![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
|
Tissues |
collections of specialized cells and cell products that perform a limited number of functions. |
|
|
Histology |
is the study of tissues |
|
|
Four primary tissue types: "ECMN" |
-epithelial -connective -muscular -neural |
|
|
Epithelial Tissue: |
covers exposed surfaces or lines internal cavities or passageways and forms glands. |
|
|
Characteristics of Epithelial Tissue: 'CP' |
1. Cellularity 2.Polarity |
|
|
1. Cellularity: |
Epithelial cells are always CONtIGOUS cells bound closely together by cell junctions. In other words, there is little intercellular space. |
|
|
2. Polarity: |
Epithelial cells have exposed surfaces and surfaces for attachment with neighboring cells and tissues. These surfaces are called: 1. Apical surface 2. Basolateral surface |
|
a. Apical surface: |
for the side that faces the external or internal space lined by the epithelium |
|
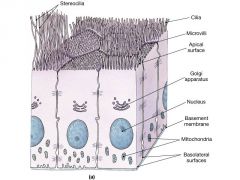
b. Basolateral surface: |
for the side attached to the underlying tissue and the sides attached to neighboring epithelial cells. |
|
|
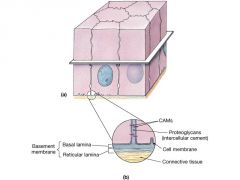
3. Attachment: |
the BASAL surface (part of the BASOlateral surface) is attached to the underlying tissue by a basal lamina (aka. basement membrane) |
|
|
4. Avascularity: |
Refers to the absence of blood vessels. Nutrients are obtained by diffusion or absorption across the apical and basal surfaces. |
|
|
5. Regeneration: |
Cells that become damaged, worn out or abraded are replaced by division of STEM CELLS. |
|
|
6.Arranged into Sheets or Layers |
Epithelial cells are arranged in layers one or more cells thick. |
|
|
Functions: 1. Physical Protection: |
Protects tissue from abrasion, dehydration, and damaging chemical or biological agents. |
|
|
2. Control Permeability: |
Controls the passage of material into (absorption) and out of (secretion) tissue. |
|
|
3. Provide Sensation: |
Epithelium has nerve ending and specialized epithelium cells that detect environmental changes. A NEUROEPITHELIUM is specialized sensory epithelium. |
|
|
4. Produce Specialized Secretions: |
GLANDS are derived from epithelial cells. |
|
|
The epithelium is GLANDULAR EPITHELIUM when... |
most or all epithelial cells produce secretions.
|
|
|
These glands are derived from epithelial tissue: |
Endocrine and Exocrine
|
|
|
Specializations of Epithelial Cells:
Epithelial cells specialized for absorption or secretions have.... |
MICROVILI on the apical surface that increase the surface area for exchange of materials.
|
|
|
Stereocilia:
|
are very long microvilli that are found along portions of the male reproductive tract and on receptor cells of the inner ear. |
|
|
Ciliates epithelium : |
has CILIA on the apical surface to move fluids. Ciliated epithelium is typical of the upper respiratory tract. Cilia are also found on the epithelial cells lining the oviducts. |
|
|
Maintaining the Integrity of Epithelium: maintained by CELL JUNCTIONS |
1. Intercellular Connections2. Attachment to Basal Lamina (Basement Membrane) 2. Attachment to Basal Laminia (Basement Membrane). |
|
|
a. lamina lucida: b. lamina densa: |
a. A layer next to the epithelium containing glycoproteins and a network of microfilaments b. A layer next to the connective tissue contains protein fibers produced by the connective tissue cells. |
|
|
3. Maintenance and Repair:
|
-cell renewal -Germinative (stem) cells continually divide to replace cells lost due to wear and tear. |
|
|
Basis for Classification: 1. Layers ex: Simple Epithelium |
-one layer thick -found in protected areas such as VENTRAL BODY CAVITY, heart chambers and lining of blood vessels. -involved with secretion, absorption and filtration |
|
|
2. Shape of Cells |
-has more than one layer of cells resting on the basal lamina and is subjected to mechanical or chemical stresses. |
|
|
Classification of Epithelium: Simple Squamous |
Very delicate and the thinness of the cells readily allow molecules to pass through it. Found in regions where rapid exchange of molecules is needed such as the AVEOLI of lungs and ENDOTHELIA of capillaries.
