![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
430 Cards in this Set
- Front
- Back
|
DDx for delirium / AMS |
IS IT / MEATS
I nfection S tructural/S eizure/S troke I CH/I schemia T rauma/T hrombus M etabolic E ndocrine/E nvironment A noxia/A bnormal pCO2 T oxins/T ablets/T oo little (withdrawal) pS ychiatric |
|
|
Intubation preparation |
STOP I C BARS |
|
|
Diagnosing the cause of an alarming ventilator |
D - Dislodged tube |
|
|
CHF treatment
|
POND |
|
|
Ingestions that are not absorbed by activated charcoal |
PHAILS
Pesticides Hydrocarbons Acids/Alkalis/Alcohols Iron Lead/Lithium Solvents |
|
|
Causes of anion-gap metabolic acidosis
|
KULT |
|
|
Hydrocarbon additives that require GI decontamination |
CHAMP
Camphor - seizures Halogenated HC - dysrhythmias/hepatotoxicity Aromatic HC - bone marrow suppression/cancer Metals (arsenic, murcury & lead) Pesticides - cholinergic crises/seizures/resp depression |
|
|
Mass casualty triage protocol |
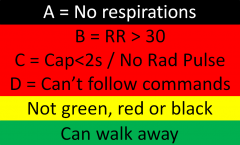
Use the START (Simple Triage And Rapid Treatment) Protocol
Remember with ABCD |
|
|
PERC Rule
|
Apply if clinical gestalt = low risk for PE |
|
|
CATCH Rule - High Risk Criteria |
WIGS
W - Worsening Headache I - Irritability G - GCS <15 2 hours after the injury S - Suspected open/depressed skull # |
|
|
CATCH Rule - Medium Risk Criteria
|
SDH |
|
|
Causes of Seizure
|
STATUS EPILEPsy |
|
|
Signs of Delirium (for Confusion Assessment Method, CAM)
|
AIDA
A - cute and fluctuating I - nattention D - isorganized thinking - incoherent, rambling A - ltered LOC - stuperous, agitated, hyper-alert, lethargic, drowsy |
|
|
What is needed for a safe discharge plan?
|
No RISKS |
|
|
Diagnostic criteria of major depressive disorder |
MDD classified as 5 or more of these symptoms occurring most days over a 2 week period along with a change in function. MUST have depressed mood or loss of interest/function.
SIGECAPS
Not a mixed episode, due to anxiety, caused by a general medical condition, or consistent with bereavement (<2 months from loss) |
|
|
Approach to the Alarming Ventilator |
D - Disconnect the patient from the ventilator +/- provide gentle pressure to the chest (assess for and treat breath Stacking and Equipment failure) |
|
|
Ottawa SAH Rule |
A - Age > 40y |
|
|
Ring enhancing lesions on Head CT |
MAGICAL DR A - Acute Disseminated Encephalomyelitis L - Lymphoma
D - Demyelinating disease |
|
|
Anterior cord syndrome
|
Like a car - if it smashes the front the engine won't work (paralysis) but instruments/GPS will (soft touch and proprioception)
|
|
|
What are the NEXUS Criteria? |
2 Exam
-Neurologic deficit -Midline cervical tenderness 3 Credibility -Normal GCS -Not intoxicated -No distracting injuries |
|
|
Unstable C-Spine Fractures |
Jefferson Bit Off A Hangman's Tit And Pinky A ny fracture-dislocation P osterior neural arch of C1 |
|
|
Approach to bradycardia |
DIE!
Drugs (BB, CCB, Dig) Infarction Electrolytes (especially K!) |
|
|
Rashes that start on the palms
|
Sifting Rocks Scabbed Emma's Hands |
|
|
Rashes with a + Nikolsky sign |
Stevie got scalded by TEN PV'd nickels
Steven-Johnson Syndrome Staph Scalded Skin Syndrome Toxic Epidermal Necrolisis (TEN) Pemphigus vulgaruS (PV) Nikolsky |
|
|
Rashes with vesicle / bullae
|
Old man with BPPV fell into a pool of necrotizing gonorrhea
Bullous Pemphigoid / Pemphigus Vulgarus Necrotizing fasciitis (hemmorhagic) Gonorrhea (disseminated) |
|
|
Rashes with petechiae / purpura |
Henoch the Tick gave Meningitis to DICk the purple drug addict |
|
|
Exam findings of serotonin syndrome |
CHARM |
|
|
Depression symptoms |
SIGECAPS |
|
|
Suicidal ideation assessment |
SADPERSONS scale correlates with the decision to admit to psychiatry. Does not predict risk of future suicidality.
S ex (male) - 1
<6 - Outpatient >6 - ED psych evaluation >9 - Psych admission |
|
|
Major and minor criteria for Rheumatic Fever. Treatment. |
Jones criteria (requires evidence of strep infection + 2 major or 1 major/1 minor)
MAJOR J - oints - polyarthritis of large joints (knees, elbows, wrist, ankles) <3 - carditis (murmurs, effusions, cardiomegaly, CHF) N - Nodules - subcutaneous on extensor surfaces (wrist, elbow, knees, spine) E - Erythema marginatum (painless, non-pruritic) S - Sydenham's Chorea
MINOR F - Fever A - Arthralgias C - CRP E - ESR P - PR interval increased
Treatment -Penicillin x 10 days or Benzathine penicillin 1million units IM; long-term prophylactic antibiotics -Aspirin -IVIg |
|
|
Criteria for diagnosing Endocarditis |
Duke's criteria () BE FIVER (+ if 2 major, 1 major 2 minor, 5 minor)
B - Blood cultures (2 positive with typical pathogens) E - Echo lesions (vegetation, perivalve abscess, prosthetic valve dehisence, new regurgitation)
F - Fever (>38) I - Immunologic (Roth, Osler, rheumatoid factor) V - Vascular (Janeway, septic emboli, conjunctival hemorrhage) E - eccentric blood culture (single positive culture unless organism does not cause IE) and echo (consistent with IE but do not meet criteria) R - risk factors (IVDU, prosthetic valve) |
|
|
San Francisco Syncope Rule |
CHESS CHF Hematocrit <30% ECG SOB Systolic BP <90 |
|
|
Dangerous ECG findings on an ECG of a patient with syncope |
Prolonged QT WPW Brugada HOCM Ischemia |
|
|
Causes of hyperacute T waves |
Ischemia Hyperkalemia Pericarditis LVH LBBB Benign early repolarization |
|
|
Causes of tall R wave in v1 |
Posterior MI RBBB WPW type A Children and adolescents Dextrocardia |
|
|
Causes of ST elevation on ECG |
STEMI Printzmetal's LBBB LVH Pericarditis Hyperkalemia Brugada PE Celebral hemorrhage Pacing BER |
|
|
How can VT be distinguished from SVT with aberrancy? |
Brugada criteria (note: not good enough to use in real life): 1. Absence of any RS complexes in the chest leads |
|
|
What are the common pacemaker malfunctions? |
Failure to capture - lead displacement or break, block or battery Oversensing - sensing T waves or extracardiac stimulus Undersensing - poor lead connection or break, small amplitude, poor contact Inappropriate rate - battery, response to atrial dysrhytmias |
|
|
What is the code for pacemaker type? |
Chamber paced - A, V, D Champer sensed - A, V, D Response to sensing - Inhibit pacing (V or A and V) or Trigger pacing (old) Programming - simple, programmable, rate adaptive, communicating, none Antitachy response - pace or shock |
|
|
Complications of ICD and pacemaker placement |
Infection of wound Infection of pouch Thrombophlebitics Chronic thrombosis |
|
|
Indications for a pacemaker |
High level block: -And symptomatic brady -And asystole >3s (AFib pauses >5s) -Following AV ablation -With neuromuscular disease -Intermittently with bi or trifascicular block -With exercise
|
|
|
Indications for an ICD |
1. Cardiac arrest from VF or VT not caused by a reversible event |
|
|
Etiology of Pericarditis |
-Infectious (Viral, Bacterial, Fungal, Parasite, Rickettsia) -Postinjury (Trauma, Surgery, Myocardial infarction, Radiation) -Metabolic diseases (Uremia, Medications) Tumors |
|
|
List the hypertensive emergencies and their ideal treatment. |
ACS - nitroglycerine, labetolol Heart failure - nitroglycerine, furosemide Dissection - esmolol & nitroprusside OR labetolol Ischemic stroke - nicardipine, labetolol Intracerebral hemorrhage - nicardipine, labetolol Hypertensive encephalopathy - nicardipine, labetolol Kidney injury - fenoldopam, nicardipine Preeclampsia - magnesium and labetolol Sympathetic crisis - phentolamine |
|
|
What features distinguish orbital cellulitis from periorbital cellulitis? |
Proptosis, opthalmoplegia, and visual changes (look for afferent pupillary defect secondary to increased IOP). |
|
|
Differential diagnosis for a NAGMA |
HARDUPS Hyperalimentation / TPN Acetazolamide RTA Diarrhea Ureteral diversion Pancreas Spironolactone |
|
|
Niacin deficiency |
aka Vitamin B3 and results in Pellagra
4D’s: Diarrhea Dermatitis Dementia Death |
|
|
Thiamine deficiency |
aka vitamin B1
Wernicke's Encephalopathy- WACO: ataxia, confusion, opthalmoplegia Korsakoff's Psychosis - irreversible short-term memory loss Beri-beri - high output heart failure secondary to vasodilation and fistula formation |
|
|
Cobalamin deficiency |
aka vitamin B12
Megaloblastic anemia Neurologic changes (paresthesias, ataxia, clonus, memory loss) Psychiatric (depression, psychosis)
Folate looks the same except NO neurologic changes and it happens faster. |
|
|
Causes of non-cardiogenic pulmonary edema |
IS NOT THE HEART
I nhaled Toxins (Ammonia, Chlorine, Phosgene, Nitrous oxide)
N eurogenic (seizure, strangulation, trauma)
T rauma
H igh altitude pulmonary edema |
|
|
Diagnostic criteria of Multiple Myeloma |
-Monoclonal plasma cells or plasmacytoma in the bone marrow -Monoclonal protein in blood or urine -Organ dysfunction (CRAB criteria) C - HyperCalcemia R - Renal failure A - Anemia B - Bone damage (lesions or osteoporosis) |
|
|
What cancers cause bone mets? |
Painful Bones Kill These Suckers Prostate Breast Kidney Thyroid Skin
Also Lungs |
|
|
Hard signs of vascular injury |
HARD Bruit
Hypotension Arterial Bleed Rapidly expanding hematoma Deficit (pulse/neuro) Bruit/thrill |
|
|
Criteria to call a febrile seizure simple |
6 months to 6 years 1 episode in 24 hours Duration <15 minutes Generalized No neurological history |
|
|
HELLP Syndrome |
Hemolysis
Elevated Liver enzymes
Platelets |
|
|
Kawasaki Disease criteria |
Warm CREAM
Warm - fever >5 days C - Conjunctivitis R - Rash (erythematous, maculopapular, morbilliform) E - Erythema of palms/soles with swelling A - Adenopathy (cervical) M - Mucous membranes (dry, red, strawberry tongue) |
|
|
Tetrology of Fallot cardiac anomolies |
-Boot shaped heart (Fall over your own Boots) -Pulmonary hypertension, VSD, RVH, Overriding Aorta -Ductal dependent lesion that crash after PDA closes (2-10 days, treat with PGE1 0.1mcg/kg/m) Tet spells (knees to chest to increase SVR and O2 to decrease PVR)
|
|
|
Congenital Adrenal Hyperplasia abnormalities |
21-hydroxylase deficiency Low Na and High K Virulized females, small penis in boys Treat with glucose and hydrocortisone |
|
|
Abuse fracture patterns |
ANY in a child <1yo Bucket Corner** Diaphysis of humerus, radius, femur, tibia (especially <3yo) Rib** Scapular** Spinous process** Sternum** Skull (stellate)* Vertebral* Digits* Multiple* or Bilateral Different stages of healing* |
