0.5mg/kg to effect -Propofol Pentobarbitol -Levetiracetam -Mannose to maintain normotension and normoxemia |
|
|
|
Strychnine half life
|
-10 hours
-Animal can recover quickly -No long-lasting effects after complete recovery |
|
|
|
Aldicarb
|
-Category 1 toxin
-Not approved by the EPA for household use -Most commonly seen in granules -"Tres pasitos", mouse takes 3 steps and dies -Available for agricultural use |
|
|
|
Aldicarb Toxicity
|
-Carbamate pesticide
-Interferes with ACh-esterase --rapid on rapid off binding, temporary binding --clinical signs appear very quickly and resolve very quickly --muscarinic signs -Rapid absorption from the GI tract -LD50 for rats is 0.5-1.5 mg/kg if in liquid form --7.0mg/kg in granular form |
|
|
|
Aldicarb Muscarinic Clinical Signs
|
-Muscarininc clinical signs based on transient ACh-esterase inhibition
-DUMBELLS -Defecation and urination -Miosis -Bradycardia -Bronchorrhea -Emesis -Lacrimation -Lethargy -Salivation |
|
|
|
Aldicarb Nicotinic Signs
|
-Hypertension
-Muscle fasciculations -Tremors -Respiratory depression -Hypertension |
|
|
|
Aldicarb Toxicity Differential Diagnoses
|
-Organophosphates, work by same mechanism
--aldicarb is temporary, while organophosphates continues -Nicotine toxicity -Phenothiazins -Muscarine-containing mushrooms -Envenomation -Botulism -Encephalitis |
|
|
|
Aldicarb Diagnosis
|
-Exposure history
-Clinical signs -Aldicarb in the tissue, urine, or vomitus/stomach contents -Blood ACh-esterase activity should be less than 25% of normal --inaccurate in cats due to pseudocholinesterase in feline RBCs |
|
|
|
Aldicarb Toxicity treatment
|
-Decontamination via emesis or gastric lavage
-Activated charcoal -Parasympatholytic therapy to address muscarinic signs --Atropine: anti-muscarininc, 0.2-0.5 mg/kg (MUCH higher than normal atropine dose!) -Respiratory support due to aspiration pneumonia --O2 therapy, intubation -Cardiovascular support -IV fluids -Manage acid/base and electrolyte disturbances |
|
|
|
Aldicarb Recovery
|
-Clinical signs from aldicarb resolve quickly
-Complications do not resolve quickly --pneumonia |
|
|
|
Exposure Assessment
|
-Is this a poisoning or a medical condition?
-What is the exact product involved? -Maximum amount of product involved? -Is the LD50 of the substance helpful in clinical decision making? (NO! not helpful!) -Is this a non-toxic exposure |
|
|
|
Poison Control Centers
|
-Local human poison control center
-National Animal Poison Control center |
|
|
|
Common Non-toxic exposures
|
-Water-based paints
-Silica gel -Cat litter -Glow jewelry -Personal care products: Shampoo, conditioner, lotion, soap, shaving cream -Antacids -Rust -Plaster -Ballpoint pen ink -Crazy glue, white glue (do not pull them apart! let dissolve on own) -Chalk -Matches -Toilet bowl water -Glue traps |
|
|
|
Substances toxic in small doses
|
-Animals ingesting these substances need immediate medical attention
-Cannot be decontaminated or observed at home -Do not always know minimal toxic dose in animals -Camphor -Hydrofluoric Acid -Lindane -Gun Blue -Benzocaine -Acetaminophen -Toxic alcohols (methanol, ethylene, glycol) -Aspirin and aspirin related products -Lomotil -Ca channel blockers -Oil of wintergreen -Calcipotriene -5-fluorouracil |
|
|
|
Camphor
|
-Toxic in small doses
-In vick's vapor rub, vapostream, etc. -Rarely found in moth repellants anymore -Rapid acting neurotoxin, causes seizures without warning --difficult to manage patient, seizures occur without warning -Death can occur with ingestion of as little as 5 mL of camphorated oil (a few tablespoons) --super concentrated! does not take much to cause a toxicity -Has to be absorbed intestinally, not trans-dermally |
|
|
|
Treatment for Camphor toxicity
|
-Do not induce vomiting
-Supportive care in ER |
|
|
|
Hydrofluoric Acid
HF acid |
-Toxic in small doses
-Sources: automotive wheel cleaners, glass etching solution, rust removal products -VERY dangerous acid -Causes burns, electrolyte disturbances, death -Dilute solutions (less than 12%) can cause delayed injury -Systemically absorbed dermally, gets on skin and into systems -Toxic via all routes of exposure -Exposure over a large surface area with dilute solution or small area with concentration solution |
|
|
|
HF acid Mechanism of Action
|
-F ion dissociated, binds to Ca in patient
-Causes Ca precipitates --very painful under skin -Hypocalcemia -Hypomagneseimia -May cause ventricular fibrillation! |
|
|
|
Lindane
|
-Kills lice
-Present in shampoos, lotions, and creams -Very strong, prescription only -For external use only!!! -Rapid onset of unpredictable seizures --DO NOT induce vomiting |
|
|
|
Lindane Mechanism of Action
|
-Chlorinated hydrocarbon insectivide
-Interferes with K and Na ion fluxes across the axonal membrane as nerve impulses travel along axon -Causes rapid onset of seizures |
|
|
|
Gun Blue Toxicity
Selenious Acid |
-Inorganic selenium, used for gun cleaning
-Toxic via dermal route if area is denuded -Causes systemic toxicity --seizures, hypotension, cardiorespiratory arrest, shock -Ingestion of a few drops can cause illness -15ml |
|
|
|
Benzocaine
|
-Available in oral and topical anesthetics
--oragel, anbesol -Wide range of toxicity -Toxic in small doses -Causes methemoglobinemia cats without heinz body formation |
|
|
|
First steps in taking care of a Toxic patient
|
Airway
Breathing Circulation Disability, Dextrose, Decontaminaion, Drugs Decontamination often takes precedence! |
|
|
|
Gastric Decontamination
|
-Any technique that prevents absorption of a drug or chemical from the GI tract
-Goal is to decrease blood concentration of the toxin -Decrease amount of toxin that is absorbed -Reduce severity of the poison -Do what you can, won't always be able to get all of it |
|
|
|
Options for gastric decontamination
|
-Gastric emptying
-Activated charcoal (do in ER, not at home) -Cathartics help things move through faster --whole bowel irrigation -Emetics -Gastric lavage |
|
|
|
Emesis for gastric emptying
|
-Efficacy is improved if ingestion is recent and food is present in the stomach
-Not for rabbits or rodents -Hydrogen peroxide -Apomorphine for dogs -Xylazine for cats -DO NOT USE: salt water, liquid dishwashing soap, mechanical induction, excessive water |
|
|
|
Contraindications for Emesis
|
-Species cannot vomit
--rodents, rabbits, horses, ruminants -Risk of seizures or patient is already seizing -Caustic substances -Batteries or sharp foreign bodies -Substances with risk of aspiration |
|
|
|
Substances with Risk of Aspiration
|
-Petroleum distillate family
-Kerosene, gasolene, etc. -Do not induce emesis! -Covers more surface area, low viscosity -Easily aspirated when vomited -Not systemically toxic, just leave them in the stomach |
|
|
|
Complications with Emesis
|
-Persistent vomiting, hard to control how much the patient vomits (most common)
-Aspiration -Vagal-induced bradycardia -Esophageal injury (rare) |
|
|
|
Apomorphine hydrochloride
|
1. Stimulates chemoreceptor trigger zone
--"on" 2. Crosses BBB to depress emetic center --"off" Synthetic opiate Use in dogs only, emesis is more consistent in dogs compared to cats -do not know safe feline dose |
|
|
|
Apomorphine hydrochloride Route of Administration
|
-Give to DOGS only
-Conjunctival: unreliable onset of action, 2-10 minutes --easiest administration -SQ: 2-10 minutes -IM: fast, but erratic absorption -IV: immediate results |
|
|
|
Apomorphine hydrochloride Duration of Action
|
-Conjunctival: rinse out of the conjunctival sac after emesis
-IM: can be prolonged duration -IV: 1-2 minutes, short duration |
|
|
|
Hydrogen Peroxide
|
-Can be done at home
-3% H2O2 ONLY!! Nothing stronger -Fresh is better, older hydrogen peroxide does not bubble as well -Takes 10 minutes -Can repeat dose if it does not work in 10 minutes -1 tablespoon for all animals -Food in stomach encourages emesis |
|
|
|
Xylazine hydrochloride
|
-alpha-2 adrenergic agonist
-Used in CATS for emetic -Stimulates chemoreceptor trigger zone -Reliable emesis in cats and not for dogs -Higher dose will sedate the cat, lower dose will cause emesis -Make sure cat is hydrated --increased risk of hypotension with dehydrated animal |
|
|
|
gastric lavage
|
-For unconscious or anesthetized animal
-Do with secure airway -Allows gastric emptying when emesis is contraindicated -Do not use with hydrocarbon toxicity or caustics --increased risk for aspiration |
|
|
|
Gastric lavage complications
|
-Aspiration pneumonia
-Fluid and electrolyte imbalances --hyponatremia, water intoxication --hypernatremia with large volumes of saline -Esophageal perforation |
|
|
|
Emesis vs. gastric lavage
|
-Which works better?
There are no adequately controlled studies to show that either one is better than the other Choose based on situation |
|
|
|
Activated Charcoal
|
-Binds non-polar or large molecules
-Can pull toxins out of circulation also -Not effective for: alcohols, hydrocarbons, metals, inorganic minerals, caustics -1-2 mg/kg of powdered activated charcoal mixed with water --can come pre-mixed -May use a cathartic also (sorbitol) -Do not give with mineral oil, may interfere with charcoal adsorption |
|
|
|
Activated Charcoal does not work on:
|
-Alcohol (any type of alcohol)
--ethylene glycol, ethanol, methanol, -Hydrocarbons/petroleum distillate -Metals (iron, ca, K, etc.) -Inorganic minerals -Caustics |
|
|
|
Multi-doses of Activated Charcoal
|
-Use with drugs that have enterohepatic recirculation
--anticonvulsants (phenobarnital) -Use when a large amount of substance is still in GI tract -Do not use a cathartic with multiple doses --increases risk for electrolyte imbalances |
|
|
|
Contrainications for Activated Charcoal
|
-Caustics
--does not work, and do not need it -Agents with high risk of aspiration --hydrocarbons/petroleum distillates |
|
|
|
Cathartics
|
-Moves things through the bowel faster
-Give with Activated Charcoal to move activated charcoal bound with toxin through the GI tract -Only give with 1 dose of activated charcoal |
|
|
|
Cathartic contraindications
|
-Diarrhea
-Dehydration -Ileus |
|
|
|
Whole Bowel Irrigation
|
-Labor intensive! takes 2-6 hours
-Clear in, clear out -Poly-ethylene glycol solution --isotonic, will not cause electrolyte imbalances -Put through nasogastric tube, have to use high amounts -500ml/hour for pets -Use for metals, sustained release medications |
|
|
|
Sustained release medications are bad news for toxins
|
-Have to get medication out of the gut
-have to do whole-bowel irrigation |
|
|
|
Things to consider before gastric decontamination
|
1. Risk of the agent
2. Recent ingestion 3. Is activated charcoal alone sufficient? --large amount of agent ingested 4. Vomiting on their own, do not need to induce vomiting 5. Contraindications: --caustics --hydrocarbons --sharp objects |
|
|
|
Dog eats sustained release lithium
|
-Want to decontaminate, lithium is toxic
-No Activated charcoal, will not bind (metal) -Can induce emesis -Gastric lavage, pills will not fit in the tube -Whole bowel irrigation will also work |
|
|
|
Dog ingests gasoline
|
-Do not induce emesis (risk for aspiration)
-No Activated charcoal -No whole bowel irrigation -No gastric lavage DON'T CONTAMINATE! |
|
|
|
Cat eats 2 acetaminphen tablets 8 hours ago
|
-HIGHLY toxic to cats
-emesis will not do anything, neither will charcoal -Whole bowel irrigation will not have effect -No options for gastric decontamination, acetaminophen is out of GI system by 8 hours |
|
|
|
Antidotes
|
-A remedy that counteracts the effects of poison
-May affect poison's action, concentration, or binding -No universal antidote, does not exist |
|
|
|
NAC
|
-Use for acetaminophen toxicity
-Sulfur derivative -For best results treat ASAP --best if animal still has 30% of glutathione stores -No down-side to NAC -Optimally give it within 8 hours of acetaminophen ingestion -Also acts as anti-oxidant for free radicals -IV and PO versions exist, give based on tolerability and cost --PO version smells bad, can cause upset stomach |
|
|
|
Acetaminophen and Glutathione
|
-Acetaminophen destroys glutathione stores
-Metabolites (NAPQE) can also deplete glutathione stores -Small doses of Acetaminophen are Not a big issue for animals that have a lot of glutathione --liver and kidney are safe -Large doses can overwhelm glutathione stores |
|
|
|
NAC adverse reactions
|
-GI upset if given PO
-Bronchospasm if given IV -140 mg/kg loading dose --70 mg/kg IV or PO q6 5-7 more times |
|
|
|
4-methylpyrazole
Fomepizole |
-Antidote for ethylene glycol toxicity
-Approved for methanol poisoning in humans -Competitively inhibits alcohol dehydrogenase for 12 hours --no breakdown of ethylene glycol, no active metabolites formed -Very safe at standard doses -Very expensive -Need higher doses in cats to inhibit alcohol dehydrogenase |
|
|
|
Ethanol as antidote to Ethylene Glycol toxicity
|
-Competitive inhibitor of Alcohol dehydrogenase
-Prevents ethylene glycol from binding to alcohol dehydrogenase and breaking down into toxic active metabolites -Use in cats, cheaper -Uses equally as well as 4-methylpyrazole -MUCH cheaper! -Has side effects, animal gets drunk! -Need to make sure than the ethanol level in blood is 100mg/dL, lots of monitoring involved |
|
|
|
Flumazenil
|
-Originally marketed to reverse benzodiazepine anesthesia post-operatively
--works very quickly and very effective -Very expensive -Binds and displaces benzodiazepines from benzodiazepine receptor -No real dangerous side effects, can cause agonist-like activity -Need to monitor, short-acting --half life 1 hour |
|
|
|
Pralidoxime
|
-Antidote for clinically significant organophosphate poisoning
-Use with insecticide poisoning or warfare agents -Reverses inhibition of ACh-esterase by organophosphates and carbamate insecticides --knocks ACh-esterase inhibitor off of ACh-esterase -Not effective if irreversible binding or with long duration (aged binding) |
|
|
|
Pralidoxime Adverse effects
|
-Nausea, dizziness
-Infusion-related reactions --hypertension --tachycardia --muscle ridgidity |
|
|
|
Vitamin K1
|
-Reverses inhibitory affects of coumarin and coumarin derivatives on clotting factors 2, 7, 9, 10
--anticoagulant rodenticide toxicity -For symptomatic animals -Do not give as prophylaxis, makes monitoring difficult --cannot make good decision of when to discontinue treatment -Can be given PO, SQ -DO NOT GIVE IV, can cause severe anaphylatic reactions |
|
|
|
Succimer
|
-Contains dithiol groups that interact with metals, bind metals
-Sulfur-derived product -Use as antidote to arsenic, lead, mercury, silver, thallium toxicity -35 ug/dL -not a veterinary product, have to get from human hospitals -Make sure patient is hydrated -Will treat current toxicity, but will not treat underlying source of toxin |
|
|
|
Succimer Adverse Reactions
|
-GI-upset
-Sulfur-like odor of urine and breath -Transient increase in hepatic enzymes -Less likely than other chelators to bind dietary minerals -Does not enhance absorption of Pb from the GI tract |
|
|
|
Deferoxamine
|
-Antidote for iron and aluminum toxicosis
-Metal chelator -Binds iron to form ferrioxamine --ferrioxamine chelate is excreted via kidneys -Give for 24 hours or until Fe level is below 300 ug/dL -IV route is best, SLOWLY |
|
|
|
Deferoxamine Adverse effect
|
-Hypotension
-Anaphylactic reaction risk from rapid IV infusion -Ferrioxamine complex may cause hypotension --can accumulate in patients with renal issues |
|
|
|
Antivenins for Scorpions
|
-Antivenom for scorpions does not exist
|
|
|
|
Antivenins for Snakes
|
-Lots exist
-Call the zoo! -Crotalid FAB -Eastern coral snake -Foreign snakes |
|
|
|
Antivenin Mechanism of Action
|
-Blocks venom's ability to hit target tissues
-Causes hypersensitivity reactions --less risk with newer products |
|
|
|
Black Widow Antivenin
|
-Use with possibility of anaphylaxis
-Can usually just use supportive care and anti-pain drugs -Use in patients with neurotoxicity, hemodynamic instability, uncontrolled pain, or prolonged symptoms |
|
|
|
Naloxone
|
-Antidote for opioid toxicity
--allows return of adequate, spontaneous ventilation -Simple mechanism of action: antagonist at opioid receptor -Does not have many down-sides in animals, no serious adverse reactions -Short duration of action, have to make sure CNS and respiratory depression resolves -Usually given IV or IM, can be given SQ |
|
|
|
Digoxin Fab Antibodies
|
-"Digibind"
-Monocloncal antibody antidote -Used for digoxin, digitalis-like plants (lily of the valley, oleander, foxglove, Bufo toad poisoning, Red squill rodenticide) -Works best for straight digoxin, but can also work for the others -Monocloncal antibodies bind to free digoxin and prevent action --want FREE digoxin levels! |
|
|
|
Digitalis Toxicity Signs
|
-Causes hyperkalemia
-Cardiovascular heart block |
|
|
|
Down-sides to Digibind/Digoxin Fab antibodies
|
-Adverse reactions:
--hypokalemina (resolves on own) --Allergic reactions due to MAB --Rebound toxicity, binding does not last forever, depends on how fast the patient can clear digoxin -Very expensive! -Give 1-2 vials in animals |
|
|
|
Rx and OTC accidental Ingestion
|
-Accidental: pet eats owner's medication
-Therapeutic error -Idiosyncratic drug reaction -Unintentional mis-use: owner gives pet meds for human without consulting vet |
|
|
|
Ca Channel Blockers
|
-Many are in sustained-release formulations
--release drugs over a long period of time -Used as anti-hypertensive treatment -VERY toxic, and many are sustained-release! -Ex: Verapamil, Diltiazem, Nifedipine, Amlodipine |
|
|
|
Ca Channel Blockers mechanism of Action
|
-Block Ca into the cell, prevents Ca influx into the cell and prevents contraction
-Affects a lot of different cells, decreases Ca influx into: --pancreas, kidney, heart, etc. -Effects: --hypotension --Bradycardia and reflex tachycardia --pulmonary edema --hyperglycemia |
|
|
|
Ca Channel Blocker Overdose Treatment
|
-Support hypotension with Vasopressors
-Ca gluconate to replace Ca -Insulin/Dextrose infusion to address insulin drop and carbohydrate utilization by the heart --difficult to give right amount, have to call veterinary toxicologist -Serious issue! Treat with guidance of a veterinary toxicologist! |
|
|
|
Insulin/Dextrose infusion
|
-Given as treatment for Ca Channel blocker overdose
-Normally myocardium depends on fatty acids for energy -Ca channel toxicity makes myocardial cells carbohydrate dependent --Also uses carbohydrates due to lack of insulin (pancreatic beta cells are affected by Ca channel blockade) |
|
|
|
Cough and Cold preparations
|
-Decongestants (symoathomimetic amines)
-Antihistamines (H1 blockers) -Analgesics -Antitussives (dextromethorphan, opioids) -Expectorants (po guiafenesin) -All may contain a whole mix of stuff! --caffeine, alcohol, combinations, etc. -Need to check and make sure you know what is in the product |
|
|
|
Decongestants
|
-Lots of different types
-Stimulate alpha-1 receptors -Pseudoephedrine |
|
|
|
Pseudoephedrine
|
-Decongestant
-Affects both alpha and beta receptors --beta stimulation results in tachycardia and tachyarrhythmias --alpha stimulation causes peripheral vasoconstriction, hypertension -Inhibits bladder emptying, stimulates receptors that tighten bladder sphincter -Has been used to treat canine urinary incontinence |
|
|
|
Key clinical signs with Decongestant toxicity
|
-Hyperactivity
-Vomiting -Hyperthermia -Disorientation -Tachycardia (and sometimes reflex bradycardia) -Mydriasis |
|
|
|
Dog-specific Deongestant Issues
|
-Pseudoephedrine toxicosis causes increased agitation after diazepam administration
-Higher risk of toxicity compared t other patients -Clinical signs appear at 5-6 mg -Death can occur at 10-12 mg/kg |
|
|
|
Treatment for Decongestant Toxicity
|
-Decontamination
-Symptomatic supportive care to manage tachycardia, bradycardia, excess CNS stimulation -Acepromazine -Chlorpromazine -Phenobarbital |
|
|
|
Antihistamines
|
-MOA: block H1 receptors
-Chlorpheniramine -Diphenhydramine (cream and PO form) --cream is 2%, easy to get a toxicity! -Meclizine (motion sickness) -Calamine lotion, Caladryl (has benadryl also!) |
|
|
|
Clinical Signs of Antihistamine toxicity
|
-CNS depression