-provides slippers surface for there serous (watery) membranes on the ventral body cavity |
|
|
a. Mesothelium: |
refers to the simple squamous epithelium that lines the ventral body cavity |
|
|
b. Endothelium |
is the simple squamous epithelium that lines the interior of the heart chambers and blood vessels. |
|
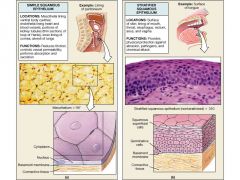
Stratified Squamous |
the type of epithelium that typically consists of many layers of cells and is found where mechanical stresses are severe. Stratified squamous can be further subcategorized into: |
|
|
a. Keratinized: b. Nonkeratinized: |
a. The apical layers of epithelial cells become packed with intermediate filaments of KERATIN; a protein that gives toughness and water-resistance b. The apical layers lack water resistance and must be kept moist by glandular secretions. Found lining the oral cavity, esophagus, rectum, anus, and vagina. |
|
|
Simple Cuboidal |
This type of epithelium sometimes lines the ducts of sweat glands and the larger ducts of exocrine glands. |
|
|
Transitional Epithelium |
-is stratified with plump cuboidal cells on the surface. -is designed to accommodate the stretching that occurs in the urinary bladder and ureters while maintaining the impermeable barrier these locations require. |
|
|
Simple Columnar |
-is simliar to simple cuboidal except that the cells appear taller than wide -provides some protection and is found in regions where active absorption or secretion cures including the stomach, intestinal tract, uterine tubes, and excretory ducts. -cells show distance polarity with the nuclei crowded into a band near the basal lamina |
|
|
Pseudostratified Columnar |
-there is only a single layer of cells but there are appears to be multiple layer because of the varying locations of the nuclei -typically found lining the upper respiratory tracts as pseudo stratified ciliated columnar epithelium (PCCE) also male reproductive tract |
|
|
Stratified Columnar |
is rare and is found lining portions of the pharynx, urethra, anus, and large ducts |
|
|
Glandular Epithelium |
-may develop into gland cells that produce secretions.
|
|
|
Classifications of Glands: 1. Type of Secretion |
-Exocrine secretions are discharged onto the epithelial surface. Glandular cells may move away from the epithelial surface but remain connected by tubes called DUCTS. -secret mucins, enzymes, water and waste products. |
|
|
Nature of Secretion: a. Serous |
-glands that secrete a watery secretion containing enzymes |
|
|
b. Mucous |
-glands the secrete mucins that absorb water to form MUCUS |
|
|
c. Mixed |
-glands that contain a mixture of cells secreting both serous and mucous secretions. |
|
|
Endocrine: |
-cells that secret by exocytosis into the fluid surrounding the cell. -may either be single cells or aggregation of cells and secret HORMONES that serve as chemical messengers. SUCH AS: thyroid, adrenal or pituitary glands, are DUCTLESS |
|
|
2. Gland Structure: Unicellular: |
-glands that are single secretory epithelial cells. The only unicellular glands are GOBLET CELLS that secret mucins. |
|
|
Multicellular glands include: a. Glandular epithelium: |
in which all the surface cells are secretory. the epithelium that lines the lumen of the stomach is an example. |
|
|
b. Aggregations of glandular cells... |
-move away from the surface and form either exocrine or endocrine glands. -multicellular exocrine glands have 2 components that results in further subclassifications, the secretory portion and the duct. |
|
|
The secretory portion may either be: 1.Tubular 2. Alveolar or acing 3. Tubuloalveolar |
1. when the cells are arranged in tubes 2. when the cells are arranged in blind pockets. 3. when both configurations are present. |
|
|
Ducts may either be:
1. Simple 2. Compound |
1. when it is unbranched 2. when it is branched |
|
|
3. Modes of Secretion: a. Merocrine |
glands are the most common and release their secretions by exocytosis. |
|
|
b. Apocrine |
glands release their secretions by detachment of an APICAL PORTION OF THE CYTOPLASM. |
|
|
c. Holocrine |
glands release their secretions with the disintegration of the entire cell. |
|
|
Connective Tissues |
is found throughout the body but is never exposed to the environment |
|
|
Three Basic Components: 1. Specialized Cells 2. Extracellular Protein Fibers 3. Ground Substance |
1.-MATRIX that surrounds the cells with: 2. " " 3. A viscous, clear substance with a slippery feel and a high water content and very large macromolecules including PROTEOGLYCANS and GLYCOSAMINOGLYCANS. |