|
|
Psychological signs of child sexual abuse |
Very broad definition
Regression Acting out Sexualized behavior Disclosure |
|
|
The crashing neonate |
THE MISFITS T rauma / abuse H eart disease / H ypothermia / H ypoxia E ndocrine (CAH, hyperthyroid) M etabolic (hypoglycemia, hyponatremia, hypocalcemia) I nborn errors (ammonia) S epsis (most common!) F ormula mishaps I ntestinal catastrophes (volvulus, NEC, diaphragmatic hernia) T oxins (home remedies) S eizures |
|
|
Cyanotic heart disease |
Increased lung markings 1-Truncus arteriosis 2-Transposition of the great arteries 5-Total anomalous venous return
Decreased lung markings 3-Tricuspid atresia / pulmonary atresia 4-Tetrology of Fallot
|
|
|
Congenital heart disease: Obstructive Lesions |
Also happen with closure of the duct, but NOT cyanotic. Give them 0.1mcg/kg/m of PGE1
Coarctation of the aorta Hypoplastic left heart syndrome Interrupted aortic arch Aortic stenosis (critical) |
|
|
List some symptoms of lead poisoning |
L - Lead lines E - Encephalopathy A - Anemia with basophilic stippling D - Drop (wrist) |
|
|
Outline the phases of iron poisoning |
I GI effects (hemorrhagic GI effects) x 6 hours II Quiscient x 12 hours III Systemic (vasodilatory shock; hepatorenal dysfunction) IV Liver failure V Resolution (GI scarring, stomach obstruction) |
|
|
Pelvic avulsion fractures (muscle attachments and bony anatomy) |
|
|
|
Anticholinergic Toxidrome |
Blind as a bat (Mydriasis) Mad as a hatter (Altered mental status) Red as a beet (vasodilation, flushed) Hot as a hare (febrile) Dry as a bone (no secretions/diaphoresis) Bowel and bladder lose their tone Heart runs alone (tachycardia)
Atropine, antihistamines, scopalamine, antipsychotics |
|
|
Cholinergic Toxidrome |
SLUDGE and the killer B's Salivation Lacrimation Urination Defication Gastro upset Emesis Bradycardia, Bronchorrhea, Bronchospasm
Also mioisis and lethargy Organophosphates, carbamates, mushrooms |
|
|
Approach to CT Head |
Blood Can Be Very Bad
Blood Cisterns Brain Ventricles Bone
|
|
|
Approach to CXR |
ABCS
Airway Breathing (lungs) Cardiac (heart) Skeleton and Soft tissues |
|
|
Substances that are radioopaque on x-ray |
CHIPES Chloral hydrate Hydrocarbons (especially halogenated ones) Iron Phenothiazines Enteric coated Solvents (some of them) |
|
|
Associations with Ciguatera toxicity |
Big fish (grouper, barracuda) -Anticholinesterase (cholinergic) effects -Gastroenteritis -Hot/cold reversal of sensation or cold allodynia -Teeth feel loose -Brady / resp arrest Treat with antihistamines (treat the itch), atropine, amitryptaline (allodynia), mannitol (controversial) |
|
|
Associations with Scombroid |
Poorly refrigerated fish (Tuna, mahi mahi) Histidine in decomposing fish gets broken down into histamine -Rapid flushing to head/face/torso -Gastroenteritis |
|
|
What is VATER Syndrome? |
AKA VACTERAL Association, these conditions occur together more commonly than would be expected otherwise Vertebral anomolies Anal atresia Cardiac defects Tracheo-esophogeal fistula Esophageal atresia Renal anomolies Limb defects |
|
|
DDx for febrile and altered mental status patients |
SWEAT Sepsis Withdrawal Endocrine (thyroid) & Environment (heat stroke) Agitated delirium Toxidromes (sympathimetic, anticholinergic, amphetamines, salicylates, SS, NMS, MH, strychnine, hallucinogens) |
|
|
General approach to the intoxicated patient |
ABCDDDEF Airway Breathing Circulation Dextrose Decontamination Diagnosis (ECG, VBG, acetaminophen, ASA, osmolality, EtOH) Exposure (features of toxidrome) Elimination (enhance it) Find an antidote |
|
|
TCA mechanisms of action |
TCA Thinker 1 – Indirect GABA antagonism (seizures) Cardiac 4 - Na channel blockade in phase 0 of cardiac depolarization (wide QRS, impaired inotropy) Anti 7 – Anticholinergic (delirium, seizures, sedation, coma, prolonged gastric emptying) |
|
|
Sternbach's criteria for serotonin syndrome |
Recent serotonergic med/med increase, no recent neuroleptics, no other cause, and 3 CAN features Cognitive -Agitation, Confusion, Delirium, Hypomania Autonomic instability -Tachy, HTN, shiver, diaphoresis, mydriasis, diarrhea Neuromuscular activity Fever, ataxia, tremor, hyperreflexia, myoclonus, muscular rigidity |
|
|
Plants and animals containing cardiac glycosides |
FLOWeRY BF Foxglove Lily of the valley white Oleander Weed of milk Red squill Yellow oleander
Bofo toad Firefly
|
|
|
What are the indications for monitoring/admission after electrical injury? |
Clinical -Cardiac arrest, LOC, hypoxia, chest pain, suspected conductive injury, other injury requiring admission ECG -Abnormal or dysrhythmia has occurred Risk factors -Known CAD -Risk factors for CAD |
|
|
What is the feathering cutaneous burn caused by a lightning strike called? |
Lictenburg figure |
|
|
How do high voltage electrical injuries differ lightning injuries? |
More often, high voltage electrical injury causes -Rhabdomyolysis -Compartment syndrome -Kissing burns -Mouth burns
But does not cause -Lictenburg figures -Karaunoparalysis |
|
|
How do humans transfer heat? |
Conduction - from a warmer to cooler object through direct physical contact Convection - loss to circulating air and water molecules Radiation - transferred by electromagnetic waves Evaporation - conversion of liquid to gas |
|
|
Contrast heat cramps, heat edema, heat syncope, prickly heat |
Cramps - due to fluid replacement with hyptonic fluids Edema - vasodilation causes pooling which leads to swelling Syncope - vasodilation and dehydration lead to decreased CO and fainting Prickly heat - obstruct the sweat pores, staph infection, vesicular rash - treat with chlorhexidine cream |
|
|
What is the difference between classic and exertional heatstroke? |
Classic is in older people with chronic disease in high temperatures, sweating is absent, rhabdo and ARF are rare, lactate is BAD
Exertional is in young people exerting themselves, sweating is common, rhabdo and ARF are common, and lactate is less bad |
|
|
List the ways that a patient can be rewarmed from hypothemic states |
Active external: -Bair hugger, AV anastomosis, hot water immersion, heating pads, hot water bottles, radiant heat lamp, negative pressure rewarming Active internal -Humidified ventilation, warm IVF, thoracic bladder gastric myocardial or colonic lavage, peritoneal dialysis, ECMO +/- diathermy |
|
|
Causes of syncope |
P ressure (hypotensive causes)
A rrhythmias - Bradyarrhythmias, Tachyarrhythmia's (SVT, NSVT, A.F.), pacemaker malfunctions
S eizures
S ugar (hypo / hyperglycemia)
O utput (cardiac) - AS, PS, MS, IHSS, Cardiomyopathies, Atrial Myxoma, Cardiac Tamponade, Aortic Dissection, MI, CHF
O 2 (hypoxia) - PE, Pulm HTN, COPD exacerbation, CO poisoning
U nusual causes - Anxiety, Major depressive disorder, Panic disorder, Hyperventilation syndrome, Somatization disorder
T ransient Ischemic Attacks & Strokes, CNS dz's |
|
|
Describe the Haddon matrix |
Matrix to assess and modify factors related to injury
HAVE Host Agent Vector/Environment
Before, during, and after injury |
|
|
List 3 strategies used to decrease injuries |
The E's
Education - teaching at risk populations how to prevent injury Engineering - design safety into the environment (e.g. highway design) Enforcement - of laws requiring safer behavior (e.g. seatbelts) |
|
|
Hemiparesis ipsilateral to a pupil blown secondary to increased ICP |
Kernohan's notch syndrome secondary to uncal herniation compressing the contralateral cerebral peduncle. It results in 'false localization' |
|
|
Layers of the scalp and associated hemorrhage |
SCALP Skin Connective Tissue (Caput succedaneum) Aponeurosis galea Loose areolar tissue (Subgaleal hematoma) Periosteum (Cephalohematoma limited by sutures) |
|
|
How can we assess for pseudosubluxation on pediatric c-spine x-rays? |
Most commonly C2-C3 Look at spinolaminar (Swischuk's) line drawn from anterior cortex of the C1 to C3 spinous process. If the line is >2mm anterior to the anterior cortex of C2 suspect a posterior element fracture. |
|
|
Differences in the pediatric versus adult airway |
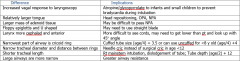
|
|
|
Anatomic differences in pediatric patients that change response to trauma |
-Small size = more multitrauma -Less protective fat/muscles = more internal organ injuries (liver, spleen, kidneys) -Elastic chest wall = lung injury without # -Open growth plates = different fracture patterns -Large surface area = quicker hypothermia -Faster metabolic rate = quicker desat, hypoglycemia -Better at maintaining BP = tachy as only sign of shock -Bigger head-to-body, thin skull, less myelin = more head injuries -More elastic vertebral column = more SCIWORA -Bigger head = higher fulcrum = C2-3 versus C6 injuries more common |
|
|
Anatomic difference in pregnant patients that change response in trauma |
Airway - more friable and edematous mucosa, lower esophageal sphincter tone, increased abdominal girth
Respiratory - higher RR = greater minute ventilation and lower CO2; higher diaphragm = lower FRC (quicker desat) and req's higher chest tube
Cardiac - Increased blood volume, tachycardia, decreased PVR, increased venous congestion/pressures, lots of blood to uterus, aortocaval compression when supine
Heme - dilutional and Fe-deficiency anemia; hypercoaguable
Abdomen - displaced contents; decreased sensitivity of exam for peritonitis; ALP doubles; decreased GB contractility (increased gallstones; weight gain
Nephro - bladder is extrapulvic after 12 weeks; decreased GFR; polyuria and hydropnephrosis due to bladder compression
MSK - widened pubic symphesis (4 -> 8mm) |
|
|
How can we assess for atlanto-occipital dislocation on pediatric c-spine x-rays? |
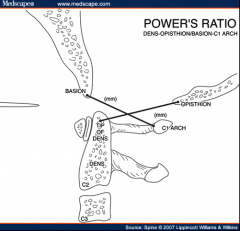
Use power's ratio (should be <1): Basion to anterior cortex of C1 spinous process Opisthion to posterior cortex of dens
Also Basion-Dens & Basion to posterior axillary line should be <12mm
|
|
|
Tube sizes in pediatrics |
Broselow tape ETT = (age/4) + 4 (uncuffed - drop 0.5-1 size for a cuffed tube) Chest tube = ETT size x 4 Foley / NG tube = ETT size x 2 |
|
|
Anatomic difference in elderly patients that change response in trauma |