-Dry mucous membranes -Ataxia -Animal looks sleepy -Anticholinergic effects vary with agent and patient -No species-specific signs |
|
|
|
Treatment for Antihistamine toxicity
|
-Decontamination
-Supportive care |
|
|
|
Analgesics
|
-NSAIDS
-Acetaminophen -Aspirin |
|
|
|
NSAIDs
|
-Decrease pain, fever, inflammation
-Decrease renal blood flow, gastric mucous production, platelet aggregation -IbU -Carprophen -Naproxen -Etodolac -Have some major side effects! -Risk factors for renal toxicity: pre-existing renal disease, hypovolemia, hyotension |
|
|
|
NSAIDs Toxicity Key Clinical Signs
|
-Extension of therapeutic effects
-Vomiting, diarrhea, anorexia, hematemesis, melena -Lethargy, weight loss, liver enzyme elevations -Renal failure -NARROW margin of safety in both cats and dogs -Cats are 2x as sensitive as dogs --limited glucuronyl-conjugating ability |
|
|
|
NSAID toxicity Treatment
|
-Decontaminatino
-Symptomatic supportive care -GI protectants (avoid bismuth subsalicylate) --Anti-ulcer medications (sucralfate, misoprostol, H2 antagonist/blockers) -Fluids for vomiting animals and to preserve renal function |
|
|
|
Acetaminiphen Chemical Structure
|
-N-acetyl para amino phenol
|
|
|
|
Acetaminophen
|
-Tylenol
-Combination products: Fioricet, Percocet, Lorcet --LOTS of products have acetaminophen -Dog toxicity: 100-150 mg/kg --1 500mg tablet in a small dog -Cat toxicity: 10-60 mg/kg --1 325mg tablet in a normal cat |
|
|
|
Acetaminophen Toxicity Clinical Signs
|
-Vomiting, anorexia
-methemoglobinemia -Edema -Dogs are more prone to hepatic necrosis -Most common cause of heinz-body related toxicity in cats -In a mid patient will not see any clinical signs until hepatic necrosis or heinz-body formation |
|
|
|
Acetaminophen toxicity Treatment
|
-N-acetylcysteine (NAC): antidote
-Symptomatic treatment -Methylene blue may be needed in cats, give carefully at low doses -Cimetidine and ascorbic acid are NOT TO BE GIVEN, use NAC instead |
|
|
|
Aspirin
|
-Not used super often anymore as "aspirin" tablet
-Also in muscle rubs (BenGay) --very potent formulation!! 4.5g methyl salicylate= 6.3g aspirin -Pepto-bismol: has bismuth-subsaliylate |
|
|
|
Aspirin Toxicity Clinical Signs
|
-Vomiting
-Hyperventilation (aspirin is an acid, compensatory respiratory mechanism to blow off excess CO2) -Fever -Hypo or hyperglycemia -metabolic acidosis (BIG DEAL) -Cats are more susbeptible than dogs --saturation of elimination pathways --NO safe dose of aspirin for cats -Dogs and cats are at risk for gastric ulcers -Dog therapeutic dose: 10-20 mg/kg q48 hours |
|
|
|
Aspirin Toxicity Treatment
|
-Decontamination
-Symptomatic supportive care -Sodium bicarbonate for ion trapping --treat metabolic acidosis --helps with elimination of acid --helps increase pH --Alkalizes urine (make sure patient is not hypokalemic) |
|
|
|
Seizing from Aspirin
|
-Due to Aspirin crossing BBB
-Once crosses BBB, cannot get back across -Reduce with Sodium bicarbonate infusion |
|
|
|
Antitussives
|
-Opioids
-Dextromethorphan --hits a lot of receptors, acts like opioid and PCP |
|
|
|
Expectorants
|
-Guaifenesin: mucolytic, breaks up mucus
-Causes a lot of stomach upset -Animal will be vomiting and sick, but not deadly ill |
|
|
|
Alpha-2 agonists
|
-Clonidine: anti-hypertensive, opioid addiction treatment, ADD treatment
-Visine: imidazoline decongestant -Alpha-2 stimulant effects |
|
|
|
Alpha-2 agonist Toxicity Clinical Signs
|
-CNS depression
-Bradycardia -Hypotension with central alpha-2 stimulation -Hypertension with peripheral alpha-2 stimulation -Miosis |
|
|
|
Alpha-2 agonist Toxicity Treatment
|
-Decontamination
-symptomatic supportive care -Naloxone: reduces endogenous opioid release --can reverse coma and hypotension --can't hurt! |
|
|
|
GI Preparations
|
-Antacids
-Laxatives -Anti-diarrheals |
|
|
|
Antacids
|
-Aluminum hydroxide
-Magnesium hydroxide -Calcium carbonate -MINIMALLY toxic |
|
|
|
Laxative Toxicity
|
-Major concern is fluid and electrolyte losses
-Sodium phosphate enemas can cause hyperphosphatemia, hypernatremia, dehydration, and shock --serious electrolyte abnormalities -Toxicity reported with rectal use and ingestion |
|
|
|
Anti-diarrheal toxicity
|
-Kaolin-pectin: no longer available
--was safe for animals, now has salicylate in it -Lamotil: anticholinergic/opioid --narrow margin of safety for animals -Bismuth subsalicylate: pepto-bismol, kaopectate products --form of aspirin! -Loperamide: opioid-like efects |
|
|
|
Loperamide toxicity
|
-Anti-diarrheal medication
-Can have opioid-like effects -Naloxone may be effective as antidote -Therapeutic dose exists, but is very small -Causes GI issues, opioid effects, constipation, drowsiness |
|
|
|
Treatment for Anti-diarrheal toxicity
|
-Decontamination
-Sympotmatic supportive care -Naloxone for diphenoxylate (lomotil) and loperamide (imodium) |
|
|
|
Zinc Oxide Toxicity
|
-Strong GI irritant
-Can have Zn toxicosis with a HUGE amount or chronic ingestion --need lots of tubes -Treatment: supportive care |
|
|
|
Vitamin A and D Ointment toxicity
|
-Minimal risk
-Stomach upset, vomiting and diarrhea (usually mild) --due to emollient base |
|
|
|
Calcipotriene Toxicity
|
-Synthetic analog of Vitamin D3
-Rx cream for human psoriasis -Can be deadly! -Not a big deal topically, but orally can be a major issue -Hypercalcemia, soft tissue mineralization, renal failure -CNS depression -Vomiting, CNS depression, anorexia, diarrhea, polyuria |
|
|
|
Treatment for Calcipotriene Toxicity
|
-Decontamination
-Treat elevated Ca and P -Give bisphosphontes (aredia) to lower Ca -Supportive care to prevent renal failure -May have to treat for weeks -Death can occur after weeks of apparent recovery --secondary to calcification of cardiac tissue |
|
|
|
5-Flurouracil Toxicity
|
-Used for human keratoses and superficial basal cell carcinomas
-Rapidly absorbed with ingestion -Low margin of safety -Half of a tube is lethal to a 70lb dog! -Causes severe seizures -Vomiting and GI mucosal sloughing -Delayed severe leukopenia -Toxicity if ingested and with dermal application -Prognosis is poor due to seizures |
|
|
|
5-Flurouracil Toxicity treatment
|
-Seizures rarely respond to diazepam
--can try barbiturates, iso, propofol -Filgrastim for severe leukopenia -Weeks of monitoring may be required due to delayed leukopenia |
|
|
|
Things that are dangerous in small amounts
|
-Oil of Wintergreen
-Lomotil -Ca channel blockers -Imidazoline decongestants -Clonidine -Oral hypoglycemics -Beta blockers -Toxic alcohols |
|
|
|
Things that are dangerous in small amounts in Dogs
|
-NSAIDs
-Pseudoephedrine -Caffeine -Albuterol |
|
|
|
Things that are dangerous in small amounts in Cats
|
-Acetaminophen
-Benzocaine -NSAIDs -ASA -Oxidant drugs that induce heinz body formation |
|
|
|
Thing that are dangerous in small amounts in Dogs And Cats
|
-5-fluorouracil
-Calcipotriene -Isoniazid |
|
|
|
Herbal Preparation
|
-Dietary Supplement which may be derived from plant or non-plant materials
-Can be raw or extractions of plants |
|
|
|
Homeopathic Preparations
|
-law of similars: like treats like
--theory is to get body's own mechanisms to respond -Law of Infintesimals: the more diluted the remedy the more potent it is --10x is 10x dilution |
|
|
|
Animal exposure to herbal remidies
|
-can be accidental
-Can be used under the assumption that "natural" products are "safe" -Can be used due to frustration with traditional remedies |
|
|
|
Herbal Regulations in US
|
-Not a lot
-Herbal remedies can reach consumer without independent pre-market assessment of quality and safety -Inadequately tested medications are being marketed as dietary supplements, NOT medications -Role of the FDA is to regulate label claims of dietary supplements --must prove that the product is unsafe to be removed |
|
|
|
Dietary Supplement health and Education Act of 1994
|
-Pre-marketing efficacy and safety or adverse events are not required to be reported
-Label cannot say that preparation treats a specific disease -Label can say that a supplement supports a specific system -1999: need listing of contents, fact panel, and manufacturer contact info -2000: no claims related to pregnancy on the product |
|
|
|
Contraindications for Herbal Use
|
-Kidney disease: licorice root and parsley
-Autoimmune Disease: echinacea, reishi and maitake, mushrooms, astragalus --do not need additional immune system effects! -Liver Disease: eucalyptus -Thyroid disease: kelp, bugleweed |
|
|
|
Parsley
|
-Can be used for cancer growth inhibition, "detoxifier"
-Digestion stimulant, treatment for bad breath -Can irritate and damage the renal epithelium |
|
|
|
Licorice Root
|
-Can be used for stomach upsets, diarrhea, and reflux
-Has mineralocorticoid effects --Na and H2O retention --K loss -Bad for patients with renal dysfunction |
|
|
|
Eucalyptus
|
-Used for respiratory tract inflammation
-Induces liver enzyme activity --do not know how much it induces liver enzyme activity -Use with caution in patients with liver disease |
|
|
|
Kelp
|
-May contain iodine
-Can adversely affect thyroid function -Hard to titrate |
|
|
|
Bugleweed
|
-Can cause dangerous decrease in thyroid function
-Hard to titrate and know exactly how much patient is getting |
|
|
|
Pyrrolizide Alkaloids
|
-Over 60 plants used medicinally contain pyrrolizidine alkaloids
-Can cause hepato-occlusive disease, LIVER disease -Hard to figure out how much to use safely --Depends on time of year, developmental stage of the plant, location of the plant --storage and length of storage can affect toxicity |
|
|
|
Factors contributing to Herbal Toxic Reactions
|
1. Time of year of harvesting
2. Developmental stage of the plant 3. Location of the plant 4. Storage and conditions of storage 5. Misuse or misunderstanding label 6. Compounding error 7. Misidentification of Plants 8. Dangerous substitiutions (contains dangerous things it should not) 9. Confusing terminology (sounds like something that is not dangerous) 10. Adulterants and contaminants |
|
|
|
Common herbal adulterants and contaminants
|
-Aspirin
-Barbiturates -Corticosteroids -Viagra -Non-US approved medications -Colchicine -Scopolamine -Heavy Metals -Hepatitis E -Listeria |
|
|
|
Allergic Reactions with Herbals
|
1. Royal Jelly
2. Chamomile |
|
|
|
Royal Jelly
|
-Can cause severe bronchospasm
|
|
|
|
Chamomile
|
-Can cause anaphylaxis
-Severity of reaction is not proportional to the severity of allergy to ragweed |
|
|
|
Herb-drug Interactions
|
-Testing is not done to identify interactions
-Most suspected drug-herb interactions are identified via case reports -Garlic: Warfarin, causes increased bleeding -Ginkgo Bilboa: warfarin, increases bleeding --aspirin: increases bleeding -Ginseng: warfarin, decreases clotting activity -Kava: alprazolam, causes additional sedation -St. John's Wort: --paroxetine, serotonin syndrome --Warfarin, decreased clotting activity --Digoxin, reduced plasma concentration |
|
|
|
Pennyroyal Oil
|
-Oral aborifacient
-Digestive tonic -Diuretic -Topically used as insect repellant and antiseptic -Depletes hepatic glutathione levels -Damage to target cellular proteins -large doses can cause miscarriage, irreversible kidney damage, hepatic damage, death -Topically can cause rash and dermatitis -Causes |
|
|
|
Pennyroyal Oil Toxicity
|
-Humans: 10-15ml can cause death
--less than a teaspoon causes seizures -Canine death following use as a flea repellant |
|
|
|
White Willow Bark
|
-May have analgesic, anti-inflammatory and anti-pyretic effects
-Inhibits platelet aggregation but less than aspirin -Used for pain, fever, common cold -basically the same thing as aspirin |
|
|
|
White willow Bark Toxicity
|
-Same as aspirin
-GI upset -Salicylate poisoning (CNS toxicity, acid-base disturbances, fluid and electrolyte imbalances, coagulopathy) -Cats are especially susceptible -Clinical signs: CNS depression, vomiting, GI hemorrhage, hyperpnea, pyrexia |
|
|
|
White Willow Bark Toxicity Treatment
|
-Decontamination
-Symptomatic supportive care |
|
|
|
Garlic Toxicity
|
-Inhibits platelet function
-Increases fibrinolytic activity -Decreases blood-lipid levels -Lowers blood sugar -Used to treat infections, HW, flea repellant, general health tonic -Affects GI system and hematopoietic system -Toxicity causes GI irritation and platelet dysfunction |
|
|
|
Garlic Toxicity key clinical signs
|
-GI upset, bleeding
-Treat with decontamination and symptomatic supportive care |
|
|
|
Tea Tree Oil
Melaleuca |
-Unknown mechanism of action
-Used for antibactierial, antifungal, antipruritic, insect repellant -Do not want to use in pure form, NEVER use straight! -need to know what the strength is -Affects CNS, GI, skin -Causes CNS toxicity? |
|
|
|
Clinical signs of Tea Tree Oil toxicity
|
-Ataxia
-Incoordination -Weakness -Tremors -Altered behavior -Treat with decontamination and symptomatic supportive care |
|
|
|
Comfrey
|
-Binds to proteins, DNA, and RNA
-Causes cell damage and death -May be carcinogenic -Used for topical wound healing, GI upset, joint inflammation, cough, cancer |
|
|
|
Comfrey Toxicity
|
-Hepatic failure!
-Can be absorbed in quantities that will cause toxicity with extended use or high concentrations -Treatment: decontamination and symptomatic supportive care --Early NAC administration may be beneficial |
|
|
|
St. John's Wort
|
-Inhibits monoamine oxidase and serotonin reuptake
-Topically inhibits epidermal inflammatory response -Used for anxiety, depression, phobias, and topical anti-inflammatory -Affects skin and CNS -Same activity as SSRIs and MAO inhibitors, but do not know the concentration -Has many drug interactions -Treat toxicity with decontamination and symptomatic supportive care |
|
|
|
Kava kava
|
-Acts as a central dopaminergic receptor antagonist
-Local anesthetic -Used for anxiety -Affects CNS and liver -Case reports associates with hepatic failure |
|
|
|
Kava Toxicity
|
-Ataxia
-Sedation -Extrapyramidal effects -Jaundice -Fatigue -Treat by decontamination and symptomatic supportive care |
|
|
|
Hops
|
-Antimicrobial activity
-Inhibits smooth muscle spasticity (unclear mechanism) -Use for anxiety and sleep disorders -Affects CNS -Can cause sedation and hyperthermia |
|
|
|
Common herbs that are dangerous to animals in small doses
|
1. Pennyroyal
2. White Willow Bark 3. garlic 4. Mah-wang |
|
|
|
What to do with an unknown herbal toxicity
|
1. Evaluate need and safety for GI decontaminatino
2. Symptomatic and supportive care 3. Laboratory testing might not be useful, difficult to detect herbs |
|
|
|
Summary of Herbal Preparations
|
-Under-regulated
-Considered "dietary supplements" -Increases risk for contaminants -have unlisted ingredients -Variable dosing of active ingredients |
|
|
|
Melamine Contamination
|
-Contamination of corn gluten feed and infant formula
-Imported from China |
|
|
|
Moldy Sweet Potato Waste
|
-Caused 200 cattle deaths
-Cows fed moldy sweet potatoes -Contained mold toxin produced by Fusarium solani |
|
|
|
Feed factors that can cause toxicosis
|
-Natural factors within the feed
-Chemical concentration in plants -Exposure on pasture from inappropriate disposal of trash -Inappropriate mixing of feeds |
|
|
|
Natural sources of Toxic Factors in feed
|
-Plant species: concentrate toxic factors
--heavy metals concentrated -"Natural" products in plants for protection against insecticides |
|
|
|
Human error as source of toxins in feed
|
-Feed additives added in excess
-Feed additives given to wrong species -Animals introduced to recently fertilized pasture -Contaminants in the environment -Chemical insecticides or herbicides inappropriately mixed into feed --animals allowed inappropriate access to herbicides/insecticides |
|
|
|
Infestation of feed before or after harvest
|
-Mycotoxins
-Bacterial toxins |
|
|
|
Diagnosis of a Feed Toxicosis
|
1. History: multiple animals in a group
-peracute condition that affects many animals in a herd 2. Sudden onset, spreads over time --increasing deaths with increasing time 3. Clinical signs and physical exam 4. Post-mortem exam 5. Clinical toxicology 6. Feed analysis! |
|
|
|
Physical exam of animal with Feed Toxicosis
|
-Look at all animals affected
-Get history -Most difficult thing can be the sampling of the feed --need a representative sample --toxic event may be over, feed has already been ingested |
|
|
|
Common Feed Toxicosis
|
-Mycotoxins: products of mold
-Urea: nitrogen toxicosis in ruminants -Monensin toxicosis -Nitrate/Nitrate toxicosis -Botulism -Chemical contamination of feeds and pastures -Heavy Metals: mercury, fluoride, zinc, copper, chromium, selenium -Gossypol: whole cotton seeds, cotton seed meal |
|
|
|
Representative Sample of Feed
|
-Mix 10 samples of feed in a bucket, use 1lb to sample and 1 lb to send out
|
|
|
|
Mycotoxins
|
-Toxin produced by organism in fungi (mushroom, molds, yeasts)
-Aspergillus, penicillium, fusarium, claviceps -300-400 types identified -Major toxins: aflatoxin, deoxynivalenol, fumonisins, zearalenone, ochratoxin, T2 toxin, ergot |
|
|
|
Major Mycoplasma Toxins
|
-Aflatoxins
-Deoxynivalenol (vomatoxin) -Fumonisins -Zearalenone -Ochratoxin -T2 toxin -Ergot |
|
|
|
Mycotoxin and performance
|
-Huge range in clinical syndromes, can be nothing or can be death
-Can have HUGE effect on performance -Low resistance to disease -Poor eating, poor producing animals -Reproductive failure and abortions -Embryonic death -Teratogenic effects -Can cause kidney, liver, GI tract, heart, brain, lung organ system failure -Disrupts endocrine, exocrine, cellular functions |
|
|
|
Mycotoxins as carcinogens
|
-One of most carcinogenc agents known
-Aflatoxin especially |
|
|
|
Growing Mycotxins
|
-Depends on environmental conditions
--heat, humidity -Depends on species |
|
|
|
Fungal infestations in the field
|
-Stressful conditions (drought)
-Insect damage -Bird damage -Humidity, temperature, and seasonal influences are all based on individual toxin species -Situations that weaken seed integrity, allow mold spores to enter seed and grow -Presence of mold does not mean toxins will be produced |
|
|
|
Storage conditions allowing Mold growth
|
-16-30% moisture in grain
--more than 30% moisture favors bacterial growth -Warm storage temperatures -Oxygen and CO2 concentrations --mold likes oxygen! --Storage conditions tend to displace and decrease oxygen |
|
|
|
Fescue grasses
|
-Contain mold spores in the ovary of the seed
-When plant goes to mature, mold is already present in the seed -Can purchase endophyte-free grass seeds |
|
|
|
Grains having multiple toxins
|
-Conditions that allow mold to grow can result in many mold species
-Any given toxin might not be toxic on own -Combination of toxins can be very dangerous, cumulative effect -Grains are screened |
|
|
|
Ruminant Resistance to Toxins
|
-Ruminants have slightly more resistance due to rumen degradation of toxins
-Poultry and swine are more susceptible |
|
|
|
Preharvest control of Mycotoxins
|
-Manage and put fungicides on crops
-Dry grain at harvest, make sure correct dry matter -Use drying ovens to create better storage environment |
|
|
|
Mixing wet and dry grains
|
-Bad news!!
-Dry grains become wetter --mold creates metabolic water with growth, makes grains wetter with time |
|
|
|
Methods to reduce mycotoxin load in grain
|
1. Do not mix wet and dry grains
2. Destroy aflatoxin molecule before feeding 3. Prevent absorption in GI tract 4. Do not feed contaminated grain! duh. 5. Dilute contaminated grain for feeding on-farm --cannot be sold |
|
|
|
Destroying aflatoxin before feeding
|
-Ammoniation disrupts molecule
-Acid or alkali treatments -Irridation -Heating (not a safe method, many are not susceptible) -Not commonly done due to cost |
|
|
|
Prevent toxin absorption in gut
|
-Chemisorbents, yeasts, enzymes
-Hydrated sodium calcium alumino silicates -Activated charcoal -Clay with cationic surfaces, binds toxins -Yeasts with poly-saccharide rich cell wall to bind toxins and prevent absorption |
|
|
|
Aflatoxins
|
-made by Aspergillus mold species
-Regulated by FDA due to ability to produce cancer in humans -Feeds: cotton seeds, corn, oil seeds, peantus -B1 toxin is very common -toxin metabolites are passed in milk -Toxin is produced during pre and post harvest production --drought, insect and bird activity increases toxins --wet grains, 20-25% moisture, temps 25-35 |