|
|
Functions: |
1. Establishes structural framework for the body e.g. bone, cartilage 2. Transports fluids and materials throughout the body. e.g blood, lymph 3. Provides protections for delicate organs e.g bone of skull, rib cage, spinal column. 4. Supports, surrounds and interconnects other tissue types. e.g. Fascia, tendons, organ capsules. 5. Stores energy. e.g adipose tissue. 6. Defends body from invasion. e.g. inflammatory cells reside and migrate through connective tissue. |
|
|
Classifications: |
connective tissue can be placed in one of three broad categories: |
|
|
1. Connective Tissue Proper Loose/dense CT |
this type is literally connecting or binding the other tissue and hence is "proper"ly speaking connective tissue |
|
|
2. Fluid Connective Tissue |
is connective in a broader sense in that it allows substances to move from one part of the body to another, e.g blood and lymph. Matrix is essentially a fluid rather than a gel or solid. |
|
|
3. Supporting Connective Tissue |
This connective tissue supports the body against the forces of gravity but also provides physical protection and functions as levers upon which muscle can exert force, e.g cartilage and bone. |
|
|
Connective Tissue Proper 1. Cells Fixed Cells: a. fiberblasts/Fibrocysts |
-These cells are always present in connective tissue proper and is the most abundant cell found there. -Fibroblasts SECRETE PROTEIN SUBUNITS that form extracellular fibers (collagen and elastic fibers) and molecules that form the ground substance. -Differentiate from fibroblasts and maintain the connective tissue fibers of the tissue. HYALURONAN is secreted and gives the ground substance its viscous consistency. |
|
|
b. Fixed Macrophages (Histiocytes) |
-Defensive cells that engulf damaged cells and pathogens. -not as abundant as fibroblasts but when mobilized for defense or repair attracts other cells of the immune system. |
|
|
c. Adipocytes (Fat Cells) |
-These cells contain lipid inclusions that push other organelles to the edge of the cell. -the number of adipocytes will vary in different regions of the body and in different individuals. |
|
|
d. Mesenchymal Cells |
These are stem cells that can divide and differentiate into the other specialized cells when needed. |
|
|
e. Mast Cells |
they secrete HISTAMINE and HEPARIN in response to injury and infection. This results in local inflammation. |
|
|
f. Melanocytes |
-gives pigmentation -is an inclusion -absorbs UV radiation -synthesizes MELANIN |
|
|
Wandering Cells: a. Free Macrophages |
-Phagocytic cells that circulate in the blood as MONOCYTES and migrate rapidly through connective tissue. -these cells are recruited to areas of infection or tissue damage by fixed macrophages |
|
|
b. Lymphocytes |
-These cells migrate throughout the body and provide the body with specific immunity - Lymphocytes that actively produce ANTIBODIES are called PLASMA CELLS |
|
|
C. Neutrophils and Eosinophils |
These are phagocytic cells that are smaller than macrophages and are attracted to areas of infection and injury by chemicals released by cells already at the site. |
|
|
2. Connective Tissue Fibers |
all tissue fibers are assembled from protein subunits by FIBROBLASTS |
|
|
a. Collagen |
-Collagen fibers are the most common and strongest fibers. -These fibers combine tensile strength with flexibility |
|
|
b. Reticular Greek: Rete- "little net" or "mesh" Stroma= "bed" or " cells to rest on" |
-has many RETICULAR FIBERS -forms the STROMA ( the mesh keeping cells in position) in various organs -not as strong as collagen fibers -PARENCHYMA - refer to the cells of the organ performing the function. |
|
|
c. Elastic |
-ELASTIN -Recoil property -give greater RESILIENCE -walls of BVs--- transitional epithelium |
|
|
3. Ground Substance |
-clear, colorless and of a thick consistency (like maple syrup) -this is the substance that surrounds the cells and fibers. It contains HYALURONAN and proteoglycans and glycoproteins. |
|
|
Types of Connective Tissue Proper:
EMBYRONIC TISSUES: Embryonic Tissue a. Mesenchyme |
-connective tissue found in the embryo (unspecialized) cells in a matrix with fine fibers. -differentiate into other kinds of tissue including adult connective tissue cells. |
|
|
b. Mucous Connective Tissue |
-embryonic connective tissue found in the umbilical cord. -the extracellular matrix is like gelatin in consistency and is often referred to as WHARTON'S JELLY |