General - on medications Cardiac - decreased reserve, can't increase HR Pulmonary - decreased compliance and increased chest wall rigidity, brittle bones Neurologic - brain atrophy increases mobility and shearing of bridging veins (SDH); dura is fused so less EDH Derm - skin is thin and brittle, easier to lacerate and tear, forms ulcers quicker MSK - osteopenia so increased fractures, decreased joint mobility, spinal stenosis |
|
|
Approach to hyponatremia |
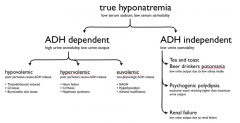
|
|
|
Effects of typical antipsychotics |
HOT DAMN
Fever Dopamine receptor blockade Alpha blockade Muscarinic blockade Na/K channel blockade (wide QRS and long QTc) |
|
|
Addictions that can kill in withdrawl |
ABBA Alpha blockers (clonidine) Benzo's Barbiturates Alcohol |
|
|
Nicotinic stimulation effects |
Monday - mydriasis Tuesday - tachycardia Wednesday - weakness tHursday - hypertension Friday - fasciculations Saturday - seizures |
|
|
Oxygen toxicity symptoms |
VENTIAC V ertigo E uphoria N ausea T innitus I mpaired judgement A LOC (Altered LOC) C onvulsions |
|
|
Lake Louise criteria for AMS |
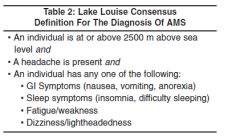
|
|
|
Lake Louise criteria for HACE |
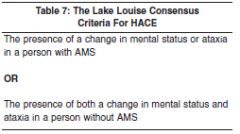
|
|
|
Lake Louise criteria for HAPE |
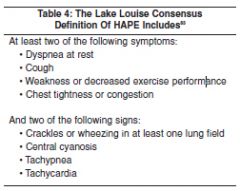
|
|
|
The TIMI Score |
2 or more episodes of angina in past 24h 7 days history of ASA use
C AD (known and >50%) A ge > 65 R isk factors (>3) T roponin S T changes |
|
|
Predictors of difficult BVM |
B eard O bstructed / O bese / O SA N eck stiffness / N eck mass E xpecting (pregnant) S tridor / S nores |
|
|
Predictors of difficult intubation |
L ook externally E valuate 3-3-2 M allampati O bstruction / O besity N eck mobility (decreased) |
|
|
Predictors of difficult cric |
S urgery H ematoma / H ave infection (abscess) O besity R adiation T rauma / T umor |
|
|
Predictors of difficult LMA |
R estricted mouth opening O bstruction D istored airway anatomy S tiff lungs / Neck |
|
|
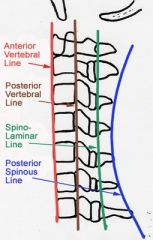
What are the lines of the cervical spine? |
|
|
|
How do you assess for pseudosubluxation in the pediatric C-spine? |

Swischuk's line (anterior arch of C1-C3 is within 2mm of C2)
|
|
|
Cervical spine fracture mechanisms |
All are flexion, except:
Vertical Compression - Burst & Jefferson
Extension - C1 neural arch, Hangman, Extension teardrop
Flexion-rotation - Unilateral facet, Rotary atlantoaxial |
|
|
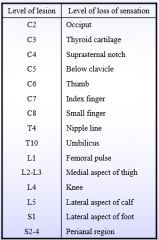
Sensory spinal levels |
|
|
|
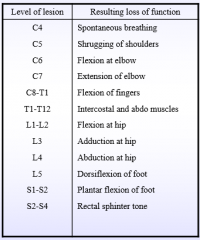
Motor spinal levels |
|
|
|
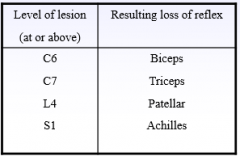
Reflex spinal levels |
|
|
|
Describe the motor deficit in central cord syndrome |
It is MUDdy!
Motor > sensory Upper > lower Distal > proximal |
|
|
Signs of aortic dissection on CXR |
Wide CHAPPLA1N
Wide mediastinum (8cm AP, 6cm PA, >25% chest width at aortic knob) C alcium sign H emothorax A ortic knob obscured P aratracheal stripe widened P leural cap L eft mainstem bronchus depressed A ortic window lost 1 st rib fracture N G deviates to the right along with trachea |
|
|
Occlusive and nonocclusive arterial injuries |
Occlusive -Transection -Thrombosis -Arterial spasm (reversible)
Nonocclusive -Intimal flap -Pseudoaneurysm -AVM -Compartment syndrome |
|
|
Diagnostic aid for a migraine |
Migraine is likely with two or more of the POUND criteria: -P ounding -hO urs lasts (4-72) -U nilateral -N ausea and vomiting -D ebilitating |
|
|
International Headache Society Migraine Definition |
1 --> 4 to 72 hours
2 --> At least two of the following: -Aggravation by or causing avoidance of routine physical activity -Moderate or severe pain intensity -Pulsating quality -Unilateral location
3 --> During headache, at least one of the following: -Nausea and/or vomiting -Photophobia and phonophobia
4 --> Not attributed to another disorder
5 --> History of at least five attacks fulfilling above criteria |
|
|
Causes of pancreatitis |
I GET SMASHED I diopathic
G allstones E thanol T umors (pancreas, ampula, choledochal)
S corpion stings M icro - Bacterial (Mycoplasma, Camylobacter, TB), Viral (Mumps, Coxsackie, Rubella, Varicella, CMV, hepatitis, EBV), Parasites (ascaris, echinococcus) A utoimmune (SLE, PAN, Crohn's) S urgery / trauma H yperlipidemia / H ypercalcemia (hyperparathyroid) E mboli / ischemia D rugs / toxins (azathioprine, estrogen, lasix, valproic acid, APAP, ASA, sulfonamides) |
|
|
Types/causes of diarrhea |
MMISO
M alabsorption (short gut, CF, IBD, celiac, lactose intolerant) M otility (DM, neuromuscular, scleroderma) I nflammatory - cellular damage causing secretion; can be hemorrhagic (enterohemorrhagic E Coli, Salmonella) or IBD, autoimmune, chemo S ecretory (Toxin-mediated chloride secretion: Enterotoxic E Coli, Shigella, Salmonella, Vibrio, C Diff; does not decrease with fasting) O smotic (altered gut flora from Noro or Rotavirus; ingestion of sorbitol or lactulose; decreases with fasting) |
|
|
Top 5 causes of occult irritability in children |
FAT SHIC
F racture A buse T esticular torsion
S urgical abdomen H air tourniquet I mproper feeding C orneal abrasion / C olic |
|
|
Dermatologic findings in pediatric seizures due to neurocutaneous disorders |
Cafe au lait - Neurofibromatosis Ash leave - Tuberous sclerosis Port au Wine Staine - Sturge-Weber |
|
|
Appearance assessment of the pediatric assessment triad |
TICLS Tone Interactivity Consolability Look/gaze Speech/cry |
|
|
Lateral soft tissue x-ray findings of epiglottitis |
AAA PBL on TV A ir fluid level A ryepiglottic fold swelling A rytenoid swelling
P revertebral tissue swelling B allooning of the hypopharynx L oss of L ordosis
T humbprint epiglottis V allecula obliteration |
|
|
Approach to the striderous child |
Supraglottic -Congenital (Micrognathia, Macroglossia, Choanal atresia) -Acquired (Retropharyngeal abscess, Epiglottitis) Glottic -Congenital (Laryngeal web, Vocal cord paralysis, Laryngeomalacia) -Acquired (Laryngeal papilloma) Subglottic -Congenital (Subglottic stenosis, Hemangioma) -Acquired (Croup, Subglottic stenosis) Tracheal -Congenital (Tracheomalacia, Tracheal stenosis, vascular ring) -Acquired (Bacterial tracheitis, Foreign body) |
|
|
Signs of retrobulbar hemorrhage and indications for lateral canthotomy |
DIP A CONE (DIP is primary indications; A CONE is secondary)
D ecreased VA I ncreased IOP (>40) P roptosis
A fferent pupillary defect
C herry red macula O pthalmoplegia N erve head pallor E ye pain |
|
|
Medical treatment of increased IOP |
ABCDPS A lpha 2 agonist (Apraclonidine 1% - decrease production and increase outflow) B eta blocker (Timolol 0.5% - decrease humor production) C holinergic (Pilocarpine 1% - constricts pupil and opens trabecular meshwork) D iuretic (Mannitol & Acetazolamide - decrease production) P rostaglandins (Latanoprost - increase outflow) S teroids (Prednisone acetate 1% - decrease inflammation) |
|
|
Indications for referral to opthalmology of an eyelid laceration |
The 5 L's
L id margin L acrimal system L evator or canthal tendons L oss of tissue L eaking of fat |
|
|
DDx for sudden visual loss |
Anatomic
Anterior chamber - hyphema, hypopiom, glaucoma Iris/lens - lens dislocation, iritis Posterior chamber - posterior vitreous detachment or hemorrhage Retina - Retinal detachment, central venous occlusion, central arterial occlusion Neuro-opthalmologic - pre-chiasm (optic neuritis due to ischemia/compression/toxin), chiasmal (tumor), post-chiasm (CVA, tumor, AVM, migraine), visual cortex (CVA) |
|
|
Kanavel signs of flexor tenosynovitis |
Fingers held in slight flexion Fusiform (symmetrical) swelling Pain to palpation of flexor tendon Pain on passive extension |
|
|
Hand motor testing |
Radial nerve - wrist extension (triceps) Posterior interosseous branch of the radial nerve - thumb extension
Median nerve - thumb opposition to fingers Anterior interosseous branch of the median nerve - OK sign
Ulnar nerve - Froment's paper sign; finger abduction and adduction |
|
|
Hand sensation testing |
Radial nerve - dorsal 1st web space Median nerve - volar tip of D2 Ulnar nerve - volar tip of D5 |
|
|
Back pain red flags |
Infectious - fever, IVDU Fracture - history of trauma Cancer - weight loss, history of cancer Cauda equina - urinary retention, fecal incontinence, saddle anesthesia
Nocturnal pain
|
|
|
Indications for lumbar spine x-rays |
M alignancy A ge (<18 or >50)
F ever I mmunocompromised N euro deficits (progressive) D uration (>4-6 weeks)
W eight loss I VDU T rauma |
|
|
Lines of the pelvis x-ray |

|
|
|
One pill can kill |
Alpha blocker (clonidine) Antihyperglycemic agents BB Barbiturates CCB Digoxin
MAO-I Methadone
Theophylline TCA
Methyl salicylate Toxic alcohol
Iron Camphor Lomotil |
|
|
Drugs that cause seizures |
WITH LA COPS W ithdrawal / Wellbutrin I NH T heophylline / TCA L ithium / L ocal anesthetics / L ead A nticholinergics C holinergics / C amphor O rganophosphates P CP S alicylates / Sympathomimetics |
|
|
Drugs MDAC is appropriate for |
Please Quit Drinking the AC Dummy Phenobarb Quinine Dapsone Theophylline / TCA (maybe) ASA Digoxin (maybe) / Dilantin (maybe) |
|
|
Dialyzable drugs |
BIT SLIME B arbiturates I soniazid T heophylline
S alicylates L ithium I ctogenic drugs (Tegetrol, Valproate, Phenobarb) M ethanol E thylene glycol D abigitran |
|
|
Indications for reduction of a distal radius fracture |
Step >1mm Radial inclination <15 degrees (normal 22) Volar tilt less than 0 degrees (normal 10-25) Decreased radial height (normal 11mm, loss of 2mm relative to other side is short) |
|
|
Clavicle fracture's requiring orthopedic consultation |
The rule of 2's >2 cm displacement 2 or more pieces <2cm from either end of the clavicle >2cm of shortening 2 good 2 be true |
|
|
Shoulder dislocation techniques |
Stimson - prone, arm hanging with weight x 20 minutes Traction-countertraction - sheet under arm for countertraction, abducted arm FARES - supine, slow abduction with flexion/extension until 90 degrees then external rotation Milch - supine at 45 degrees, external rotation and abduction to 90/90 then longitudinal traction Scapular manipulation - can be added to traction/countertraction and Stimson, rotate inferior tip medially Cunningham - seated, shoulders adducted, elbow flexed with shoulder on provider shoulder, massage of bicep at mid-humeral level |