|
|
|
Clinical signs of Aflatoxin toxicity
|
-Poor performance
-Reduced feed intake -Poor resistance to infection -Heaptic cirrhosis -Carcinomas (VERY carcinogenic!) |
|
|
|
Aflatoxin regulation
|
-Needs to be less than 20 ppb in feed
-Less than 0.5 ppb in milk -LD50 is 0.5-10 mg/kg in all species |
|
|
|
Fusarium Toxins
|
-Deoxynivalenol and Trichothecenes
-Zearalenone -Fumonisin |
|
|
|
Deoxynivalenol and Trichothecenes
|
-Fusarium toxins
-pigs are sensitive -causes vomiting, feed refusal, diarrhea, mucosal hemorrhage -Limited to 5ppm in total ration for cattle over 4 months |
|
|
|
Zearalenone
|
-Fusarium toxin
-Associated with moldy corn and barley -Has estrogenic effect --Causes vulvo-vaginitis and infertility --inhibits development of embryo after day 15 -Results in reduced litter size and infertility -Swine are very susceptible |
|
|
|
Fumonisin
|
-Fusarium toxin
-Horses are sensitive --causes equine leukoencephalomalacia in horses --"moldy corn disease" -Regulated to be Less than 30 ppm in diet |
|
|
|
Ochratoxin and Citrinin
|
-Produced by aspergillus and penicillium species
-Grows on stored barley and corn --too wet at storage allows growth -Renal toxin, can cause kidney disease -Causes immunosupporession -Can have teratogenic effects, cause resorption of the embryo -Carcinogen -Pigs are most sensitive -0.25 ppm in total feed |
|
|
|
Ergot Alkaloids
|
-Endophyte fungus in tall fescue
-Associated with endophyte infected seed heads -Prevent by grazing fescue and rye grass before it has gone to seed or buying seeds that are fungus free -Rye grass Staggers -Cause gangrene, sloughing of extremities, tails, hooves, etc. -can lead to Strep agalactiae, will cause shut-down in milk production -Causes hyperthermia |
|
|
|
Lupine
|
-Lupine stubble is the issue
--dry foliage with seed pods, or if it has been rained on -Once develops to seeds, if it gets wet mold can grow in seeds -Causes hepatic issues |
|
|
|
Ipomeanols
|
-Fusarium toxin
-Moldy potatoes -Causes acute bovine pulmonary emphysema |
|
|
|
Tremorgens
|
-Penicillium
-Aspergillus -Causes staggers, muscle tremors, recumbency -Affects sheep and ruminants |
|
|
|
Gossypol
|
-Natural component of cotton seeds
-Protects plant from insect activity -Contained in tiny resin glands within the seed head -Concentration varies with different species of cotton seeds |
|
|
|
Gossypol Toxicosis
|
-Swine and humans and poultry are particularly sensitive
-Myocardial toxin, causes myocardial degeneration and heart failure -Causes liver toxicity also -Keep at less than 100 ppm in swine and poultry feed |
|
|
|
Ruminants and Gossypol
|
-Ruminants can detoxify gossypol
-Can have in diet -Gossypol binds to soluble proteins in the rumen --inhibits absorption -Calves can be susceptible -Adult cows can be affected over a certain amount --abomasitis, hemoglobinuria, respiratory distress -Keep at less than 400 ppm |
|
|
|
Diet to prevent Gossypol toxicosis
|
-iron sulphate
-lysine -protein -vitamin E |
|
|
|
Nitrate vs. Nitrate N
|
-Nitrate N= Nitrate Nitrogen
-Nitrate N= .23 nitrate -Have to be careful when reading reports and looking at values Nitrites are more toxic than nitrates |
|
|
|
Sources of Nitrates
|
-Plants concentrate nitrates, especially in drought conditions
--pigweed, lamb's quarter, jimson weed, fireweed, johnson grass -Water-stressed plants take up nitrogen, but cannot convert it into proteins -more concentrated in the proximal portions of the plant --stems, trunks, etc. -Nitrates in the water is BAD news |
|
|
|
Nitrate Toxicity
|
-Nitrite Can easily enter RBCs in exchange for Cl
--oxidizes Hb to form methemoglobin and nitrate --Inhibits O2 carrying capacity, causes hypoxemia (respiratory distress) -Nitrate levels higher than 15,000 ppm are toxic to cattle and sheep -Cattle can tolerate large amounts, use as nitrogen source for bacteria in rumen, produce baterial proteins |
|
|
|
Treatment for nitrate toxicity
|
-Methylene blue IV
-Reducing agents |
|
|
|
Syndromes associated with non-protenated Notrogen
|
-Sudden death from ammonia toxicity
-Subclinical toxicosis leading to impaired fertility -Ammoniation of forage "bovine bonkers" -Environmental contamination, nitrate in ground water --Eutrophication of ground water |
|
|
|
Nitrogen in Diets
|
-Ruminants can utilize up to 40% of protein and Non-protein nitrogen
-Crude protein= Nitrogen * 6.25 --estimate of crude protein content --most AA contain 16% nitrogen |
|
|
|
Rumen Metabolism
|
-Non-protein Nitrogen is converted to ammonia in the rumen
-Enzymatic conversion via urease (rapid conversion) -Chemical conversion is slower, dissociation -Bacteria can capture 25-35g of nitrogen per kg of fermentable organic matter --determines how much NPN can be put into the diet -Not enough fermentable organic matter, or too much NPN, ammonia is absorbed across the rumen wall --Ammonia enters portal circulation and liver has to detoxify --can overwhelm the liver above 1.0 mg/dl (start to see clinical signs) |
|
|
|
Risk factor for Nitrogen Toxicosis
|
-Based on the form of the ammonia
-NH3: un-ionized form, is more quickly absorbed -rumen pH less than 7.0 favors NH4, slows absorption -Rate of ammonia generation is rapid with urea sources --urease breaks down urea quickly -Amount of NPN n the diet has big effect -Animals can be adapted to NPN |
|
|
|
Sources of NPN
|
-Urea (1g/kg LD)
-Biuret (8 g/kg LD) -Ammonium sulfate (3 g/kg LD) -Anhydrous ammonia -Fertilizers -Fermented silages -Lush pastures, recently fertilized pastures |
|
|
|
Adaptation to NPN
|
-To efficiently use ammonia from NPN, have to adapt animals
-Takes 5-7 days of exposure to high NPN levels to adapt animals -Adaptation can be lost in 2 days if feeding is stopped -Rapid introduction of high levels of NPN can be fatal |
|
|
|
Clinical signs of Ammonia toxicity
|
-Dead animals
--mistake in feeding, animals die -Living animals: --muscle tremors --restlessness, incoordination, weakness --rapid respiration, cyanosis, jugular pulses --cardiac arrhythmias --Hyperthermia --Excitable --bellowing, colic --rumen atony and bloat |
|
|
|
Blood ammonia with Ammonia toxicity
|
-More than 1.0 mg/dl
-Death if ammonia level gets higher than 2 mg/dl -Subclinical toxicity at 0.4 - 1.0 mg/dl |
|
|
|
Ammonia Toxicity Diagnosis
|
-History can give an idea
-Feed analysis for NPN -Blood levels are not very useful unless within 12 hours of death -Can test CSF for ammonia -Rumen fluid is not helpful, even after death will have bacterial breakdown of proteins |
|
|
|
Differential Diagnoses for Ammonia Toxicity
|
-Nitrate toxicity
-Respiratory distress -Bovine Bonkers -Cyanide or lead toxins -Peracute infection -Grain overload, rumen acidosis |
|
|
|
Treatment for Ammonia toxicity
|
-Large volumes of cold water
--slows urease enzyme activity --give 20L -5% acetic acid (white vinegar), converts NH3 to NH4 and slows absorption --2-6L in cattle --0.5-1L in sheep -Rumenotomy in extreme situations --not practical if herd outbreak |
|
|
|
Etiology of Ammonia Toxicity
|
-Exposure to NPN with no adaptation
-Errors in mixing feeds -Exposure on pasture within a week of being fertilized -Acclimated cattle can tolerate 1g urea per kg -Unacclimated cattle can tolerate less than 0.45g urea per kg -Rapid onset of breakdown --20-60 min in cows --30-90 min in sheep --longer in horses |
|
|
|
Ammonia toxicity prevention
|
-Limit NPN to 1/3 of total crude protein required in diet
-3% urea max, 1% of total ration --total intake less than 0.5g/kg -Biuret should be 3% of grain or less -Ammonium salts 0.75-1.5 oz per head per day |
|
|
|
Bovine Bonkers
|
-Ammoniation of high-quality forage, ammonia forms with tryptophan
-2-methylinidazole, 4-methylindazole, and pyrazine compounds are formed from tryptophan -Becomes toxic factor |
|
|
|
Preventing Bovine Bonkers
|
-Do not use more than 3% ammonia in feed
-Cool temperatures -Less than 20% moisture in feed (hay) -Low quality forage |
|
|
|
Pest
|
-Living organisms that occur where they are not wanted
-Can cause damage to crops, humans, or other animals -Insects -Mice, rodents -Unwanted plants, weeds -Fungi -Microorganisms (bacteria, viruses) -Prions |
|
|
|
Insecticides
|
-5 billion pounds used in US every year
-Exposure is very common -Insecticides change often due to development of resistance -Change also due to increasing efficacy and decreasing adverse effects to unintended hosts |
|
|
|
Common insecticides
|
-Organophosphates
-Carbamates -Pyrethrins and pyrethroids -Metaldehyde -Ivermectin (macrolide endectocides) |
|
|
|
Organophosphate Insecticides
|
-Still widely used in agriculture
-Topical application to plants, animals, soils, floors -Systemic administration: absorbed by plants or animals --affect insect when it feeds or inhales -Previously in some flea collars, not anymore |
|
|
|
Organophosphate Sources of Exposure
|
-Livestock feedstuffs contaminated from crop use
-Improper use on crops or animals -Malicious use to poison animals --wildlife -Secondary/relay toxicosis |
|
|
|
Organophosphate ADME
|
-Occurs very quickly! Clinical signs are apparent very soon after exposure in patients
-Rapid absorption from body surfaces (skin, respiratory tract, GI tract) -Rapid distribution and metabolism -Rapid excretion via urine -Toxicity is variable |
|
|
|
Organophosphate Mechanism of Toxicity
|
-Inhibition of cholinesterase enzyme
-prevents breakdown of ACh in synaptic cleft -Binds ACh-esterase, and causes irreversible process --"Aging" -ACh concentrations increase and causes continuous stimulation of nervous, glandular, and muscular receptors |
|
|
|
Cholinesterase Enzymes
|
1. Acetylcholinesterase: "true" cholinesterase
-Specific to ACh -In RBCs, brain, retina, NMJs -Responsible breakdown for ACh 2. Butyrlcholinesterase: "pseudo" cholinesterase -Less specific -Present in plasma, liver, pancreas, CNS |
|
|
|
ACh breakdown
|
-Broken down in synaptic cleft by ACh-esterase
-Broken down into choline and acetic acid --Choline is taken back up by presynaptic neruon -In process of breakdown, ACh-esterase becomes acetylated temporarily |
|
|
|
Carbamate Mechanism of Action
|
-Binds to ACh-esterase and prevent breakdown of ACh in the synaptic cleft
-Binding is reversible, breaks down eventually -Breakdown takes longer than normal ACh --half-life is longer -ACh concentration increases, causes continuous stimulation of nervous, glandular, and muscular receptors |
|
|
|
Systems using ACh as NT
|
1. Parasympathetic: (Muscarinic)
--pre-ganglionic --post-ganglionic 2. Sympathetic: --Pre-ganglionic (nicotinic) --post-ganglionic at sweat glands (muscarinic) 3. Somatic: --pre-ganglionic (nicotinic) 4. CNS: --Pre-ganglionic (central) |
|
|
|
Organophosphate Aging Process
|
-Allows for irreversible binding of organophosphate to ACh-esterase
-Enzyme becomes permanently inactivated |
|
|
|
Carbamate and Organophosphate Mechanism of Toxic Action
|
-Inhibits cholinesterase
-Individual organophosphates and carbamates vary in affinity and reversibility -Implications for treating intoxicated oatients |
|
|
|
Carbamate Antidote
|
-Pralidoxime chloride (2-PAM)
-Reactivates ACh-esterase enzyme if given in time -Binds to enzyme and removes toxin from enzyme -If given after aging (with organophosphate toxicity) will not have any effect |
|
|
|
Clinical signs of Muscarinic Toxicity
|
-Toxicity is affecting parasympathetic nervous system
-Can be from insecticide (carbamate or organophosphate) -DUMBELS -Diarrhea -Urination -Miosis -Bronchospasm and bradycardia -Emesis (vomiting) -Lacrimation -Salivation |
|
|
|
Clinical signs of Nicotinic toxicity
|
-Toxicity if affecting sympathetic nervous system
-Can be from insecticide (carbamate or organophosphate) -Muscle tremors -Tetany -Weakness |
|
|
|
Clinical signs of CNS toxicity
|
-Can be due to organophosphate or carbamate toxicity
-Anxiety -Seizures -Depressed respiration -Coma |
|
|
|
Death in organophosphate/carbamate toxicity
|
-Death is usually due to hypoxia
--respiratory tract secretions --bronchospasm -Respiratory depression and paralysis -Cannot get enough O2 to tissues |
|
|
|
Organophosphate/Carbamate toxicity Diagnosis
|
-History and clinical signs
-Necropsy should not have any gross lesions, no specific lesions -Measure ACh-esterase activity to assess exposure -Detect specific insecticides in tissues or GI contents -See how animal responds to Atropine |
|
|
|
Measuring ACh-esterase activity to diagnose Organophosphate/Carbamate toxicity
|
-run on whole blood in mammals
-if activity is less than 50% of normal: suspicious of toxicity -activity is less than 25% of normal: diagnostic of toxicity -Enzyme activity may return in animals with sun-lethal exposure |
|
|
|
Atropine for Organophosphate/Carbamate toxicity
|
-Atropine can inhibit muscarinic signs
-Non-competitive antagonist at ACh receptors -Prevents accumulating ACh from having an effect at receptors -Can make patients look better clinically -Have to give very high doses to have an effect |
|
|
|
Organophosphate/Carbamate toxicity Treatment
|
-Atropine for clinical signs (not long-term)
--may need high dose -2-PAM (long-term) --will work for carbamates, probably will not work for organophosphates unless caught early -Emesis (often vomit on their own) -Activated charcoal -Bathe if dermal exposure -Supportive care -Lipid therapy? |
|
|
|
Summary of Organophosphate and Carbamate Toxicity
|
-ACh-esterase inhibition
-parasympathetic nerve stimulation (muscarinic): DUMBELS -Somatic neuromuscular junctions: muscle tremors, paralysis -CNS: seizures, coma -Diagnose based on history and clinical signs --measure whole blood ACh-Esterase activity -Treat with atropine, 2-PAM and supportive care |
|
|
|
Pyrethrins/Permethrins and Pyrethroids
|
-Derived from chrysanthemums
-Used as spot-on treatment for fleas and ticks on DOGS -NOT safe for cats! -Fat-soluble toxin, rapidly ADME -Pyrethroids have enhanced stability and potency -Toxicity is variable, can be less than 100 to more than 2,000 mg/kg needed for toxicity -Cats are very sensitive -Toxicity can be enhanced by synergistic components in compound -Toxicity usually occurs due to misuse or exposure in sensitive species |
|
|
|
Pyrethrin Mechanism of Toxic Action
|
-Action on Na channels
-Enhance inwards Na current into axons -Causes repeated depolarization of membrane, repeated firing of neuron -Can also enhance NT release |
|
|
|
Pyrethrin Clinical Signs
|
-Can be very variable
-Start within minutes of exposure due to rapid ADME -Can last for up to 3 days -Minor: hypersalivation, paw-flicking, ear twitching, hyperesthesia, reduced activity --single episodes of vomiting/diarrhea -Major: long-term vomiting and diarrhea --marked depression, ataxia, muscle tremors --rarely leads to seizures and death --Muscle tremors are the big thing -Animal can present as hyperthermic from excessive muscle activity -Requires immediate veterinary care!! |
|
|
|
Pyrethrin Toxicity Diagnosis
|
-Detect pyrethrin toxin in tissue
-Mostly based on clinical signs and history -Pathology is not helpful |
|
|
|
Pyrethrin Toxicity Treatment
|
-Standard GI decontamination for oral exposure
-Bathe if dermal exposure -Methocarbamol IV for muscle tremors (muscle relaxant) --does have maximum dose, can cause severe respiratory depression with too much -Control seizures and muscle tremors (valium, barbiturates) -Lipid therapy -Prognosis is good in owner can afford hospitalization and treatment |
|
|
|
Complications with Pyrethrin Toxicity treatment
|
-Hyperthermia due to excessive muscle tremors
-Lactic acidosis -Hypoxia |
|
|
|
Intra-Lipid
|
-Give lipid IV
-Lipid creates separate compartment in blood, toxin is contained in compartment --toxin cannot bind to anything, is excreted -Can help with cardiovascular signs -Has potential for bacterial contamination |
|
|
|
Metaldehyde
|
-Active ingredient in slug and snail baits
--can be up to 5% -Regional use -Baits are readily consumed, mostly by dogs -Some states require formulations to be unattractive to animals |
|
|
|
Metaldehyde Toxicity
|
-ALL neurologic effects
-Readily absorbed by GI tract -metabolized to acethaldehyde -Cross BBB and acts on GABA system --decrease GABA transmission --Decrease brain Serotonin and NorEpi --increase MAO activity -Range of lethal dose is very variable |
|
|
|
Metaldehyde Toxicity Clinical Signs
|
-"Shake and bake"
--Neurologic signs and hyperthermia -Tremors, seizures -Animal gets VERY hot -Mild clinical signs: anxiety, restlessness -Mydriasis, tremors, ataxia, colic in horses -Hyperpnea, tachycardia, opisthotonus, convulsions, hyperthermia, acidosis -Not generally hyperesthetic or hyper-reactive -No vomiting or diarrhea |
|
|
|
Metaldehyde Toxicity Diagnosis
|
-Based on history and clinical signs
-detection of metaldehyde in stomach contents -Can submit bait, stomach contents, serum, urine, liver for assessment -Check ACh-esterase levels to rule out organophosphate toxicity |
|
|
|
Metaldehyde Toxicity Treatment
|
-Supportive care
-Decontamination -Control seizures or muscle tremors -Mechanical ventilation if indicated -Control hyperthermia -Fluids -Sodium bicarbonate if animal is acidemic --will increase CO2 levels, use with caution! especially if patient has respiratory issues -Prognosis is good if treated early |
|
|
|
Amitraz
|
-Topical miticide used in flea collars for dogs
-NEVER use on cats or horses!! -Exposure is ususally via dog eating collar -Toxicity is variable -Clinical signs can be transient -Moderate absorption, 2-6 hours to see peak in blood levels -Works as alpha-adrenergic agonist and weak MAO inhibitor |
|
|
|
Amitraz Toxicity Clinical Signs
|
-Signs are related to CNS and cardiovascular effects
-Ataxia, depression, disorientation, polyuria, vocalization, seizures -Bradycardia -GI signs: emesis, diarrhea, anorexia -Non-specific lesions -Can be detected in tissues |
|
|
|
Amitraz Toxicity Diagnosis
|
-Lesions are non-specific
-Amitraz Can be detected in tissues |
|
|
|
Amitraz Toxicity Treatment
|
-Decontamination
--quick emesis may be enough to get toxin out of the system -Bathe the animal -intra-lipid therapy -Alpha antagonists --yohimbine, atipamizole |
|
|
|
Citrus Oil Extracts
|
-Derived from citrus fruit and peels
-Crude oil and refined products can be used to control fleas and ticks -Also used as food additives! -Dogs and cats are both susceptible |
|
|
|
Citrus Oil Toxicity Clinical Signs
|
-Related to CNS signs
--depression, hypothermia -May see salivation, skin irritation, tremors, skin necrosis -Clinical signs often resolve in 6-12 hours with supportive care and bathing |
|
|
|
Macrolides
|
-Ivermectin
-Selamectin -Abamectin -Doramectin -Milbemycin -Moxidectin -Eprinomectin -Used in a lot of HW products -Oral treatment for demodex |
|
|
|
Ivermetin Toxicity
|
-Relatively safe product!
--wide margin of safety -Only dangerous unless MDR1 gene mutation in collies and herding breeds |
|
|
|
MDR-1 mutation
|
-In collies and herding breeds
-Animal is missing the P-glycoprotein pump at BBB -Ivermectin can cross BBB and cannot be removed -Tortoises are also susceptible! |
|
|
|
Ivermectin Toxicity Clinical Signs
|
-Neurologic:
--ataxia, disorientation, hyperesthesia, hypersalivation --weakness -Blindness -Coma |
|
|
|
Ivermectin Toxicity mechanism of Action
|
-influx of Cl into neurons, causes hyperpolarization
-Prevents AP from transmitting |
|
|
|
Ivermectin Toxicity Treatment
|
-Lipid Therapy!
|
|
|
|
metals
|
-Metals are neither created not destroyed
-Tend to hang around, can cause problems in terms of toxicity -Pb is by-product of silver smelting -Arsenic is by-product of copper and tin melting -Cd associated with zinc carbonate as a contaminant |
|
|
|
Redistribution of Metals in the Environment
|
-Caused by geologic cycles, biological cycles, and human industry
-Can become bioconcentrated as they move up the food chain -Human activity alters the forms of metals --can alter/enhance transport and distribution on land, in water, in atmosphere |
|
|
|
Metals in Living Organisms
|
-Most metals affect multiple organ systems
-At low doses usually have target organ or organ system -Blood and urine can have metal biomarkers --give indication of exposure, toxicity, and susceptibility |