|
|
2. Loose Connective Tissue: ("packing material") a. Areolar Connective Tissue |
-LEAST SPECIALIZED -HAS ALL THE CELLS AND FIBERS found in connective tissue proper. -immediately under the dermis. -HIGHLY VASCULAR -provides MAJOR PATHWAY FOR CELLS OF THE IMMUNE SYSTEM to reach sites of damage or invasion. |
|
|
b. Adipose Tissue |
-difference are arbitrary; as areolar tissue is considered adipose tissue when there is a high concentration of ADIPOCYTES. |
|
|
c. Reticular Tissue |
- predominance of RETICULAR FIBERS -it forms the STROMA in various organs including liver, spleen, lymph nodes and bone marrow. |
|
|
3. Dense Connective Tissue "TALE" |
1. Tendons 2. Aponerouses 3. Elastic Tissue 4.Ligaments |
|
|
a. Dense Regular Connective Tissue |
-HIGH concentration of collagen fibers ---> arrayed in parallel |
|
|
1. Tendons |
-form cords that attach muscle to bone |
|
|
2. Aponeuroses "flat-sheet" |
-parallel arrays form flat sheets of connective tissue that connect flat muscles to their attachments. |
|
|
3. Elastic Tissue |
-give greater resilience -found in the wall of large blood vessels, underlying transitional epithelium and surrounds respiratory passages. |
|
|
4. Ligaments |
-similar to tendons -often contain a sig. number of ELASTIC FIBERS -ELASTIC LIGAMENTS have a predominance of elastic fibers - attaching BONE TO BONE |
|
|
b. Dense Irregular Connective Tissue
|
-Bundles of collagen fibers -EX: dermis of skin -> fibrous coverings on surface of cartilage and bone. -forces from MANY directions -ex. also forms tough CAPSULES AROUND ORGANS AND JOINTS |
|
|
Supporting Connective Tissue 1. Cartilage: |
-the matrix contains CHONDROITIN SULFATE and KERATIN SULFATE, that forms links with protein molecules -FIRM but pliable -the matrix is produced by both CHONDROBLASTS and CHONDROCYTES and is maintained by CHONDROCYTES -chondrocytes exist in spaces of the matrix called LACUNAE |
|
|
Cartilage is.... |
avascular and all nutrient and waste product exchange occurs by diffusion through the matrix. |
|
|
Formation and Growth: Cartilage grows by two mechanisms: |
Appositional growth: -fibroblasts of the cellular layer of the PERICHONDRIUM differentiate into chondroblasts that produce matrix and become chondrocytes when embedded in matrix. |
|
|
Interstitial growth: |
-chondrocytes within the MATRIX divide by mitosis and produce additional matrix that cause internal expansion of cartilage. |
|
|
Types of Cartilage: |
a. Hyaline Cartilage (hyaline means "glassy") b. Elastic Cartilage c. Fibrocartilage |
|
|
a. Hyaline Cartilage |
-most common type -connects ribs to sternum as COSTAL CARTILAGE -supports conducting passages ( larynx, trachea and bronchi) -forms ARTICULAR SURFACES of moveable joints |
|
|
b. Elastic Cartilage: |
-very resilient -found in the PINNAE of outer ear, EPIGLOTTIS and CUNIFORM CARTILAGES of the larynx and supporting the AUDITORY CANAL |
|
|
c. Fibrocartilage: |
-dense regular connective tissue and hyaline cartilage -tougher and durable -found in intervertebral discs, pubis symphysis, and in menisci of the knee and temporomandibular joints. |
|
|
Membranes: 4 types of membranes |
1. Mucous Membranes -continuous with the exterior -include digestive, urinary, reproductive and respiratory tracts -lining is kept moist by secretions including MUCUS from MUCOUS GLANDS -the areolar CT that attaches the epithelium to basal lamina is called LAMINS PROPRIA |
|
|
2. Serous Membranes |
-very thin and transparent and line compartments of the VENTRAL BODY CAVITY |
|
|
a. Pleura |
the lining on the LUNGS and the PLEURAL CAVITIES in which the lungs are found.
|
|
|
b. Peritoneum |
the lining of the ABDOMINOPELVIC CAVITY and all organs situated there. |
|
|
c. Pericardium |
lining on the surface of the HEART and the PERICARDIAL SAC that surrounds heart |
|
|
Mesothelium |
-simple squamous epithelium of a serous membrane. |
|
|
Areolar connective tissue.... |
is a thin underlying layer of tissue -allowinf fluid to seep through and form a TRANSUDATE. (contributing to the smooth and slippery nature) |
|
|
3. Cutaneous Membrane |
-aka. SKIN. -keratinized stratified squamous epithelium attached by areolar connective tissue to a layer of dense connective tissue - |
|
|
4. Synovial Membrane |
-found within joint capsules -composed of areolar connective tissue incompletely lined by "epithelial" cells. -Secretory cells secrete SYNOVIAL FLUID that lubricates and nourishes the hyaline cartilage of the joint. |