|
|
Open fracture classification |
Gustillo classification system I - <1cm, clean, tx with 1st gen cephalosporin II - >1cm, minimal soft tissue damage, tx with 1st gen cephalosporin IIIa - significant soft tissue damage with adequate coverage, 1st gen cephalosporin and aminoglycoside (gentamicin) IIIb - significant soft tissue damage with INadequate coverage, same tx as IIIa IIIc - open # with vascular injury , same tx as IIIa
Add Pen G or Clinda if concern for anaerobes (farm injury) and Cipro if concern for salt water (pseudomonas)
|
|
|
Femoral nerve injury |
Motor - weak knee extension, can't climb stairs or get up from sitting Sensory - varies, most reliable superomedial to patella Reflex - decreased patellar |
|
|
Sciatic nerve injury |
Motor - paralysis of hamstring (knee flexion) and all muscles below the knee Sensory - posterior thigh and below the knee Reflex - decreased Achilles tendon |
|
|
Hip reduction techniques |
Allis - patient supine with hip and knee flexed to 90 degrees, get on bed and provide vertical upward traction while someone holds the pelvis to the bed. Works for posterior and anterior-obturator (femoral head seen over obturator foramen).
Stimson - patient prone with one leg hanging off of the bed, flex hip and knee to 90 degrees, vertical downward traction while someone holds the pelvis/pushes down on the femoral head.
Whistler - patient supine, arm under knee of dislocated hip with arm on opposite knee (both legs flexed at the hip/knee) to use opposite leg as a fulcrum. A modification of this is the Captain Morgan with your leg under the patient's knee instead of your hand. |
|
|
Kocher criteria to distinguish septic arthritis from transient synovitis |
With 0-4 criteria the likelihood is: 2%, 9.5%, 35%, 73%, 93% -Non weight bearing -ESR >40 -WBC >12 -Fever > 38.5 CRP >20 is also predictive |
|
|
Ottawa Knee Rule |
Get x-rays if: Age >55 Inability to transfer weight 4 times at time of injury OR in ED Inability to flex to 90 degrees Patellar tenderness Fibular head tenderness |
|
|
How do you assess for patella alta / baja? |
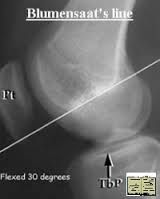
Blumensaat's line or Insall-Salvati ratio (patella length should be <0.8 of patellar tendon length; if not patella alta)
|
|
|
Ottawa Ankle Rule |
Applied to acute ankle injuries with malleolar pain (not hindfoot, forefoot, upper fibula) -Pain to posterior edge of the lateral malleolus from its distal part and 6cm proximal -Pain to the posterior edge of the medial malleolus from its distal part and 6cm proximal -Unable to weight bear 4 steps immediately after the injury and in the ED |
|
|
Ottawa Foot Rule |
-Pain over the navicular bone -Pain to the base of the 5th metatarsal -Unable to weight bear 4 steps immediately after the injury and in the ED |
|
|
How do you calculate Boehler's angle? |
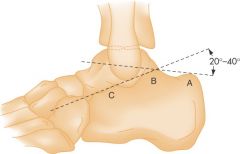
A = Posterior tuberosity B = Apex of posterior facet C = Apex of anterior process |
|
|
Bones at high risk of AVN |
-Head of femur (Legg-Calve-Perthes syndrome in children generally 4-10yo) -Scaphoid -Lunate (Kienbock's disease) -Talus -Navicular (Kohler's disease) -Second metatarsal |
|
|
DDx for non-accidental trauma in children (fractures and bruising) |
-Osteogenesis Imperfecta -Rickets -Scurvy -Menkes' Kinky Hair Syndrome -Hypervitaminosis A -Hypoparathyroidism -Congenital Syphilis -Pathologic fractures -Birth fractures
-Metaphyseal cupping & spurring (normal variant - bilateral, diaphyseal, smooth) -Periosteal new bone formation (normal variant - especially to the femur)
-Cultural practices (Cupping, Coining, Spooning) -Bleeding disorders (hemophilia, vWD, HSP) -Mongolian spots -Hemangioma -'Tattooing'
-ITP -HSP -Secondary syphilis |
|
|
Diagnostic criteria for staph toxic shock syndrome |
DR FrOH (NO culture needed) D esquamation of the skin (begins during recovery phase after 1-2 weeks; R ash (blanching, macular, erythematous, NOT itchy, fades before desquamation)
F ever (>38.9) r O rgan systems (>3/7 involved: CNS, mucous membranes, GI, renal, hepatic, heme, MSK) H ypotension (sBP < 90 or < 5th percentile in children) |
|
|
Diagnostic criteria for strep toxic shock syndrome |
You going to the strep SHO?
S erology (isolation from a sterile [definite] or nonsterile [non-definite] site) H ypotension (sBP<90 or <5th percentile) O rgan systems (>2/6 involved: Renal, Heme, Liver, Lung, Rash, Soft tissue necrosis) |
|
|
Determining capacity |
C ommunication U nderstanding R easoning V alues E mergency S urrogate |
|
|
When can implied consent be assumed |
-Patient is unable to express their preferences (CURV) -Immediate action is required (E) -No surrogate decision maker (S) |
|
|
Signs of Lithium toxicity |
SNAP MUD S eizures N /V/D A taxia P arkinsonian
M yoclonus U MN D elirium/D ecreased LOC |
|
|
Infections requiring airborne precautions |
Respiratory TB Varicella (chickenpox and disseminated zoster) Measles SARS +/- Ebola and TB (during aerosolizing procedures) |
|
|
AIDS-defining illnesses |
Heme -CD4<200
Malignancies -Kaposi's Sarcoma -Lymphoma -Cervical cancer (invasive)
Neuro -HIV-associated encephalopathy -Progressive multifocal leukoencephalopathy -Toxoplasmosis of brain
Fungal infection -Candida (esophageal or pulmonary) -Histoplasmosis -Cryptococcus -Coccidiomycosis
Protozoa infection -PJP pneumonia -Isosporiasis -Toxoplasma gondii -Cryptosporidium
Viral -HSV (persistent, pneumonia, esophagitis) -CMV (except spleen/liver/lymphatics)
Bacterial infection -Tuberculosis -Mycobacterium avium complex -Salmonella sepsis -Recurrent bacterial infections |
|
|
SIRS |
HR > 90 RR < 20 OR PaCO2 <32 T < 36 OR > 38 WBC <4 OR >12 OR >10% bands |
|
|
Definition of ARDS |
As per the 2012 Berlin Definition -Respiratory symptoms started or worsened acutely with the last week -PaCO2 / FiO2 ratio 200-300 = mild, 100-200 = moderate, <100 = severe -Bilateral pulmonary infiltrates (CXR or CT) -Not in cardiac failure / no fluid overload
|
|
|
Malaria: Organism, Vector, Incubation, Presentation, Complications, Diagnosis, Treatment |
-Organism: Plasmodium Falciparum is most dangerous (also Ovale, Vivax, Malariae) -Vector: Female anopheles mosquito -Incubation: 8-28 days -Presentation: Fever in the returning traveler, anemia, constitutional (weak, dizzy, N/V/D, lethargy, myalgia, arthralgia, CP, abd pain, SOB) -Complications: cerebral/seizures, ARDS, ARI, DIC, anemia, acidosis, hypoglycemia -Diagnosis: Thin and thick peripheral blood smears q8-12h x 3d -Treatment: Chloroquine if sensitive; otherwise quinine & doxycycline |
|
|
Lyme disease: Organism, Vector, Incubation, Presentation, Diagnosis, Complications, Treatment |
-Organism: Borrelia Borgdorferi (spirochete) -Vector: Ixodes Tick -Incubation: Tick must attach long enough to become engorged (>48 hours) -Presentation: 1st stage erythema migrans & flu-like symptoms/HA; 2nd stage 4 weeks later with fluctuating meningoencephalitis/bilat Bells palsy, conduction block/pericarditis, arthritis, eye inflammation; 3rd stage lasting >1y with fatigue syndrome and arthritis -Diagnosis: Tick bite, IgM+ from 3-6 weeks, IgG+ >1 month (send both) -Complications: Can get Jarisch-Herxheimer reaction when tx started -Treatment: prophylax within 72h in endemic areas if adult tick on for >36h - use Doxy 200mg x1; treat with Doxy 200mg BID x 28d |
|
|
Rocky-Mountain Spotted Fever: Organism, Vector, Incubation, Presentation, Diagnosis, Complications, Treatment |
-Organism: Rickettsia Rickettsii -Vector: Rocky Mountain Wood Tick -Presentation: Sudden onset fever followed by N/V/abd pain/HA. Gets into vessels and releases tPA & vWF causing microthrombi and vascular permeability. Petechiae develop on wrists/hands then spread inward. Also cardiac (AVB, myocarditis), pulmonary (ARDS), neurologic (meningismis, transient deficits due to microinfarcts), renal (microinfarcts), heme (DIC). -Diagnosis: Serology not positive for 1/52 but req'd for conclusive Dx. Skin bx at 4-10 days. -Complications: Death due to renal failure then ARDS/DIC in 25% if not treated -Treatment: Doxycycline |
|
|
Things that shift the oxygen-hemoglobin dissociation curve |
CADETS turn right and fall down (right shift and decreased oxygen affinity) C - CO2 A - Acid D - 2,3 DPG E - Exercise T - Temperature S - Sickled Hb S |
|
|
Diagnostic criteria for delerium |
4 criteria: -Inability to focus/Inattention -Fluctuating course -Cognitive deficit (memory, disorientation, language) or perceptual disturbance not caused by dementia -Evidence that it is caused by a medical condition, ingestion, or withdrawl |
|
|
Diagnostic criteria for dementia |
1 - Memory impairment AND 2 - One of aphasia, apraxia, agnosia, impairment in executive functioning -Causing significant impairment -NOT due to delerium |
|
|
Treatment of active TB |
RIPE (side effects) x 9 months! R ifampin (orange body fluid) I soniazid (INH injures nerves and hepatocytes) P yrazinomide E thambutol (E=eyes - optic neuritis; can't distinguish red/green) |
|
|
Treatment for hyperkalemia |
C BIG K Drop
C alcium
B eta agonist / B icarbonate I nsulin G lucose
K ayexalate
D iuretics (Furosemide) R - R enal dialysis o p |
|
|
GBS: Cause, Presentation, Diagnosis, Complications, Treatment |
Cause: idiopathic, often secondary to Campylobacter, Mycoplasma, CMV or EBV - results in antibodies to nerves
Presentation: progressive ascending symmetric weakness and areflexia; Miller-Fischer variant starts centrally (areflexia, ataxia, opthalmoplegia with III/IV/VI affected). Also has autonomic dysfunction (tx brady with atropine; use short acting for hypertension, fluids for hypotension)
Diagnosis: CSF elevated protein, normal glucose and WBC
Complications: respiratory compromise req'ing intubation if FVC <20ml/kg or NIF <30mL/kg
Treatment: IVIg or plasmaphoresis |
|
|
Myasthenia Gravis: Cause, Presentation, Diagnosis, Complications, Treatment |
Cause: Antibodies to post-synaptic ACh receptors (take spots & destroy them)
Presentation: Ptosis, Diplopia, Dysarthria, Dysphagia, Blurred vision with spared pupils, resp failure. Treated patients can present with cholinergic crisis.