|
|
|
Dose-Effect Relationship of Metals
|
-Dose: amount of metal within cells of organs that manifests a toxological effect
--function of metal concentration and time -Single measurement can reflect either recent or long-term/past exposure -Biological half-life varies with metal and organ/tissue |
|
|
|
Metals in Blood and Urine
|
-Blood and urine concentrations of metals usually reflect recent exposures
-Correlate best with acute effects -Exception: urinary Cadmium --can reflect renal damage related to accumulations of Cd in the kidney |
|
|
|
Metals in Hair
|
-Hair levels of Mercury are reliable measure of alkyl or methyl mercury exposure
-Not always a reliable method for measuring exposure to most metals --External contamination may persist and complicate analysis, regardless of washing -Not the best method for testing, both dead and alive patients have other better methods for testing |
|
|
|
Targets of Toxicity
|
-Specific enzymes
-Specific membrane receptors of cells and organelles -Patterns of deposition and toxicity vary between organic and inorganic forms --Difference exists between organic and inorganic forms of metals! |
|
|
|
Essential Metals
|
-Essential metals and toxic metals can have similar metabolic pathways in the body
--Pb and Ca share homeostatic mechanisms -Inverse relationship between dietary protein content and Cd and Pb toxicity --toxicity increases as dietary protein decreases -Vitamin C increases ferrous Fe absorption -Vitamin C decreases absorption of Pb and Cd -Pb interferes with ca-dependent NT release |
|
|
|
Metal-Binding Proteins
|
-Proteins can be a target of toxicity
-Enzymes in particular can be a target -Proteins can play a protective role in toxicity --metallothioneins -Non-specific binding by serum albumin or Hb plays a role in metal transport and distribution |
|
|
|
Metallothioneins
|
-Low MW proteins
-Enable high-affinity binding with Cd, Cu, mercury, silver, and Zn --bind to both toxic metals and necessary metals -Highly inducible by numerous metals and stimulants --levels fluctuate in response to a need |
|
|
|
Metal Binding Proteins
|
1. Transferrin: Binds most of the ferric iron in plasma
--transports ferric iron across cell membranes via receptor-mediated endocytosis --also transports Aluminum and Manganese 2. Ferritin: storage form of Iron --in reticuloendothelial cells of liver, spleen, bone --also binds Cd, Zn, Beryllium, Al 3. Ceruloplasmin: copper-containing glycoprotein oxidase --converts ferrous Fe to ferric Fe, allows binding to transferrin |
|
|
|
Complexation
|
-Metal ion complex forms in which the metal ion is in association with a charged or uncharged ligand of some kind
-Electron is donated by Ligand |
|
|
|
Chelation
|
-Formation of stable ring structure
-Consists of metal ion and 2 ligand atoms -Makes metal not as available to be absorbed by target tissues |
|
|
|
Ideal properties of chelating Agents
|
1. Water soluble
2. Resistant to biotransformation, stays present in active form 3. Able to reach sites of metal storage 4. Capable of forming non-toxic metal complexes 5. Capable of being excreted 6. Low affinity for essential metals, esp Ca and Zn |
|
|
|
British Anti-Lewisite
BAL |
-2,3-dimercaptopropanol, dimercaprol
-Developed during WWII as antagonist for arsenical war gasses --arsenic binds to sulfhydryl-containing substrates -Able to chelate organic mercury, antimony, bismuth, chromium, cobalt, gold, nickel -Used as adjunct treatment of Pb encephalopathy --removes Pb from RBCs --can reach the brain |
|
|
|
Signs of BAL toxicosis
|
-vomiting
-Tremors -convulsions -coma -Death |
|
|
|
DMSA
|
-Chelation agent
-Chemical analog of BAL -PO administration, unique factor -Removes Pb from soft tissues -Greater specificity than EDTA, less excretion of Ca and Zn -Not effective in removing Pb from brain -Effective in dogs exposed to methyl mercury, Pb, arsenic |
|
|
|
EDTA
|
-Traditional chelator
-Ca salt, ethylene diaminetetraacetic acid -Greater affinity for Ca, will cause hypocalcemic tetany -Binds Pb and displaces Ca -Must be given parenterally -Not effective in reducing Pb in the brain -Potentially nephrotoxic -Often given in combination with BAL or DMSA, reduces risk of side effects |
|
|
|
Deferrioxamine
|
-Chelating agent
-Strong affinity for ferric (Fe3+), low affinity for Ca -Competes for iron contained in ferritin and hemosiderin -does NOT compete with transferrin, Hb, or heme-containing enzymes -Must be given parenterally -Has toxic effects: --hypotension, skin rashes, cataracts |
|
|
|
Penicillamine
|
-Chelating Agent
-Hydrolytic product of penicillin -Used for removal of Cu, Pb, mercury, and Fe -Side effects: --hypersensitivity reaction, skin rash, blood issues --leukopenia, eosinophilia, thrombocytopenia --Proteinuria, nephritic syndrome -Avoid in patients with penicillin hypersensitivity! |
|
|
|
N-Acetylcysteine
|
-Can be used as chelating agent
--also used for acetaminophen toxicity -Free radical scavenger -Precursor to glutathione -Forms water-soluble complexes with mercury and other metals --accelerates removal of methyl mercury -PO administration -Low toxicity -Widely available |
|
|
|
Arsenic
|
-Inorganic and organic forms
--Organic forms can be trivalent and pentavalent -Used to be used as pesticides -CCA treated lumber (copper, chromium, arsenic) --toxicosis with burning and ash formation |
|
|
|
Ant bait and Arsenic
|
-Sodium arsenate
-Potassium arsenate |
|
|
|
Drinking water and Arsenic
|
-Drinking water can be contaminated in abandoned mining areas
-Can contain elevated concentrations based on bedrock -Over 5 ppb is high concentration -Water is an important source of a toxicant! |
|
|
|
Trivalent Arsenicals
|
-Inhibit cellular respiration
-target tissues have high oxidative energy requirements --actively dividing cells of intestinal epithelium --epidermis --kidney, liver, spleen, lung -Also affects capillary integrity, unknown mechanism --capillary system of GI tract is most affected -Trivalent form is 10x more toxic than pentavalent form |
|
|
|
Pentavalent Arsenicals
|
-Uncouple oxidative phosphorylation
-Produces an energy deficit -No elevated body temp (unlike other forms of arsenic poisoning) |
|
|
|
Arsenic Hydride gas
|
-AsH3
-Can combine with Hb -Oxidized to a hemolytic metabolite -Not common |
|
|
|
Arsenic susceptibility in diferent species
|
-Cats are most susceptible to arsenic
-Horses -Cattle -Sheep -Swine -Birds -Organic arsenical feed additives have caused arsenic toxicosis in swine and poultry |
|
|
|
Arsenic as HW treatment
|
-Does not work!
-Thiacetarsamide, Caparsolate -Results in arsenic toxicosis in dogs |
|
|
|
Signs of Arsenic Toxicosis
|
-Severe GI effects
-Inorganic or organic trivalent arsenicals cause acute or peracute poisonings -Vomiting, intense abdominal pain -Weakness, staggering, ataxia, recumbency -Weak rapid pulses -Signs of shock -Animal is rapidly losing fluid into GI tract that is not intact like it should be -Rapid onset of watery diarrhea or rumen/GI atny -Kidney damage: oliguria, proteinuria, dehydration, acidosis, azotemia leading to death |
|
|
|
Arsenic chronic poisoning
|
-Rarely seen in domestic animals
|
|
|
|
Arsenic in Feed additives
|
-Organic pentavalent arsenical feed additives
-target nervous system --mild edema of the white matter in the brain and spinal cord --shrunken and degenerate neurons in the medulla -Cause signs within 2-4 days of overdose -Pigs: ataxia, incoordination, torticollis, blindness -"Dog-sitting" position -Eventually become paralyzed in lateral recumbency -Appetites and cognition stay normal -Causes GI irritation, mucosal congestion, submucosal edema, epithelial necrosis, massive fluid accumulation, atonic intestine |
|
|
|
Arsenic in People
|
-Can see increased levels in urine, vomit, feces, liver, and kidney
-Arsenic accumulates in epidermis and in the hair |
|
|
|
Arsenic poisoning treatment
|
-Emergency and supportive care
-Treatment for shock, acidosis, dehydration -Dimercaprol (BAL) antidote --ineffective if given before clinical signs begin -Succimer is preferred antidote -Feed animals bland diets, vitamin supplementation, reduced high-quality protein |
|
|
|
Arsenic Morbidity and Mortality
|
-Mortality is high in acutely poisoned animals
--with inorganic arsenicals -Pentavalent organic arsenical poisoning can give high morbidity and low mortality with good nursing care -Complete recovery may take 2-4 weeks |
|
|
|
Lead
|
-More than 90% of absorbed Pb is bound to RBCs
-Look for Pb bound to RBCs in whole blood -Specifically binds sulfhydryl groups -Inactivates enzymes involved with heme synthesis --causes RBC abnormalities -Damages membrane-associated membranes --Na/K pumps --results in RBC fragility and renal tubular injury -Results in shortened RBC lifespan and decreased RBC replacement |
|
|
|
Chronic Pb Toxicosis Clinical Signs
|
-ANEMIA!
-Binds to Sulfhydryl groups and inactivates enzymes involved with heme synthesis -Causes RBC abnormalities, damages Na/K pumps and results in RBC fragility and renal tubular injury |
|
|
|
Young animals and Pb
|
-Young animals absorb lead more readily than adults
-Absorption can be enhanced by deficiencies in Ca, Zn, Fe, vitamin D --make patients more susceptible to Pb |
|
|
|
Pb clinical signs vary by species
|
1. Ruminants: CNS dysfunction
--blindness --vocalizing 2. Horses: peripheral neuropathies 3. Dogs and cats: neurologic and GI signs 4. Birds: non-specific GI, neurologic, renal, hematologic abnormalities (anemia) 5. Waterfowl and raptors: chronic wasting and peripheral nerve dysfunction |
|
|
|
Pb Hematologic abnormalities
|
-More commonly seen with subchronic or chronic Pb exposures vs. acute intoxications
-Anemia ranges from microcytic hypochromic to normocytic normochromic -Anemia may initially be regenerative -Can progress to non-regenerative in severe chronic cases |
|
|
|
Pb basophilic stippling
|
-Basophilic stippling is normal in ruminants!
-More diagnostic in dogs and horses |
|
|
|
Pb and Nucleated RBCs
|
-large numbers of nucleated RBCs can be indicative of Pb toxicity
-Even without severe anemia -Small animals |
|
|
|
Pb Whole Blood
|
-Whole blood Pb levels do not necessarily reflect total body burden of Pb
-Do not correlate with severity of clinical signs -IN most species blood levels greater than 0.3-0.35 ppm indicate significant Pb exposure -Greater than 0.6 ppm is diagnostic for Pb toxicosis |
|
|
|
Pb Toxicity Treatment
|
-Stabilization of the animal is important!
-Elimination of Pb from GI tract -Chelation --succimer of CaEDTA and BAL or thiamine --chelators are not that specific -General supportive care -Elimination of Pb from the animal's environment |
|
|
|
Mercury
|
-Common source of exposure in dogs
-Inorganic elemental mercury in glass thermometers --poorly absorbed from GI tract, not considered health hazard when ingested -Issue comes with aerosolization --do not vacuum! -Acute and chronic mercury poisoning of animals is rare |
|
|
|
Toxic sources of Mercury
|
-Inorganic mercuric salts (divalent): preservatives and fixatives
-Inorganic mercurous salts (monovalent): preservatives and fixatives -Organic alkyl mercurials: fungicides --methyl mercury --ethyl mercury -Aryl mercurials (Phenyl mercuric acetate): in paints |
|
|
|
Mercury toxicosis
|
-Organic forms are very lipophilic
--methyl mercury, ethyl mercury --lipophilic --readily absorbed by the GI tract and accumulate in the brain -Inorganic mercurial salts are transported in RBCs and plasma --accumulate in renal cortex, localize in lysosomes -Alkyl organic mercury compounds accumulate in the brain |
|
|
|
Mercury and the Placenta
|
-All forms of mercury can cross the placenta
-Accumulate in the fetus -Organomercurials severely damage granular cells in cerebellum --cause cerebellar hypoplasia in neonates born to mothers with mercury exposure |
|
|
|
Mercury excretion
|
1. Inorganic mercury: excreted in urine
--causes direct tissue necrosis and renal tubular necrosis 2. Organic mercurials are excreted mainly in bile and feces |
|
|
|
Mercury Bioaccumulation
|
-Bioaccumulation occurs as move up the food chain
-Marine mammals have some ability to detoxify |
|
|
|
Elemental Mercury Toxicity clinical signs
|
-Renal damage
-Stomatitis -Pharyngitis -vomiting -Diarrhea -Dehydration -Shock -Death may occur within hours of ingestion -In animals that survive acute toxicosis, oliguria and azotemia can come after |
|
|
|
Alkyl mercury toxicosis clinical signs
|
-Can develop slowly over 7-21 days
-Early signs: erythema of skin, conjunctivitis, lacrimation, stomatitis -Intermediate signs: depression, ataxia, incoordination, paresis, blindness -Dermatitis, pustules, epithelial ulcers -Anemia due to hematuria and melena -Advanced signs: proprioceptive defects, abnormal postures, complete blindness, anorexia, paralysis, slowed respiration, death |
|
|
|
Post-mortem Lesions from Mercury toxicity
|
1. GI lesions: gastric ulcers, necrotic enteritis
2. Renal lesions: pale swollen kidneys with tubular necrosis 3. Cattle: Degeneration of purkinje network in heart 4. Swine: extensive degeneration and demyelination of peripheral nerves |
|
|
|
Mercury Toxicity treatment
|
-Penicillamine after intestine is cleared
-Succimer DMSA to reduce urinary excretion of inorganic mercurials --decreased renal damage -Nutritional selenium and vitamin E are somewhat protective |
|
|
|
Selenium
|
-Essential dietary constituent
-Can also be toxic if ingested in large amounts --livestock intoxication from excess supplemental selenium in ration -Can also have parenteral overdose (injected too much) -Can also ingest plants that contain excess selenium |
|
|
|
Selenium Toxicity in Livestock
|
1. From plants
2. From excess selenium in ration 3. Parenteral excess, given when animal is sick |
|
|
|
Selenium in Wildlife
|
-Wild aquatic birds
-From agricultural drainage water |
|
|
|
Selenium Absorption
|
-Duodenum is primary site of absorption
-Little or no selenium in rumen or abomasum -40% of oral dose is absorbed by cattle -Eliminated in urine, feces, and air --most comes out in urine |
|
|
|
Porcine Focal Syndrome polioencephalomyelitis
|
-Results from induced deficiency of nicotinamide OR selenium intoxication
-Causes cervical and lumbosacral intumescences |
|
|
|
Acute Selenium Intoxication
|
-Does not happen very often
-Will smell garlicky odor on breath (selenium excretion via air) --caused by methylated metabolite |
|
|
|
Selenium intoxication in Pigs Clinical Signs
|
-Hind-limb ataxia
-posterior paralysis -tetraparesis or paralysis -Affected pigs remain alert and attempt to alk, drag hind limbs -Can have hoof separation at coronary band |
|
|
|
Chronic Selenium intoxication
|
-"Alkali disease"
-Chronic consumption of grasses and crops high in selenium -Occurs in cattle, horses, sheep, pigs, poultry -Causes lameness, hoof over-growth, hoof deformation -Hair loss and discoloration |
|
|
|
Selenium "Blind Staggers"
|
-Form of chronic selemium toxicity
-Occurs when cattle graze certain plants with high concentration o water-soluble selenium containing compounds -Cannot be replicated experimentally! -Mostly affects cattle -Most likely a syndrome with multiple etiologies |
|
|
|
Selenium lesions
|
-heart is major target organ
-Cardiac failure -Loss of microvascular integrity |
|
|
|
Selenium diagnosis
|
-based on clinical signs
-Lesions -Chemical analysis of tissues and body fluids |
|
|
|
Selenium Differential Diagnoses
|
-Organic arsenic toxicosis
-Water deprivation -Pseudorabies in pigs -Ca/P imbalances -Anything having to do with feet |
|
|
|
Copper and Molybdenum
|
-Consider Copper and molybdenum together
-If there is dietary molybdenum deficiency, will have excessive absorption and storage of copper -Sheep are very sensitive --if given calf or horse rations, will get excess of copper |
|
|
|
Monensin and Copper
|
-Can cause excessive copper absorption from intestine
|
|
|
|
Copper in Footbaths
|
-Can act as a source of copper toxicosis
|
|
|
|
Copper Absorption
|
-Monogastrics: stomach, duodenum, jejunum, ileum
-Ruminants: in lower small intestine -Transported through enterocytes, then loosely binds to albumin, ceruloplasmin, and transcuperin -Distributed to liver, kidney, brain for storage |
|
|
|
Excess Liver Copper
|
-Causes liver necrosis, hepatocytes release Cu
-Releases copper into bloodstream, causes RBC lysis -Hemoglobinuria -Transiently will see elevated Cu in serum -Excess free copper accumulates in the kidney -most is excreted in bile -Classic syndrome in sheep -Swine, horses, chickens, turkeys are resistant to copper toxicity |
|
|
|
Copper and Kidneys
|
-Excess free copper accumulates in the kidneys
-Primary post-mortem specimen/organ of choice |
|
|
|
Copper and Sheep
|
-Sheep are very sensitive to Cu
--30ppm is toxic (cattle can handle up to 50ppm) -Usually do not show clinical signs until they are really stressed -Excess Cu accumulates over time, stressful event allows excess release from liver -Intravascular hemolysis: hemoglobinurua, icterus, anemia, death |
|
|
|
Dogs and Copper Toxicity
|
-In general dogs are resistant to copper toxicity
-Bedlington, WHWT, and Skye terriers have hereditary autosomal recessive disorder --decreased biliary excretion --results in accumulation of Cu in liver -Develops gradually, animal develops gradual hepatitis -Eventually get hepatocellular degeneration |
|
|
|
Clinical signs of dog with Cu toxicity
|
-Weight loss
-Anorexia -Ascites -CNS signs -Liver enzymes are often elevated -Icterus is uncommon |
|
|
|
Treatment of Cu toxicity in Sheep
|
-Treatment is usually not successful
|
|
|
|
Treatment of Cu toxicity in Dogs
|
-D-penicillamine
-Chelated copper, promotes urinary excretion in dogs with copper hepatopathy |
|
|
|
Molybdenum Sources
|
-Soil
-Ground water -Fossil fuels -Deposition on forage from molybdenum emissions from smelting, factories, etc. -Petroleum transmission pipelines |
|
|
|
Molybdenum
|
-Required in diet for metalloenzymes
--xanthine oxidase, xanthine dehydrogenase, aldehyde oxidase, sulfite oxidase -3-way interaction with Cu and Sulfur |
|
|
|
Molybdenum and Ruminants
|
-Ruminants are more sensitive to toxicity
-Attributed to sulfur metabolism in the rumen -Cattle are most sensitive --cattle on high-sulfur diet may be at more risk -Mule deer are most resistant |
|
|
|
Cu, S, Mo
|
-Cattle on high-sulfur diet will have decreased Cu absorption
-Decreased Cu, increased susceptibilty to Molybdenum -Diets high in Molybdenum can decrease absorption of Zn |
|
|
|
Molybdenum toxicity Clinical Signs
|
-Cattle: chronic diarrhea
-Relative copper deficiency causes abnormalities in connective tissue and bone -Pregnant mares will abort -No characteristic gross or histopathologic lesions for molybdenum-induced copper toxicity -Emaciation is most observed clinical sign |
|
|
|
Molybdenum Toxicity diagnosis
|
-Based on clinical signs
-Concentrations of molybdenum in the blood, liver, and kidney -Most common finding is high molybdenum with low copper concentrations in the liver |
|
|
|
Fluoride Toxicity
|
-Usually comes phosphate supplements that are not defluorinated completely
-Forages contaminated with industrial pollutants, dusts, or volcanic ash |
|
|
|
Fluoride ADME
|
-Absorbed from GI tract
-Transported in plasma -Accumulate in bone -Kidneys contain the greatest F concentration of soft tissues -Half of absorbed F is excreted in the urine |
|
|
|
Fluoride chronic exposure
|
-Effect on teeth and skeletal system
-F replaces hydroxyapatite --causes delayed and altered mineralization of bone -Structural changes in teeth occur prior to eruption --after eruption, teeth wear down easier, are prone to breaking -Damage occurs, organic material accumulates in weakened/damaged part of the teeth --causes black/brown discoloration |
|
|
|
Fluoride in Bone
|
-Causes dysfunction of normal osteogenesis
-Changes bone remodeling -Abnormal bone can be produced -Accelerated absorption of bone -Abnormal and excessive bone remodeling leads to subperiosteal hyperkeratosis with thickened and irregular long bone surfaces |
|
|
|
Fluoride in younger animals
|
-Younger animals are more at risk
-Actively forming bone and teeth, more susceptible |
|
|
|
Fluoride in Swine and Poultry
|
-Ca-deficient diet increases accumulation of F
-Can lead to toxic effects of F -Increased dietary fat can enhance effects of F in poultry |
|
|
|
Acute Fluoride Toxicosis
|
-Caused by compound 10-80
-Not used anymore, but still exists out there -Results in excitation, seizures, urinary and fecal incontinence, vomiting, weakness, hypersalivation, depression -Eventually causes cardiac depression and death |
|
|
|
Chronic Flurosis
|
-Dental and skeletal effects
-Dry haircoat and skin -Weight loss -decreased milk production |
|
|
|
Treatment of Fluoride overload
|
-Aluminum sulfate
-Aluminum chloride -Calcium aluminate -Calcium carbonate -Reduce absorption of F in diet |
|
|
|
Iron
|
-Essential metal
-Most abundant trace mineral in the body -Sources for animals: iron supplements, multivitamins, dietary supplements, foods, fertilizers, soil -Come in injectible and oral forms |
|
|
|
Iron Toxicosis
|
-Usually due to excessive injections in neonatal pigs
-Ingestion of large amounts of Fe-containing compounds in other species -Most toxic when given IV |
|
|
|
Iron Absorption
|
-2-step process
-Occurs in duodenum and upper jejunum -Needs to be in ionized form for absorption 1. Ferrous ions are absorbed from intestinal lumen into mucosal cells -transferrin-like protein facilitates entry into mucosal cells (rate-limiting factor), depends on healthy mucosal cells -Energy-dependent carrier 2. Transfer of Fe to ferritin or into circulation bound to transferrin proteins -complexed with transferrin and distributed to other storage locations |
|
|
|
Iron in the Body
|
-70% is found in Hb
--in FERROUS form bound to normal Hb and myoglobin --in FERRIC form when stored in hemosiderin, ferritin, and transferrin -Most Fe i stored in the liver, spleen, bone marrow |
|
|
|
Acute Fe Toxicosis
|
-Direct corrosive effect on the GI tract
-Causes cellular damage due to un-bound iron in circulation -Free Fe causes increased lipid peroxidation --leads to membrane damage to mitochonidria, microsomes, and other cellular organelles -Most effects on cardiovascular system |
|
|
|
Fe Toxicosis effect on organs
|
-Mostly affects the cardiovascular system
-Fatty necrosis of the myocardium -Post-arteriolar dilation -Increased capillary permeability -Reduced CO -Also interferes with normal clotting mechanisms -Can cause metabolic acidosis |
|
|
|
Excretion of Iron
|
-No mechanism for excretion of Fe in the body!
-Toxicity depends on the amount of Fe already present in the body -Amount of elemental Fe allows assessment of toxicity |
|
|
|
Iron Toxicity Levels
|
-Less than 20 mg/kg of elemental iron is NON-toxic to dogs
-Ingestion of 20-60 mg/kg of elemental Fe can cause mild clinical signs -more than 60 mg/kg of elemental iron can cause serious signs when ingested -ore than 100-200 mg/kg of elemental iron is LETHAL |
|
|
|
Iron Storage Diseases
|
-Hemochromatosis
-Hemosiderosis |
|
|
|
Hemochromatosis
|
-Pathologic tissue accumulation of Iron
|
|
|
|
Hemosiderosis
|
-Non-pathologic accumulation of Iron
|
|
|
|
Clinical phases of Iron Toxicosis
|
1. 0-6 hours post-exposure
-vomiting, diarrhea, GI bleeding -Most with mild to moderate iron toxicosis do not progress past stage 1 2. 6-24 hours post-exposure -transient latent period 3. 12-96 hours after clinical signs -lethargy, GI signs, metabolic acidosis, shock, hypotension, tachycardia, cardiovascular collapse, coagulation deficits, hepatic necrosis -Death! 4. 2-6 weeks -GI ulcerations develop -Fibrosis from healing can cause scarring and strictures |
|
|
|
Pigs given Iron Injections
|
1. Peracute syndrome: sudden death
-shot probably went into a vein 2. Too much given: lethargy, coma, death |
|
|
|
Iron Toxicity Diagnosis
|
-Serum iron levels are best method to confirm poisoning
-Measuring total iron-binding capacity is helpful (TIBC) --"carrying capacity" of the body for iron -When serum iron is greater than TIBC, will have severe systemic effects |
|
|
|
Treatment of Iron Toxicity
|
-Recent ingestion: gastric decontamination
-Activated charcoal does not effectively bind Fe -Can give sodium phosphate, sodium bicarbonate, magnesium hydroxide -Restore fluid and electrolyte imbalances -Give GI protectant (sucralfate, cimetidine, misoprosterol) -Chelation therapy for animals showing signs of severe toxicosis --Deferoxamine has highest affinity for Fe within the body --continue until serum iron levels are below 300 ug/dL or below TIBC --2-3 days of therapy may be needed |
|
|
|
Sodium Toxicosis
|
-Salt poisoning
-Direct toxicosis: ingesting too much sodium --in feed, water --illness develops in 24-48 hours -Indirect toxicosis: water deprivation --Develops over 4-7 days --most common type of sodium ion toxicosis in domestic livestock |
|
|
|
Hypernatremia
|
-Occurs when Na content of extracellular fluid increases in relation to free water content
-Free water is lost from extracellular fluid without compensatory decrease in Na -Serum Na levels increase above normal (133-155 mEq/L) --Na passively diffuses into CSF --CSF Na is increased above normal (135-150) |
|
|
|
Excess salt intake
|
-Leads to severe gastroenteritis
-Electrolyte imbalances -Severe dehydration -Acute death |
|
|
|
Acute Hypernatremia
|
-Neurons in the brain are trying to equalize osmotic pressure and prevent intracellular fluid loss
-If insult is quickly resolved without damage to neurons, levels decline and go back to normal -If defense mechanism fails and brain cannot kick Na back out, brain cells shrink and tear --cerebral edema develops --Leads to hemorrhage, brain infarcts, cerebral edema |
|
|
|
Na transport into the brain
|
-Passively enters CNS
-Actively transported back out into serum -Energy deficit develops -Na is trapped in the brain and CSF -If water is given, osmotic gradient is established, results in influx of fluid into CSF --results in cerebral edema |
|
|
|
Chronic hypernatremia
|
-Organic solutes (Idaiogenic osmoles) increase to maximum levels over time
--48-72 hours |
|
|
|
Na toxicity in Swine
|
-Early clinical signs of Na ion toxicosis are generally unnoticed
-Restlessess, thirst, pruritus, constipation, vomiting -Progress to aimless wandering, blindness, head pressing, circling -Muscle twitches -Pig assumes dog-sitting position -Seizures and death |
|
|
|
Na toxicity Diagnosis
|
-Measure levels of Na in CSF and serum
-Brain Na levels of 1600 and 1800 ppm are upper normal limits for cattle and swine -Can look at ocular fluid --Na stays stable in ocular fluid |
|
|
|
Na Toxicity Treatment
|
-Water deficit needs to be replaced slowly
--prevents iatrogenic cerebral edema -Correct over 48-72 hour period -If cannot be monitored, water intake should be limited to 0.5% of body weight at 60-minute intervals until rehydrated -Can give hypertonic saline solutions or isotonic saline solutions to reduce iatrogenic cerebral edema -Can give mannitol or glycerin for cerebral edema to try to pull H2O out of brain -Guarded prognosis, at least 50% will die |
|
|
|
Zinc Sources
|
-Usually stuff in the environment
-Zinc on animal carriers -Things used to attach containers -Galvinized pipes or equipment -Caging-type material -U.S. pennies minted after 1982 -Topical zinc ointments |
|
|
|
Zinc Absorption
|
-Absorption in proximal small intestine
-Occurs in 2 steps -Influenced by dietary factors, age, growth rate -Copper interferes with Zn absorption, Zn interferes with Cu absorption --compete for same protein-binding sites in the duodenum? |
|
|
|
Zinc Excretion
|
-Excreted in the feces by bile, intestinal mucosal secretions, and pancreatic fluid
-Chelated Zn is excreted via bile and urine |
|
|
|
Zinc toxicity Clinical Signs
|
-GI signs
-Vomiting, diarrhea, inappetance -Depressed -Icteric/pale -Tachycardia -Hemoglobinemia, hemoglobinuria -Take radiograph!! |
|
|
|
Zinc Toxicosis
|
-Severe intravascular hemolysis is most common
|
|
|
|
Zinc Toxicosis Diagnosis
|
-Special royal blue-top tubes with plastic stoppers
--Rubber in blood tubes or syringe stoppers can falsely elevate Zn levels |
|
|
|
Zinc Toxicity Treatment
|
-Symptomatic and supportive care
-remove zinc foreign bodies ASAP |
|
|
|
Fish Gallbladders
|
-Ctenopharynogodon idellus: raw grass carp gallbladder
-Causes acute renal and hepatic failure -Acute tubular necrosis and focal hepatitis -Hepatotoxicity usually comes first |
|
|
|
Icthyosarcotoxism
|
-Toxicity from fish
|
|
|
|
Ciguatera poisoning
|
-Most common forms of icthypsarcotoxism
-Accumulates toxic dinoflagellate, toxins accumulate up the food chain -Outbreaks occur in emperor fish, grouper, parrotfish, red snapper, and surgeonfish |
|
|
|
Types of Ciguatera toxins
|
1. Ciguatoxin: primary toxin involved
--antagonized with physostigmine 2. Maitotoxin: only in intestines --reversed with verapamil 3. Scaritoxin 4. Brevetoxins a and b 5. 35s-methylokadiac acid |
|
|
|
Signs of Ciguatera toxicity
|
-Numbness of mouth and limbs
-Vomiting and diarrhea -Hot and cold flushes -aching joints and muscles -Associated with consumption of tropical reef fish -Low fataility rate, but feel pretty terrible |
|
|
|
Sources of Tetrodotoxin Poisoning
|
-Puffer or fugu poisoning (most known)
-Pacific goby -Ocean sunfish -Porcupine fish -Central americam frogs -California newt -Blue-ringed octopus -Starfish -Molluscs -Crabs |
|
|
|
Tetrodotoxin
|
-Concentrated in gonads and liver
-Not heat-labile -Blocks Na channels on nerve and muscle membranes --no nerve conduction --decreased muscle responsiveness |
|
|
|
Scombroid Poisoning
|
-Histamine formed from improper storage of fish
--histidine is converted to histamine and saurine inside the fish -Saurine: phosphate salt of histamine -Urocanic acid is also present --mast cell degranulator -Causes mast-cell reaction, histamine reaction |
|
|
|
Signs of Scombroid Poisoning
|
-Intense histamine reaction
-Sweating, headaches, diarrhea, nausea -Tingling/burning sensation in mouth -Facial swelling, rash, hives, itchy skin -Signs can persist for up to 12 hours but no long-term consequences expected |
|
|
|
Stingrays
|
-Verminous fish
-Caudal spines on dorsum of tail can cause penetrating sounds -Also have venom in secretory grooves of caudal spine --Causes vasodilation, vasoconstriction, bradycardia |
|
|
|
Scorpion Fish
|
-Verminous fish
-Venom apparatus of dorsal, anal, and pelvic spines -Integument also has venom |
|
|
|
Catfish
|
-Verminous fish
-Dorsal and pectoral fin spines contain glandular tissue -Proteinaceous venom, causes local pain and edema -Crinotoxins in epidermal secretions coating entire body surface -Can cause septic arthritis via Edwardsiella tarda secondary infection from penetrating wound |
|
|
|
Paralytic Shellfish Poisoning Sources
|
-Alaskan butter clam
-Soft-shelled clams -Mussels -Sea scallops -Oysters |
|
|
|
Paralytic Shellfish Poisoning
|
-Caused by accumulation of toxic dinoflagellates
-Saxitoxin, neosaxitoxin, Brevetoxins a and b, Okadiac acid-like toxin -Domoic Acid toxin causes amnesic shellfish toxicosis |
|
|
|
Syndromes associated with Shellfish Poisoning
|
-Paralytic shellfish poisoning
-Neurotoxic Shellfish poisoning -Diarrhetic shellfish poisoning -Amnesic shellfish poisoning |
|
|
|
Hymenoptera
|
-Ants
-Bees -Wasps -Hornets |
|
|
|
Ant toxins
|
-Formic acid toxin sprayed into bite wounds from abdominal glands
-Proteinaceous venoms, peptides and enzymes --paralytic to invertebrates, neurotoxic to vertebrates -Hemolysin -Histamine, serotonin, dopamine, acetylcholine, NorEpi -Alkaloids (fire ants) |
|
|
|
Bee Wasp Hornet Toxins
|
-Allergens incite allergic response and cause local tissue damage
-Allergens: Phospholipase A2, hyaluronidase -Non-allergens: histamine, dopamine, NorEpi, amino acids |
|
|
|
Blister Beetles
|
-Beetles that feed on alfalfa flowers, specific to ALFALFA
-Crushed into hay during cutting and baling -Horses are susceptible -Cantharidin toxin is in beetles, then gets into hay --male beetles have highest concentrations -Potent vesicant -Readily absorbed through GI tract -Excreted from kidneys -Can be detected in urine, kidney, blood, GI contents |
|
|
|
Blister Beetle Toxicity signs
|
-Peracute death from shock if consumed in high doses
-Colic, anorexia, alimentary tract ulceration -Hyperthermia, weakness, depression, dehydration, dysuria, hemoconcentration, diarrhea, death -Diagnosis is based on clinical signs, lesions, and identification of beetles in hay |
|
|
|
Blister Beetle Toxicity Lesions on Necropsy
|
-Areas of ulceration or erosion in terminal portions of esophagus, stomach, intestines
-Lesions can sometimes be reddening of mucosa of GI tract and urinary bladder -Streaks of ventricular myocardial necrosis in the heart |
|
|
|
Blister Beetle Treatment
|
-Enhance fecal and urinary elimination of toxin
-Correct dehydration -Manage serum Ca and Mg abnormalities -Pain control -Repeated dose of mineral oil and activated charcoal may be beneficial for binding toxin --helps toxin move faster through GI tract |
|
|
|
Fireflies
|
-Toxicosis reported when owners feed fireflies to pet reptiles/amphibians
-Lucibufagins are toxic chemical --steroid pyrones --Structurally similar to bufodienolides and cardenolides -Toxicity has been known for a long time -Presents as head-shaking, oral gaping, color changes, death -Basically cardiovascular signs |
|
|
|
Monarch Butterflies
|
-Toxins are accumulated from milk weeds
--larvae feed on Asclepias/Milkweed -Cardiac glycosides are stored in the wings of the adults -Cause immediate vomiting in birds |
|
|
|
Sawfly larvae
|
-Larvae accumulate under silver-leaf ironbark eucalyptus
-Associated with larvae -Lophyratomin toxin -Causes hepatic necrosis and renal damage when ingested by sheep or cattle --usually accidental ingestion |
|
|
|
Caterpillars
|
-Hairs cause stinging and skin irritation
-Puss moth caterpillar -Io Moth caterpillar -Saddleback caterpillar |
|
|
|
Tent Caterpillar
|
-Causes Equine fetal losses
-Fibrinous pericarditis -Unilateral uveitis -Associated with exposure to eastern tent caterpillar -Something in the skin causes abortions -Abortions are NOT seen with laboratory-raised caterpillars, not associated with caterpillar-carried viruses or bacteria |
|
|
|
Other factors contributing to Equine Fetal Losses
|
-Cherry trees preent
-more than 50 broodmares on the farm -excess white clover in pasture -Abortion during previous pregnancy |
|
|
|
Asian Lady Bugs
|
-Harmonia axyridis
-Cause severe mucosal hemorrhage and congestion -Dogs present with severe shock and die |
|
|
|
Lactrodecus mactans
|
-Black Widow Spiders
-Identified by hourglass on ventral abdomen -Only females envenomate --male jaws are too small, unable to penetrate skin -15% of bites may be "dry," not dangerous -Alpha-latrotoxin is main toxin --large, labile protein neurotoxin --Causes Ca-independent NT release -Causes muscle fasciculations or rigidity, abdominal pain, ataxia, flaccid paralysis -Can progress to ascending paralysis -Cats vomit, hypersalivate, and have diarrhea -If respiratory muscles are compromised, can have altered breathing and death |
|
|
|
Lactrodecus mactans Treatment
|
-Symptomatic/supportive care
--respiratory and cardiovascular monitoring and pain management -Ca gluconate can reverse signs of muscle fasciculations and weakness -Anti-venin can be used as antidote -Most animals recover completely within a few days with symptomatic and supportive care |
|
|
|
Loxosceles
|
-Brown Recluse Spiders
-Characteristic dark marking on dorsal aspect of the cephalpthorax and long thin brown legs -Venom is a complex mixture of enzymes -Associated with dermal necrosis -Sphingomyelinase is primary components -Fangs of spider can also introduce clostridial organisms into the wound --secondary bacterial infections are possible |
|
|
|
Sphingomyelinase
|
-Primary component of Loxosceles spider venom
-Interacts with plasma membranes of endothelial cells, RBCs, and platelets -Causes microvascular disruption, platelet aggregation -Intravascular coagulation in capillaries and dermal necrosis |
|
|
|
Theraphosidae
|
-Tarantula spider
-Most US species are not highly venomous -Cause pain at the site of the bite -Hairs can cause urticaria |
|
|
|
Tick Paralysis
|
-Holocyclotoxin in Ixodes ticks: neurotoxin
-Signs generally occur after ticks have been feeding for 5 days or more -Causes ascending paralysis -Death is due to respiratory paralysis -Removing ticks will cause spontaneous recovery and do not seem to have any long-lasting issues |
|
|
|
Frog Toxins
|
-Mucus glands distributed over entire body
-Glandular glands distributed on sides of the head, shoulders, and dorsolateral margins -Venom precursors come from ingested ants, beetles, and millipedes -Causes flaccid paralysis, cardiac arrhythmias, cardiac arrest |
|
|
|
Bufo marinus
|
-Cane toad, marine toad, giant toad
-Lots of different secertions with lots of stuff in secretions -Toxicosis is mostly due to interactions between different secretion components |
|
|
|
Toad Toxins
|
-Bufagins: sterol aglycones with digitalis-like effects
-Bufotoxins: Similar mechanism of bufogenin -Bufotenines: tryptamine bases -Affect cardiovascular system |
|
|
|
Signs of Bufo toad toxicity
|
-Salivation
-Cardiac arrhythmias -Hypotension -Hyperkalemia -Weakness -Ataxia -Collapse -Seizures -Coma |
|
|
|
Treatment for Bufo toad toxicity
|
-ECG monitoring when arrhythmias are present
-Atropine for bradycardia -Propranolol/ beta-antagonist for sustained tachycardia -Digoxin-specific Fab fragment experimental use -Wash out mouth! a lot of toxin can be absorbed across mucosal membrane in mouth |
|
|
|
Crotalidae
|
-Pit vipers
--copperheads, cotton-mouths --rattlensakes, massausaugas -Arrow-shaped head -Retractable, hinged fangs -Venom gland is a modified parotid gland - |
|
|
|
Elapidae
|
-Cobras, kraits, mambas, coral snakes
-Short, grooved fangs that are not hinged -Small round head and small round eyes |
|
|
|
Coral Snakes
|
-Elapidae family
-Sonoran coral snake: rarely medically significant, venom has low potency -Micrurus fluvius are more of a concern |
|
|
|
Phospholipase A2
|
-Most important enzyme in snake venoms
-Hemolytic activity -Cardiotoxic activity -Anticoagulant -Neurotoxic |
|
|
|
Hyaluronidase
|
-Enzyme present in snake venom
-breaks down connective tissue locally -Makes it easier for other enzymes to spread into the surrounding tissues |
|
|
|
Enzymes present in snake venom
|
-Phospholipase A2
-Hyaluronidase -Proteases -Collagenase -Thrombin-like enzymes -Phosphodiesterases |
|
|
|
Other components of Snake Venom
|
-Non-enzymatic polypeptides
-Mojave toxin -Metal ions |
|
|
|
Crotalid bites
|
-Pit viper pites
-Pain, swelling, erythema at bite site -Progressive edema, local hemorrhage, tissue necrosis -Severe bite can result in systemic manifestations --Hypovolemic shock -Neurotoxin in mojave rattlesnakes can cause flaccid paralysis and respiratory paralysis |
|
|
|
Dry bite
|
-Bite in which no venom is injected
-25% of snake bites are dry bites -Bites are more common in hotter summer months --snakes are more active --venom yields are increased --more people are out and about with pets |
|
|
|
Monitoring with Pit viper bite
|
-Activated partial thromboplastin tie
-Prothrombin time -Fibrinogen -Fibrin split products -Platelet counts -Look at blood -Urinalysis for hematuria or rhabdomyolysis |
|
|
|
Sequelae of Crotalid pit viper bites
|
-Tissue sloughing around bite site
-Primary cause of death is cardiovascular collapse --results from hypovolemic shock |
|
|
|
Treatment for Crotalid Pit viper bite
|
-Seek medical attention ASAP
-increased mortality with corticosteroid use |
|
|
|
Elapid bites
|
-signs may be delayed
-Pain and swelling at the bite site is often minor -Neurologic signs mostly, especially with cats --weakness and paralysis -Marked hemolysis in dogs -Progressive paralysis and respiratory failure --may require rapid intbation and mechanical ventilation |
|
|
|
Antivenins
|
-Polyvlent crotalid anti-venin is available
-CroFabTM for sheep -Micrurus fulvus against eastern coral snake venom |
|
|
|
Factors contributing to plant poisonings
|
-Concentrations of toxins vary
-Time of year -Environmental factors --rainfall -Animal species vary in sensitivity to poisonous plants |
|
|
|
Cicuta
|