Diagnosis: Tensilon test, ice to eyes, NIF (<15 intubate)/FVC (<15 intubate); check for anti-AChR antibodies
Treatment: Plasma exchange or IVIg (neostigmine and/or thymectomy for chronic); intubate with cisatracurium (Hoffman degradation) |
|
|
DDx of bulbar neuropathy |
-Myasthenia gravis -Lambert-Eaton myasthenic syndrome -ALS -Miller-Fisher variant GBS -Elapidae (coral snake) or Hydraphidae (sea snake) envenomation -Botulism -Lyme disease -Organophosphate poisoning -Congenital syndrome -Penicillamine toxicity |
|
|
How can Tick Paralysis and GBS be distinguished? |
-Both generally ascending paralysis -Finding/not finding an Ixodes tick attached -Tick paralysis has pupillary dilation while GBS does not |
|
|
Gram stain results of bacteria |
Staph: Gram+ cocci in singles, doubles, tetrads or clusters Strep: Gram+ paired diplococci (other strep in pairs/chains) Listeria: Gram+ single or chains Moraxella caterrhalis: Gram- diplococci Neisseria: Gram- paired diplococci H Flu: Gram- coccobacilli E Coli: Gram- rods Pseudomonas: Gram- rods |
|
|
Angina Classification |
Canadian Cardiovascular Society I - No limitation of ordinary activity II - Mild limitation. Symptoms at >1-2 blocks or >1 flight of stairs. III - Moderate limitation. Symptoms at <1-2 blocks or <1 flight of stairs. IV - Severe limitation. Symptoms at rest. |
|
|
Definition of stable angina |
Predictable Transient (<15m) Reproducible with activity Relieved with rest/nitro |
|
|
Definition of acute MI |
-Rise and fall of troponin with: ischemic symptoms, Q waves, ST/T changes, coronary artery intervention -Pathological evidence |
|
|
Types of myocardial infarction |
I - ischemia due to a primary coronary event (plaque rupture or dissection) II - supply-demand ischemia III - sudden cardiac death with symptoms of MI IV - MI with coronary instrumentation V - MI with CABG |
|
|
At risk for an atypical presentation of MI |
Aunt Jemima with dementia -Elderly -Diabetic (from all the syrup) -Non-white -Female -Dementia -Hyperlipidemia (from all the sausages)
Also: No prior history of MI, history of stroke, /CHF, no family history |
|
|
Liver transplant criteria in acetaminophen-induced and non-acetaminophen-induced fulminant hepatic failure (King's College criteria) |
Acetaminophen induced pH <7.3 or lactate >3 after 12h of resuscitation Lactate >3.5 after 4h of resuscitation
OR all 3 of: -Cr >300 -INR >6.5 -Grade 3-4 hepatic encephalopathy
Non-acetaminophen induced INR >6.5
OR 3/5 of: J aundice >1 week prior to encephalopathy A ge <10 or >40 N on-A non-B hepatitis E tiology: indeterminate or drug reaction B ilirubin >300mmol/L I NR >3.5 |
|
|
Sgarbossa Criteria |
In setting of LBBB, the criteria for calling AMI is >3 points: >1mm concordant STE (OR 25, 5 points) >1mm STD in v1, v2, v3 (OR 6, 3 points) >5mm discordant STE (OR 4.3, 2 points)
Also look at ST (baseline to T) / S (top of S to baseline) ratio <-0.25
|
|
|
Classification of AMI severity |
Killip classes 1 no failure 2 crackles, S3, elevated JVP 3 frank pulmonary edema 4 cardiogenic shock, hypotension, vasoconstriction (oligurea & cyanosis) |
|
|
What are the target times for ACS? |
Door Data (10m) Decision Drug (lytic 30m, PCI 90m in center) |
|
|
What is the Ashman phenomenom? |
-Seen in supraventricular tachyarrhythmias (generally AFib) -Long R-R interval (has long refractory period) followed by a short R-R interval results in part of the right bundle being refractory -Get a RBBB waveform that looks like a PVC |
|
|
Mechanisms for arrhythmias |
-Increased automaticity (ischemia, electrolytes, drugs) -Reentry (req's 2 conduction pathways with different responsiveness and conduction speed) -Triggered (early afterpolarizations in brady/long QTc; treat by increasing HR vs late afterpolarizations in tachy/increased Ca; treat by slowing HR and decreasing Ca) |
|
|
Antiarrhythmic types/actions |
Some Buggers Kill Cats
S odium channel blocker (a block fast, b block inactivated phase, c block both) - procainamide/TCA/cocaine, lidocaine/phenytoin, flecainide/dilantin B eta blocker - propranolol/esmolol K potassium channel blocker - amiodarone/sotalol C alcium channel blocker (slow) - verapamil/diltiazam |
|
|
How does Digoxin work? |
1 - Blocks Na/K ATPase leading to increased intracellular Ca++ (increased inotropy, tachyarrhythmias) 2 - Increases vagal tone (anti-arrhythmic, bradyarrhythmias) |
|
|
Non-compensatory pause vs compensatory pause |
Non-compensatory pause: sinus node is reset and beat following the aberrant beat occurs at the same R-R interval as it would have if it came after a regular beat.
Compensatory pause: sinus node is NOT reset. One sinus beat is not conducted (meets refractory AVN) and the next is. The next beat comes after exactly 2x the standard R-R interval. |
|
|
DDx for irregular SVT |
-AFib -MAT -Atrial flutter/tachy with variable conduction -Parasystole -Extrasystoles |
|
|
Contraindications to ED Cardioversion of AFib |
1 - Lasted > 48 hours 2 - Rheumatic heart disease 3 - Mechanical valve 4 - History of stroke/TIA |
|
|
Risk stratification for AFib - who needs anticoagulation? |
CHADS2 C HF H ypertension A ge > 75 D iabetes S troke before (worth 2 points)
0 = ASA; 1 = ASA or anticoagulant (anticoagulant preferred); 2 = anticoagulant |
|
|
Strong predictors of VT in a rapid wide-complex tachycardia |
-AV Dissociation -Fusion beats -Capture beats -QRS >0.14 -Extreme left axis
Brugada and Griffith criteria are too unreliable for use and likely cause harm |
|
|
Congenital vs Adult Torsades |
Congenital: precipitated by tachycardia, catacholamine excess, and delayed afterpolarization, treat with beta blockers, associated with Romano-Ward syndrome and Jervall & Lange Nielson syndrome
Adult: precipitated by bradycardia, early afterpolarization, treat with beta agonists, associated with drugs |
|
|
Drugs that prolong QT |
Antidysrhythmics Ia, Ic, III: procainamide, propafenone, amiodarone Antibiotics: azithromycin, ciprofloxacin Antipsychotics: haloperidol Antiemetics: ondansetron, metoclopramide Anticonvulsants: Antihistamines: Antifungals: Antimalarials: chloroquine Antidepressants: TCA, citalopram Analgesia: Methadone
Also, hypoCa, hypoMg, hypoK |
|
|
Effect and indications for use of a magnet on a pacemaker |
Changes a standard pacemaker to VOO mode and turns off defibrillation in an ICD/pacemaker
-Atrial tachycardia with rapid ventricular rate -Runaway pacemaker (re-entry tachycardia) -Bradycardia due to oversensing |
|
|
Causes of ICD malfunction |
Frequent shocks -Shocking SVT -Oversensing T waves -Having frequent VF/VT (hypoK, hypoMg, Ischemia, drug-induced)
Inadequate shocks (dizzy/syncope) -Undersensing VT -Shocks not strong enough -Inadequate backup pacing for brady
Cardiac arrest -Likely VF did not respond to defibrillation -May have not detected VF (change parameters) |
|
|
Anemia differential approach |
Decreased production -Lack of stimulation (renal disease, chronic disease) -Unfunctional marrow (infiltrative disease: amyloid, metastasis; marrow disorders: aplastic, myelofibrosis; blood cancers: lymphoma, leukemia; tox: heavy metals, clozapine) -Lack components (B12, Folate, Fe)
Increased destruction -Intravascular (mechanical: prosthetics and microangiopathic DIC/TTP; transfusion reaction: ABO, antibodies; defects: G6PD, sickling) -Extravascular (abnormal RBC: spherocytosis, thalassemia) |
|
|
Causes of sideroblastic anemia |
Impaired production of porphoryn; leads to anemia and excess Fe in RBC's (Fe ring in sideroblasts)
-Toxins: Lead, Alcohol & INH -Premalignant condition in elderly (often get AML) -Malignancy -RA -Pyridoxime deficiency |
|
|
Paroxysmal nocturnal hemglobinuria |
Definition - Stem cell defect with abnormal sensitivity of RBCs, neutrophils and platelets to complement Diagnosis - Get hemosiderinurea, low RBC/Plt/Neutrophils, chronic hemolysis -Luekocyte alkanine phosphatase levels are elevated -Complications: thrombosis of arteries and hepatic vein. Also MUST transfuse with WASHED RBC's or compliment on them will lead to lysis. |
|
|
Encapsulated bacteria |
SSome Nasty Killers Have Capsular Protection
S trep pneumoniae S almonella typhi N eisseria meningitidis K lebsiella pneumoniae H aemophilus influenzae C ryptococcus neoformans P seudomonas aeruginosa
|
|
|
Equipment required for a neonatal resuscitation |
Be prepared for baby WOBLIS
W armer / polyethylene bag - all babies O xygen (blended) - for persistent hypoxia B ag and mask - if HR<100, gasping, apnea give 40-60 bpm with PPV L aryngoscope and ETT - for meconium suctioning, ineffective/prolonged BVM, chest compressions I ncubator for transport S uction |
|
|
Does the baby need resuscitation? |
Term? Breathing or crying? Muscle tone?