|
-Cicutoxin in roots and base of stem
-GABA antagonist, inhibits Cl influx into neurons -Signs: seizures, salivation, muscle twitching, coma, death -Multifocal myocardial degeneration and skeletal muscle degeneration -ACUTE DEATH -LDH, AST, and CK may be elevated -No specific antidote --can treat seizures --GI decontamination -Prevent by digging up plants and burning or using herbicides |
|
|
Conium
|

|
-Purple spotted roots
-Piperidine alkaloid toxin -Blocks spinal cord reflexes -ANS ganglia are stimulated, then depressed -Neuromuscular blockade and paralysis -Salivation, abdominal pain, muscle tremors, dyspnea, dilated pupils, weak pulse, urination, defectaion, temporary blindness -ACUTE DEATH -Dx: cyanosis, respiratory paralysis, coma -Animals that survive may abort if pregnant -No specific treatment, supportive care -Saline cathartics, activated charcoal -Remove plants via mowing or with herbicides |
|
|
Delphinium
|

|
-Diterpenoid alkaloid toxin
-Reversibly binds and competitively blocks nicotinic ACh receptors at NMJ -Causes muscle weakness, paralysis, bloat, inhalation of rumen contents -ACUTE DEATH -Non-specific post-mortem findings, my find plant fragments in feces/rumen -Tx with pheostigmine and neostigmine --Pass stomach tube to relieve gas -ACUTE DEATH |
|
|
Prunus and Sorghum
|