If yes, no resuscitation needed |
|
|
Neonatal CPR |
CPR is indicated if the infant's HR is <60bpm despite 30s of adequate PPV.
Chest compression rate is 90/minute Breathing rate is 30/minute (q 3 chest compressions) Epinephrine is used if HR <60bpm after 30s of CPR (dose 0.1-0.3mL/kg of 1:10,000 epi IV) |
|
|
When should an infant not be resuscitated? |
-<23 weeks -<400g birth weight -Anencephaly -Known chromosomal abnormalities incompatible with life (trisomy 13 or 18) -Stop resuscitation at 10m if there has been no HR or respiratory effort |
|
|
Causes of ascending paralysis |
Goes BOTTOM VP
G BS
B uckthorn / B-virus (Herpes Simiae) O rganophosphate T ick paralysis T oxic neuropathies (DM, EtOH, B-vitamin deficiencies, Buckthorn) M etabolic (hyperkalemic periodic paralysis)
V iral (Rabies, CNS VZV/CMV, West Nile) P olio |
|
|
Causes of hemolytic anemia (low haptoglobin, high LDH) |
Intrinsic: -Enzymes (Pyruvate Kinase or G6PD) -Membrane (Spherocytosis, Elliptocytosis, PNH) -Heme (Thallasemia, Sickle Cell)
Extrinsic -Mechanical (Microangiopathic - DIC/TTP/HUS/Vasculitis/Preeclampsia) -Other (valves, march) -Immunologic --> Alloimmune (ABO IgM intravasc / Rh IgG extravasc) --> Autoimmune (Reticular neoplasms [CML, CLL, lymphoma, myeloma], Inflammatory (SLE/RA/PAN/UC), Drugs (quinine, quinidine, methyldopa, PCN/cephalosporins, sulfa), Infectious (CMV/EBV/Mycoplasma/Coxsackie/Hepatitis), Thyroid,
Environmental (hyperthermia, brown recluse bites, freshwater drowning, burns, snakes, malaria)
Abnormal sequestration (hypersplenism) |
|
|
Pentad of TTP |
CRAFTY
C NS changes (fluctuating seizures, paresthesias, altered LOC) R enal failure (ARI, hematuria, proteinuria) A nemia (microangiopathic hemolytic with schistocytes) F ever T hrombocytopenia (Plts 10-50) |
|
|
Erythema nodosum |
BELTY SLIPS B ehcets E strogen L ofgran's T B Y = V iral (#2)
S trep (#1) L ymphoma (NHL) and Leukemia I BD P CN S ulpha |
|
|
Define and give a DDx for ALTE |
ALTE is an acute, unexpected change in an infant's breathing (apnea or gagging), appearance (color change), or behavior (loss of muscle tone) that frightens the observer. Prevalence peaks at 10-12 weeks but can occur in children <1yo.
-Neuro - Seizures/Hydrocephalus -Cardiac - Arrhythmia, Congenital heart disease -Respiratory tract infection (Pertussis, RSV) -GI - GERD (Sandifer syndrome) -Metabolic - Hypoglycemia, inborn errors of metabolism, hyponatremia -Sepsis - pneumonia, UTI -Heme - anemia -NAT -Factitious illness -Toxins |
|
|
HUS vs TTP vs DIC |
HUS -Caused by Shiga toxin of O157:H7 -Renal symptoms predominate -Consumptive (elevated DDimer decreased haptoglobin but normal LDH) -Children with bloody diarrhea -Plasmapheresis ineffective
TTP -Caused by lack of ADAMTS13 (? autoimmune) not cleaving vWF precursor -Neuro symptoms predominate -Adults -Non-consumptive (normal DDimer/Haptoglobin/fibrinogen but elevated LDH) -Schistocytes -Treat with plasmaphoresis or plasma exchange
DIC -Consumptive: low fibrinogin and fibrin levels; high DDimer -Bleeding and clotting at the same time; ultimately bleed when factors gone -Schistocytes, anemia, thrombocytopenia -Caused by multiple underlying disorders |
|
|
Treatment options in patients with vWD |
1 - Tranexamic acid or Aminocaproic acid (plasmin inhibitors - 5g po/iv) 2 - DDAVP (releases vWF and F8 from endothelium - 0.3mcg/kg SC/IV or 1.5mg nasal spray x 2) 3 - Humate-P F8 concentrate (need to ensure it has enough vWF) 4 - Cryoprecipitate (not recommended due to potential for viral transmission) |
|
|
Describe how factors should be replaced in Hemophilia A and B |
Can empirically use 15-20mL/kg FFP (40mL/kg replaces 100% of all factors). -Cryo contains F8. DDAVP releases F8 -Cryo-poor plasma contains F9. -aF7 bypasses both
Generally use F8 & F9 concentrate, respectively. Give 0.5IU/kg/% activity needed for F8 Give 1IU/kg/% activity needed for F9
INITIAL goals: Mild ~30%, Moderate ~50%, Life-threatening >90%; repeat dosing needed for F8 (q8-12h) and F9 (q18-24h) -Minor bruising/lacerations - 40% -Dental work /severe epistaxis/renal/deep lac - 50% -Deep muscle (e.g. iliopsoas)/CNS/Throat/GI/major surgery - 80-100% |
|
|
Bleeding reversal agents for Aspirin, Clopidogrel, Ticegralor, Warfarin, UFH, LMWH, Dabigatran, Rivaroxaban, Apixaban, t-PA/lytic |
Aspirin: DDAVP for minor, platelets for major
Clopidogrel/Ticegralor: DDAVP for minor, platelets for major
Warfarin: Depends. Hold if not bleeding. Hold + vit K po if have time. Hold + vit K IV + FFP (15mL/kg or 2-4U) OR PCC 50IU/kg
UFH: Protamine sulfate 1mg per 100U
LMWH: Protamine sulfate 1mg per 1mg
Dabigatran: PCC 50IU/kg, try FEIBA, vitamin K, Tranexamic acid (1g IV), dialysis (only 33% protein bound); send TT (thrombin time to confirm cause)
Rivaroxaban/Apixaban: PCC 50IU/kg; try tranexamic acid (1g IV), NO dialysis; send anti-Xa level to confirm cause
t-PA/thrombolytic: FFP 2U q6h x 4; Cryoprecipitate x 10U; Tranexamic Acid 1g; Platelets 1 adult; DDAVP 0.3mcg/kg IV; Protamine to reverse any heparin; treat ICP; be prepared to treat seizures |
|
|
Causes of heart failure |
HEART FAILED H ypertension E ndocarditis / E nvironment (heat wave A nemia R heumatic heart disease T hyrotoxicosis
F ailure to take meds A rrhythmia I nfection / I schemia / I nfarction L ung (COPD, PE, Pneumonia) E ndocrine (Pheochromocytoma / Hyperaldosteronism) D ietary indiscretions (salt / fluid) |
|
|
Heart failure classes |
NYHA Functional classes for CHF I - Asymptomatic with ordinary physical activity II - Symptomatic with ordinary physical activity III - Symptomatic with less than ordinary physical activity IV - Symptomatic at rest |
|
|
Organisms responsible for endocarditis |
Staph aureus (especially in right sided / IVDU) Strep viridans Strep bovis (association with GI malignancies) Enterococcus (add vanco and watch for resistance)
HACEK - haemophilus atrophilus, actinobacilus, cardiobacterium hominus, eikenella corrdons, kingella kingae (often chronic IE, hard to culture)
Immunocompromised fungal - Candida/Aspirgillus |
|
|
ECG changes of pericarditis and how are they different than MI |
1 - PR depression and diffuse STE (hours to days) 2 - Normalization of ST segments and flattening of T waves 3 - Deep, symmetrical T wave inversion 4 - ECG reverts to normal (sometimes T waves remain inverted)
Different than MI: non-anatomic pattern, concave up, no Q waves, no dynamic worsening |
|
|
Distinguishing murmur of AS vs HOCM |
AS is more likely to have insufficiency on top of other findings.
Valsalva (increased intrathoracic pressure decreases pre and afterload) - HCM louder and AS quieter
Squat (increased SVR increases pre and afterload) - HCM quieter and AS louder |
|
|
Prognostic factors for pancreatitis |
Ranson criteria (on admission) - mortality for 1-2 = 1%; 3-4 = 15%; 5 = 50%
Non-gallstone / Gallstone A GALL A ge >55yo / >70yo
G lucose >11 / >12 A ST >250 / >250 L DH >350 / >400 L eukocytes >16 / >18
BISAP score
Urea > 8.92 Impaired mental status >2 SIRS criteria Age >60 Pleural effusion |
|
|
Transfer to a burn center |
-Partial thickness burn 10% BSA (2nd degree) -Any 3rd degree burn -Burns to face, hands, feet, genitalia, perinium, joints -Electrical burn (including lightning) -Chemical burn -Inhalational burn -Pre-existing medical conditions that complicate management -Children at a location that can not care for children -Cocomitent burn and trauma where the burn is the greatest danger -Burn injury in patients requiring social, emotional, rehabilitative intervention |
|
|
Dive injuries |
On descent -Ear barotrauma (inner, middle, external) -Mask squeeze (facial barotrauma) -Sinus barotrauma
At depth -Oxygen toxicity -Contaminated gases -Hypothermia -Nitrogen narcosis
On ascent -Alternobaric vertigo -AGE -Pneumothorax/ Pneumomediastinum/ Pulmonary hemorrhage -GI barotrauma -Barodontalgia |
|
|
Dive injuries requiring a recompression chamber |
-AGE -DCS I and II -Contaminated gases (CO) |
|
|
Arterial embolism vs thrombosis |
Embolism -Source of emboli -Sharp demarcation (no collaterals)
Thrombosis -History of claudication -Contralateral findings of partial occlusion -Diffuse atherosclerosis (lots of collaterals) |
|
|
Causes of CVL obstruction |
Complete -Clots -Precipitant -Mechanical obstruction
Withdrawl -Against vessel wall -Vein thrombosis -Fibrin sheath -Ball-valve thrombus
Intermittent -Pinching between clavicle and 1st rib |
|
|
Well's DVT Criteria |
DImPLES and the 3 C's (-2 points if an alternative diagnosis is as likely) - Likely if 2 or more
D VT previously I mmobilization (paralysis, plaster) P ain (along deep venous system) L eg swelling (entire leg) P itting edema (to only the affected leg) S urgery (last 3m)
C ancer (palliative or treated in past 6m) C alf swelling (>3cm circumference difference C ollateral veins (visible and nonvaricose) |
|
|
Well's PE Criteria |
Likely if 4 or more
D VT signs and symptoms A lternative less likely M alignancy P revious P E/DVT H emoptysis I mmobilization hR > 100 |
|
|
Contraindications for fibrinolytic in STEMI and PE |
1-Dissection?
Stroke 2-Prior ICH? 3-Ischemic stroke in last 3m?
Bleed 4-Known vascular lesion? (AVM) 5-Known intracelebral neoplasm? 6-Significant head/facial trauma in last 3m?
Can't Clot 7-Active bleeding 8-Bleeding diatheses? |
|
|
Gas laws (Pascal, Boyle, Charles, Dalton, Henry) |
Pascal - Pressure on a fluid is transmitted equally throughout Boyle - P1V2 = P2V2 Charles - V1/T1 = V2/T2 Dalton - Pt = P1 + P2 + P3 ... Henry - The amount of gas dissolved in a liquid (solubility) is proportional to the partial pressure of that gas above the liquid |
|
|
Reasons to modify the dose of adenosine |
-Patient weight (obese, pediatrics), need more or less -Heart transplant (don't use it) -Methylxanthines (theophylline) stimulates receptors, need more -Carbamezapine, needs less -Dipyradamole prevents breakdown, needs less -CVL delivery, need less |
|
|
Causes of priapism |
Medical conditions -Sickle cell -Leukemia -Spinal cord injury -G6PD deficiency -Thalassemia
Medications -ED - papaverine and PGE-1 -Phosphodiesterase inhibitors - sildenafil -Antipsychotics - chlorpromazine, clozapine -Antidepressants - SSRI's - trazodone -HTN - HCTZ -Mood/convulsant - Valproic acid -Recreational - alcohol, cocaine, amphetamines, heroin |
|
|
Toxic levels: ASA, APAP, Iron, Digoxin, Lithium, Methanol, Ethylene Glycol, TCA |
ASA Dose: 200mg/kg dose Level: Acute >7mmol/L; Chronic >3.5mmol/L
APAP Dose: 200mg/kg/24h dose; >150mg/kg/d for 48h; >100mg/kg/d for 72h Level: >1000mmol/L
Iron Dose: 20-40mg/kg (mild); 40-60mg/kg (mod); >60mg/kg (severe) Level: >90mmol/L
Digoxin Dose: 0.1mg/kg Level: >19mmol/L acute; >12mmol/L chronic
Lithium Level: >4mmoL/L acute; >2.5mmoL/L chronic
Methanol Dose: 0.15mL/kg Level: >6mmol/L toxic; >15mmol/L HD
Ethylene Glycol Dose: 0.2mL/kg Level: >3mmol/L toxic; >8mmol/L HD
TCA Dose: >5mg/kg |
|
|
Contrast Dilated, Hypertrophic, Restrictive, Takotsubo, Peripartum Cardiomyopathies (cause, treatment) |
Dilated: Mostly idiopathic but caused by ethanol, smoking, HTN, pregnancy, infection (myocarditis). Treated with pre and afterload reduction (ACEi, diuretics, PPV)
Hypertrophic: Caused by HOCM, AS, CAD, HTN. Treated with afterload reduction (BB). Must maintain preload!
Restrictive: Caused by amyloidosis, sarcoidosis, hemochromatosis, scleroderma, radiation, glycoven-storage diseases (Fabry/Gaucher). Treat underlying cause. Optimize preload (fluids).
Takotsubo: Caused by ? stress hormones. Treat as MI (indistinguishable from anterior STEMI) then BB and ACEi until recovery.
Peripartum: Caused by pregnancy (3 months before delivery to 6 months after). Treat afterload (hydralazine/labetolol until delivery, ACEi/BB after), preload (nitro), and contractility (digoxin) until recovery. |
|
|
Arteriosclerosis obliterans vs Thromboangiitis obliterans |
Arteriosclerosis: blue toe syndrome, claudication, ischemic rest pain in an elderly (>50) vasculopath (DM, smoker, HTN, cholesterol). Requires intervention if they have pain at rest. Can have distal ulcers.
Thromboangiitis: aka Buerger's disease, get painful erythematous nodules and decreased pulse in peripheral arteries. Only most commonly in male smokers 20-40yo and cure is stopping smoking completely. |
|
|
Distinguish vasogenic skin ulcers |
Arterial - distal to ankle, shiny, hairless, unswollen skin and thick nails. Less painful when dependent.
Venous - proximal to ankle, ++ swelling, weaping. Less painful when elevated.
Neurotrophic - sites of repeated trauma that they don't feel. Heels, toes, plantar surface. Not painful.
Hypertensive - on lateral malleolus, hemorrhagic bleb becomes an ulcer. Very painful. |
|
|
Vascular complications of IV drug use |
AV fistula and pseudoaneurysms (from 'hitting pink')
Unilateral hand edema (obliteration of superficial venous circulation)
Distal ischemia (severe burning pain distal to injections; possibly FB, talc, precipitate - nothing works to fix it; can need amputation)
Infected pseudoaneurysm (infected mass after hitting artery, reason that we assess abcesses for pulsatility) |
|
|
Extensive ileofemoral DVT: Names and diagnosis |
Phlegmasia Cerulia Dolens - swollen, congested, painful, cyanotic leg due to iliofemoral occlusion. Treat with thrombectomy.
Phlegmasia Alba Dolens - painful white leg secondary to arterial spasm that results from iliofemoral occlusion. Looks like arterial occlusion. Worse then cerulia. Treat with thrombectomy. |
|
|
APGAR Score |
A ppearance (pink, acrocyanosis, cyanosis) P ulse (>100, <100, absent) G rimace (sneeze/cough/pull away, grimace, no response) A ctivity (active, arms/legs flexed, limp) R espirations (good crying, weak cry, absent) |
|
|
Diagnosis and management of oncologic emergencies: febrile neutropenia, SVC syndrome, Tumor lysis syndrome, Hyperviscosity syndrome, Hypercalcemia |
Febrile neutropenia: Temp >38.3 (x1) or 38.0 (x1h) with ANC<1 or expected <0.5 (biggest drop 5-10 days post chemo). NO rectal temps. Treat with Tazocin x 14d if stable + vanco/gent if not stable.
SVC syndrome: Present with periorbital edema, plethora, facial swelling, arm swelling, dyspnea. Diagnose with CT. Treat with radiation/chemo or stent (stent best).
Tumor lysis syndrome: See hyperkalemia, hyperphosphatemia, hyperuricemia, hypocalcemia. Treat with IVF +/- urinary alkalinization if acidic +/- dialysis. Can also try rasburicase with consultations. Allopurinol can prevent but not treat.
Hyperviscosity syndrome: Lab can't run tests. Happens with MM, Waldenstrom's Macroglobulinemia, Leukemia. Present with CNS/vision changes. Treat with exchange transfusion, plasma/leukopheresis.
Hypercalcemia: Due to mets or parthyroid-like hormone. Treat with hydration, furosemide, bisphosphonates, calcitonin. |
|
|
Indications for dialysis in tumor lysis syndrome |
Phosphate >3.2 Potassium >6 Uric acid >590 Creatinine >880 Volume overload Symptomatic hypocalcemia |
|
|
Synovial fluid interpretation (Color, Viscosity, WBC/mm3, Differential, Culture) |

|
|
|
Special tests for the shoulder (Jobe, Drop arm, Neer's, Hawkin's, Painful arc, Lift off, Lift off lag, Yergason's, Speed's) |
Supraspinatus Jobe's: 90 degrees abd, 30 degrees anterior to coronal plane, internally rotated/pronated - weakness or pain = supraspinatus involvement. Drop arm test: passive abduction to 90 degrees. If can't be maintained, possible large supraspinatus tear.
Supraspinatus/Impingement Neer's: Hand stabilizing scapula, passive flexion to 180 degrees. Pain towards 180 degrees indicates impingement. Hawkin's: imagine a hawk being held on an arm (90-90 flexion at shoulder/elbow) then internally rotate and see if there is pain. Indicates impingement.
Subacromial bursitis Painful arc: Abduction with pain from 70-100 degrees indicates subacromial bursitis.
Subscapularis Lift off test: assess for tear by putting internally rotated hand on back, holding elbow, and getting patient to lift off. Lift off lag: assess for rupture by doing same but passively lifting off and seeing if patient can maintain.
Biceps Yergason's sign: Flex elbow to 90 and have patient try to supinate against resistance. Pain is positive. Speed's test: Extend elbow and supinate forearm. Flex shoulder against resistance. Pain is positive.
|
|
|
Types of hypersensitivity reactions |
ACID I A naphylaxis - IgE-mediated degranulation of mast cells and basophils II C ytotoxic - IgG mediated complex fixation III I mmune complex - IgG or IgM antigen-antibody complex deposition IV D elayed - T cell mediated |
|
|
Causes of cavitating lesions |
CAVITY C ancer (metastasis) A utoimmune (Wegener's granulomatosis, Rheumatoid Arthritis) V ascular (emboli, infarction) I nfection (TB, MRSA, SA, Klebsiella, Fungal) T rauma (pneumatocele) Y outh (congenital things; bronchogenic cyst)
|
|
|
Treatment of common Tinea (capitis/barbae, kereon, versicolour, unguinum, pedis, other) |
Tinea capitis/barbae: Itraconazole 250mg po od x 4/52; Selenium Sulphide shampoo 2x weekly
Kerion: As per tinea, plus Keflex 500mg po qid (if infected) and Prednisone 1mg/kg/d x 1/52
Tinea versicolour (Malassezia Furfur): Selenium Suphide shampoo (q monthly for prophylaxis) +/- Fluconazole 400mg po x 1
Tinea unguinum: Penlac (antifungal painted on nail) trial; Ketoconazole 200mg po od x 6 months +/- surgical nail removal
Tinea pedis: Clotrimazole 1% bid x 6 weeks
Tinea (other areas): Clotrimazole 1% bid x 3 weeks |
|
|
Treatment of candidiasis (Thrush, Cutaneous, Vulvovaginal) |
Thrush: Adults Nystatin (100,000U/kg) swish and spit 5mL po qid until resolved x 1/52. Infants the same but 'paint the mouth' qid x 7 days. Fluconazole if immunocompromised.