|
-Cyanogenic glycosides
-HCN activates cellular respiration by inactivating cytochrome oxidase enzymes -RBCs are unable to release oxygen to the tissues -ACUTE DEATH -Rapid labored breathing, frothing, dilated pupils, ataxia, muscle tremors, mucus membranes start bright red, then change to cyanotic -Cherry red venous blood -Generalized congestion and cyanosis of internal organs -Dx: liver, blood, rumen contents -Tx: Sodium nitrite: converts Hb to methemoglobin to reactive cytochrome oxidase --Sodium thiosulfate combines with cyanide to form Sodium thiocyanate -Prevent by keeping animals from grazing after cutting, drought, frost |
|
|
Asclepias
|

|
-Cardenolide toxin
-Cardiac Glycoside -Inhibits cell membrane Na/K ATPase pumps and increases serum K -Decreases electrical conductivity through the heart -Results in severe arrhythmias and conduction disturbances leading to death -Animals are often found dead -Tachypnea, rapid weak irregular pulses, cold extremities -Sheep will have labored breathing, staggering, bloat, dilated pupils, terminal convulsions -Will see arrhythmia on ECG -Tx: decontamination, activated charcoal --antiarrhythmic drugs, monitor serum K -Avoid giving patient fluids containing K and Ca |
|
|
Nerium Oleander
|

|
-Oleandrin and neriine toxins
-Cardiac Glycoside -Inhibits cell membrane Na/K ATPase -Increases serum K -Decreases electrical conductivity through the heart -Results in severe arrhythmias and conduction disturbances leading to death -Animals are often found dead -Tachypnea, rapid and weak irregular pulses, cold extremities -ECG will have arrhythmia -Tx: decontamination with activated charcoal --anti-arrhythmic drugs, monitor serum K -Avoid fluids with K and Ca |
|
|
Taxus
|

|
-Taxine toxin
-Cardiotoxic -INhibits normal Na/Ca exchange across myocardial cells -Depresses myocardial depolarization and results in arrhythmias -Sudden muscle tremors, incoordination, nervousness, dyspnea, bradycardia, vomiting, diarrhea, convulsions, death -No diagnostic lesions -Can diagnose by microscopic examination of stomach/rumen contents -No specific Tx or antidote -Activated charcoal, rumenotomy -Atropine sulfate and fluids for supportive care -Don't plant Taxus around animal enclosures, and never feed prunings! |
|
|
Senecio
|
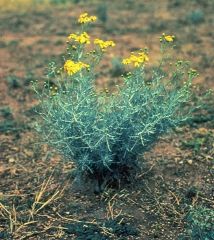
|
-Pyrrolizidine alkaloid poison
-Hepatotoxic plant -Causes weight loss, neurologic signs, photosensitivity -Skin sloughs off in 2-3 weeks, can result in secondary bacterial infections -Signs of liver failure, pathologic changes of hepatocellular necrosis -Dx via elevated liver enzymes and other liver function tests -Need to do liver biopsy to confirm necrosis -Tx: shelter animal from sun, prevent further access to plant material -Give balanced high energy low protein diet to prevent liver overload -Selectively remove senecio |
|
|
Astragalus and Oxytropis
|

|
-Swainsonine toxin
-Neurotoxic plant -INhibits lysosomal enzymes that are important for saccharide metabolism --Causes oligosaccharides to accumulate in the brain and other organs -Most often in horses -Depression, circling, incoordination, staggering gait, unpredictable behavior -Animal can become aggressive and difficult to handle -Weight loss, poor growth -Can get better if animal is removed from the source but affected neurons may never fully regenerate -Can induce infertility and reproductive failure -Diagnose by presence of swainsonine in serum coupled with decreased serum alpha-mannosidease activity -Will have elevated ALP, AST, LDH -Decreased serum protein and thyroid level -Tx: animal will recover once removed from source if removed before extensive degeneration to the brain -Prevent by moving animal to safe pasture areas when excessive consumption is observed -Can condition animal to have aversion to eating Astragalus |
|
|
Eupatorium
|

|
-Tremetone toxin
--requires microsomal activation to become toxic -Neurotoxic plant -Causes severe skeletal and myocardial degeneration -Tremetone can accumulate and be secreted in milk -Animal will be listless, depressed, lethargic, and reluctant to move -Signs of colic, constipation -Tremoring animals can become recumbent or choke from pharyngeal paralysis -Will see fatty degeneration of liver and kidney on necropsy -No specific diagnostic tests -ECG may show complete AV block, VPCs, marked ST depression -Associated with myocardial ischemia -No specific antidote -Stop consumption of plant or milk with toxin -Supportive care |
|
|
Acer rubrum
|

|
-Unidentified toxin
-Affects blood and bone marrow -Oxidant damage to Hb results in heinz body formation -RBC damage leads to hemolytic anemia -Only equids are affected -Acute hemolytic anemia: weakness, tachypnea, tachycardia, cyanosis, icterus, brown urine -Pale organs, hemorrhages on serosal surfaces, splenomegaly -Liver lipidosis and necrosis -Dx: decreased HCT, methemoglobinemia, heinz bodies, depletion of erythrocyte glutathione -Elevated AST, SDH, protein, and bilirubin -Tx: blood transfusions if necessary --Fluids to prevent dehydration and to preserve renal function -Prognosis is guarded to poor due to intravascular hemolysis -Emergency and supportive care for treatment of shock, acidosis, and dehydration |
|
|
Allium
|

|
-N-propyl disulfide
-Affects blood and bone marrow -Oxidizes RBCs to form Heinz bodies, affected RBCs are removed by the spleen and results in anemia -Will have heinz body formation even without clinical signs -Dark red/brown urine (hemoglobinuria), pale MM, fast and weak pulses from anemia -Staggering/collapse -Tx: do not stress animal --Blood transfusion as needed for severely affected animals |
|
|
Dieffenbachia
|

|
-Insoluble Ca oxalate crystals
-Affect GI tract -Needle-like Ca oxalate crystals penetrate surrounding tissues when plant material is broken -Oral pain, swelling of lips and tongue, -Irritation of esophagus and stomach -Inappetance due to oral discomfort -Tx: often none is needed --milk products can ease oral discomfort --soft diet, pain control |
|
|
Philodendron
|

|
-Insoluble Ca oxalate crystals
-Affects GI system -Needle-like Ca oxalate crystals penetrate surrounding tissues when plant cells are crushed/broken -Oral pain, swelling of lips and tongue -Irritation of esophagus and stomach -Inappetance due to oral discomfort -Tx: often none is needed --milk can ease oral discomfort --soft diet and pain control |
|
|
Robinia
|

|
-Lectin toxin
-Affects GI system -Inhibits cellular protein synthesis in ribosomes via binding to certain cell receptor sites -Animal will stop eating or lactating -Severe hemorrhagic diarrhea leading to dehydration and hypovolemic shock -Dilated pupils, arrhythmias, severe pulmonary congestion, ulceration of stomach and intestines -Fatty degeneration/necrosis of liver and kidneys -Dx: increased liver enzymes, BUN/creatinine, Na, and K --Decrease in serum protein reflects fluid and electrolyte loss and lectin effect on organ function -Exposure is difficult to confirm unless animals are seen eating plant -Tx: induce vomiting with activated charcoal and cathartic --give fluids and electrolytes |
|
|
Rhododendron/Azalea
|

|
-Grayanotoxin
-Affects GI system -Toxin binds cell membranes and affects Na channels -Causes prolonged depolarization of cells -Primary effects on heart, nervous system, and GI -Anorexia, hypersalivation, vomiting, colic -Weakness, bradycardia, arrhythmias, regurgitation -regurgitation of rumen contents can lead to aspiration pneumnia -Dx based on clinical signs and evidence that plant has been eaten -Tx: decontamination, rumenotomy, atropine for severe cases -Supportive care, oral or IV fluids |
|
|
Kalmia
|

|
-Grayanotoxin
-Causes GI issues -Binds cell membranes and affects N channels --Causes prolonged depolarization of cells -Primary effects on heart, nervous system, GI tract -Anorexia, hypersalivation, vomiting, colic -Weakness, bradycardia, arrhythmia, regurgitation of rumen contents that can lead to aspiration pneumonia -Dx based on clinical signs and evidence that the plant has been eaten -Tx: decontamination, rumenotomy, atropine for severe cases -Remove animal from the source! -Supportive treatment with IV or oral fluids |
|
|
Pieris
|

|
-Grayanotoxin
-Causes GI issues -Toxin binds cell membranes and affects Na channels, causes prolonged depolarization of cells -Primary effects on heart, nervous system, and GI tract -Anorexia, hypersalivation, vomiting, colic -Weakness, braydcardia, arrhythmia, regurtitation that can lead to aspiration pneumonia -Dx based on clinical signs and evidence of munching -Tx: decontamination, rumenotomy, atropine for severe cases -Remove source, remove animal from source -Supportive care, IV or PO fluids |
|
|
Solanum
|

|
-Tropane alkaloid toxin
-Causes GI issues -Acts on ANS, blocks action of cholinesterase, results in accumulation of ACh -Initial CNS excitement followed by depression and decreased heart/respiratory rates -Muscle weakness, dilated pupils, colic, watery diarrhea -Rupture of stomach and paralysis of digestive system can occur in the horse -Most recover with symptomatic care -Animals showing severe signs may be treated with physostigmine |
|
|
Juglans nigra
|
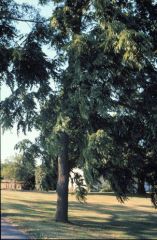
|
-Unknown specific toxin, might be juglone
-Affects musculoskeletal system -Toxin enhances vasoconstriction in presence of catecholamines and corticosteroids -Causes depression, edema of the lower legs, lameness, colic, respiratory distress -Animal may recover if removed from source early -Do not bed stalls with Juglans nigra shavings -Do not plant juglans nigra trees and remove fallen moldy nuts |
|
|
Amaranthus
|

|
-Soluble oxalate crystals
-Affects urinary system -Toxin rapidly combines with serum Ca and Mg, decreases available Ca and Mg -Acute sudden hypocalcemia: impairs normal cell membrane function -Chronic exposure causes oxalate nephrosis from the insoluble Ca oxalate crystals filtered by the kidney -Muscle tremors, tetany, weakness, depression, recumbency -Coma and death -Animals that survive acute toxicity will have severe kidney failure -Kidney may be red and edematous or pale/small -Perirenal edema is a characteristic sign -Rumen epithelium may become hemorrhagic due to large amounts of oxalate -Dx based on plants eaten, clinical signs, and oxalate crystals in urine or in kidney/rumen epithelium -No crystals in urine with acute poisoning -Tx: oral limewater to prevent further absorption of soluble Ca oxalate --IV ca gluconate does not reverse effects -Do not let animal graze where plants predominate |
|
|
Lilium
|

|
-All lilium plants are toxic with unknown toxin
-Causes renal failure via unknown mechanism -Renal tubular necrosis -Vomiting, anorexia, depression within 2 hours -Vomiting may resolve, anorexia and depression continue as BUN, creatinine, K, and P increase -Will see epithelial casts and glucose in urine -BUN/creatinine will be elevated -If treatment is delayed, increased risk of renal failure and death -In survivors renal tubular epithelial cells can regenerate --basement membrane is intact -Tx: hemodialysis or peritoneal dialysis -Early decontamination is important -Fluid diuresis at 2x maintenance ASAP and continue for 48 hours or as long as BUN and creatinine are high |
|
|
Quercus
|

|
-Gallotanin toxin found in leaves, bark, acorns
-Hydrolyzed in the rumen to smaller compounds, compounds react with cellular proteins -Causes denaturing of cell proteins and death -Inappetance, depression, intestinal stasis, PU/PD, hard dark feces with black tarry diarrhea coming later -Teeth grinding and hunched back due to abdominal pain -Mucoid hemorrhagic gastroenteritis -Kidneys are pale, swollen, hemorrhagic -Elevated liver enzymes, increased BUN and creatinine -Severe liver and kidney damage, renal tubular necrosis and liver necrosis -Tx: fresh water and good quality hay --oral CaOH can help neutralize residual tannic acid in the rumen -IV fluids to rehydrate severely affected animals and to maintain kidney function -Animals that continue to eat have better prognosis -Can use goats as biological controls! -Icterus, red urine, dehydration |
|
|
Lupinus
|

|
-Anagyrine toxin
-Restricts fetal movement due to generalized or localized uterine contraction -Causes "crooked calf" disease -Affected calves have limb deformity, vertebral column malformation, cleft palate -Front limbs are more severely affected, deformities to elbow, carpus, and fetlock joints |
|
|
Pinus Ponderosa
|
pine tree
|
-Isocupressic acid toxin
-Causes marked decrease in uterine blood flow due to casoconstriction -Results in premature parturition -Edematous swelling of the vulva, udder, mucoid vaginal discharge before parturition or abortion -Retention of fetal membranes and secondary uterine infections are common -Difficult delivery due to poor cervical/vaginal dilation -Calves born alive are weak and compromised due to no/little colostrum production from mother -Septic necrosis of placenta and uterus, necrosis of corpora lutea -Kidney and skeletal muscle degeneration -Patchy neuronal degeneration in brain on histology -Progesterone levels progressively decline due to corpus luteum necrosis |
|
|
Veratrum californicum
|

|
-Cyclopamine, jervine, cyclopasine alkaloid toxins
-Pregnant ewes consuming plant on 14th day of gestation produce lambs with cyclopia -If eaten later in gestation (30-35 days) other defects in lambs like shortened legs and tracheal agenesis -Embryonic death can also occur -Most deformed labs are born dead or die shortly after birth -Keep sheep off pastures containing plants, especially during 1st trimester -If possible delay breeding season until after 1st killing frost in the fall |