Cutaneous: Dry regularly, zinc oxide prn, 1% hydrocortisone prn, Nystatin (100,000U/kg) cream bid-qid OR Clotrimazole 1% qid x 6/52. Can also use Fluconazole 100mg od x 2/52.
Vulvovaginal: Clotrimazole intravaginal OTC. Can also use Fluconazole 150mg po x 1. |
|
|
Indications for emergent decompression of a subdural hematoma |
-Midline shift >5mm ->1cm thick -GCS decreased by 2 or more since the time of the injury -Fixed dilated pupils -ICP >20mmHg |
|
|
Define SIDS, apnea, pathological apnea, apnea of infancy, apnea of prematurity, periodic breathing |
SIDS: sudden infant death in a child without historical, physical, laboratory, or postmortem findings that explain the death. Peaks at 3-5 months (90% <6 months)
Apnea: cessation of air flow (central, obstructive, mixed)
Pathologic apnea: apnea lasting >20s with bradycardia, cyanosis, hypotonia
Apnea of infancy: pathologic apnea with no identifiable cause
Apnea of prematurity: pathologic apnea associated with pre-term delivery (generally resolves by 37 weeks)
Periodic breathing: breathing pattern with 3 or more pauses each lasting >3s with 20s of normal breathing surrounding them. |
|
|
Gout vs Pseudogout (crystals, risks, treatment) |
Gout -Negatively birefringent needle urate crystals -Risks: obesity, DM, HTN, diuretics, alcohol, meat, seafood, beer, legumes -Treat: allopurinal (production), probenacid (excretion) chronically; colchicine 1.2/0.6/0.6, NSAIDS, steroids acutely
Pseudogout -Positively birefringent rhomboid calcium pyrophosphate crystals -Risks: hyperparathyroid, hypothyroid, hypoMg, hypoPO4, Wilson's, Hemochromatosis -Treat: As for gout except steroids > NSAIDs/Colchicine; also treat underlying cause but does not affect course. |
|
|
What is Still's disease? Treatment? |
Multisystem inflammatory disorder characterized by fever, arthritis, sore throat, myalgias, pericarditis, hepatitis, splenomegaly, and salmon colored rash that occurs ONLY with the fever.
Treat with NSAIDs, Steroids, IVIg |
|
|
What are the seronegative spondyloarthropathies? |
-They are RF NEGATIVE and HLA B27 POSITIVE . Generally involve the axial skeleton (not extremities)
PAIRS - P soriatic arthritis (affects smaller joints, sausage fingers and psoriasis) A nkylising spondylitis (males, back pain, sacroiliitis, bamboo spine) I nflammatory bowel disease R eiters syndrome / reactive arthritis (post GU chlamydia or GI shigella, salmonella, campylobacter, yersinia infection)
|
|
|
Medial and lateral epicondylitis |
Medial - Pitcher's/Golfer's Elbow -Flex wrist then try to pronate against resistance - pain to medial epicondyle
Lateral - Tennis -Extend and supinate wrist then try to flex against resistance - pain to the lateral epicondyle (Cozun test)
Both - treat with rest, RICE, PT |
|
|
Criteria for the diagnosis of lupus |
Require 4/11 ANA is quite sensitive (good rule-out); anti-DS-DNA & anti-Sm are quite specific (good rule-in)
-Malar rash -Discoid rash -Oral ulcers -Photosensitivity
-Nonerosive polyarthritis
-Serositis (pericardial or pleural effusion) -Renal disorder (nephrotic or nephritic) -Neurologic disorder (seizures or psychosis nos) Hematologic disorder (low Hb, WBC, platelets)
-Immunologic disorder (anti-dsdna, anti-sm, LAC, anticardiolpin, false + syphilis serology) -Positive ANA |
|
|
Drugs that cause drug-induced lupus |
Cardiac: procainamide, amiodarone HTN: hydralazine, methyldopa Antimalarial: quinidine Antimicrobial: nitrofurantoin, penicillin, INH, sulfonamides, tetracycline Anticonvulsant: phenytoin Antithyroid: PTU Antipsychotic: lithium, chlorpromazine Gout: allopurinol |
|
|
Diagnostic criteria for giant cell arteritis |
If you have 2 treat and get biopsy, if you have 3 just treat.
1 - >50yo 2 - new onset localized headache 3 - ESR >50 4 - abnormal biopsy with mononuclear infiltration or granulomatous inflammation |
|
|
Vasculitis classification and key features |
Large vessel: -Takasayu's - pulseless disease, renovascular hypertension -Giant cell - temporal artery headache, amaerosus fugax
Medium vessel: -Polyarteritis nodosa - mostly CNS/GI necrotizing arteritis, no venous involvement, non-granulomatous, palpable purpura, hypergammaglobulinemia, ANCA negative -Buerger's disease - aka thromboangiitis obliterans, 20-40yo male smokers, painful dark phlebitis migrans nodules -Kawasaki disease - Warm CREAM, pediatrics
Small vessel -Goodpasture's - anti-GBM antibody +, alveolar hemorrhage, glomerulonephritis (RPGN). c-ANCA negative (unlike Wegener's) -Microscopic polyangitis - alveolar hemorrhage, glomerulonephritis, nerve involvement. NOT granulomatous (unlike Wegener's). p-ANCA+ (unlike Goodpasture's) -Wegener's granulomatosis - necrotizing granulomatous with upper resp (sinusitis, otitis, ulcers, tracheal stenosis), lower resp (bilat nodular infiltrates with cavitation), renal (RPGN), can have multiple other sx's, c-ANCA + -Churg-Strauss - asthma attacks, allergic rhinitis, eosinophilia. Constrictive pericarditis. -Behcet's - uveitis (also optic neuritis, iritis), apthous ulcers, genital ulcers. -HSP - IgA mediated hypersensitivity vasculitis mostly in <20yo. Fever, lower extremity palpable purpura, abd pain (occasionally intussusception), glomerulonephritis, arthralgias.
Treatment for all is a combo of steroids, plasmapheresis, cyclophosphamide |
|
|
What is serum sickness (pathophys, cause, presentation, treatment)? |
-Type III hypersensitivity response with immune-complex complement fixation in vessel walls. -Associated with penicillin, sulpha, NSAIDs -Get erythema to fingers/toes, then urticaria, lymphadenopathy, arthralgias, constitutional symptoms 7-21 days after exposure. -Give steroids if severe |
|
|
DDx for target lesions |
Pityriasis rosea (herald patch with salmon colored central clearing) Tinea corporis (very well defined) Erythema multiforme (dark center, clearing, dark halo) Urticaria (raised, migratory) Erythema marginatum (dark center, clearing, dark halo similar to multiforme but there is only 1 and it is much bigger) Secondary syphilis
|
|
|
MRSA risk factors |
J ail
S ports H omeless / H ealthcare I VDU R esidence C rowded |
|
|
Antibiotics effective against MRSA |
Clindamycin Septra Doxycycline
Vancomycin Linezolid Cefepime Ceftobiprole
Daptomycin Tigecycline |
|
|
Measles vs Rubella |
Both present with viral exanthems and should get MMR -Measles is highly contagious and classically presents with cough, coryza, conjunctivitis, and Koplic spots. Treat with Ig. Measles rash starts on hand and feet. -Rubella presents with rash, fever and lymphadenopathy with a rash that goes face to trunk. |
|
|
Treatment of pediculitis (lice) and scabies |
Both -Simultaneously treat the patient, sexual partners, family members, clothing, furniture and homes -Clothes should be washed in hot water and dried in a hot dryer. Other things can be frozen for 5 days.
Lice -Permethrin (Nix) 1% shampoo for 10m on day 1 and 8 while avoiding conditioner for 2 weeks
Scabies -Permethrin 5% cream applied for 8-14h on day 1 and 8 |
|
|
Syphilis (Stages, Diagnosis, Treatment) |
Stages -Primary - painless chancre (papule -> 1cm ulcer) with painless lymphadenopathy -Secondary - 6 weeks to 6 months post-exposure, symmetrical non-pruritic macular/papular rash to palms and soles, can have condyloma lata around genitals, fatigue, lymphadenopathy, exanthem, myalgia, pharyngitis -Latent - Nil -Tertiary - gummas, granulomatous ulcerative lesions on skin, liver, bones, brain
Treatment -VDRL is positive after primary syphilis. Used for screening (false positives in SLE, thyroiditis, lymphoma, post-vaccine, mycoplasma, mono, hepatitis, measles, malaria, pregnancy) -FTA used for diagnosis (flouresence treponomal antibody test)
Treatment -Primary & secondary: Benzathine penicillin 2.4 million U IM; VDRL goes non-reactive after ~12 months -Persistent or tertiary: treat weekly -Watch for Jerisch Herscheimer reaction |
|
|
Pemphigus vulgaris vs bullous pemphigoid |
PV -Autoimmune reaction affecting patients 50-60yo generally on penicillamine, captopril or rifampim -Present with oral bullae -> painful ulcers then skin bullae -> painful ulcers -Diagnose with history, + Nikolski sign, + Tzank smear -Treat with high dose prednisone (100-300mg/d), immunosuppresants, plasmapheresis
BP -IgG autoimmune reaction of those ~65yo. Less sick than PV. -Present with tense, fluid-filled blisters and a negative Nikolski sign. Mucous membrane involvement is possible but less frequent than PV. -Treat with prednisone and other immunosuppresants for 2-5 years and it generally resolves. |
|
|
Canadian C-Spine Rule |
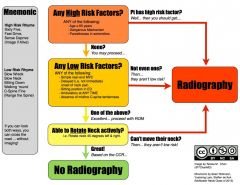
|
|
|
Indications for dialysis in renal failure |
AEIOU
A cidosis / A lkalosis (note: HCO3 can precipitate tetany/convulsions in the setting of hypoCa) E lectrolyte abnormalities (HyperK, HyperMg, HyperCa - MM) I ngestions that are dialyzable O verload of fluid (CHF, pulmonary edema, severe HTN) U remia (pericarditis, N/V, lethargy) |
|
|
Bacteria causing UTI's |
KEEPPSSS
K lebsiella (institutionalized, newborns) E nterococcus (institutionalized) E coli (>80% of UTI's) P roteus (3-11yo) P seudomonas S taphylococcus saprophyticus (can be normal skin flora in perineum) S erratia S almonella |
|
|
UTI treatment length |
Uncomplicated lower tract - 3 days with nitrofurantoin, cefixime, cipro, septra
Complicated lower tract - 7 days (diabetes, sickle cell, immunocompromised) with cefixime, cipro, septra
Pregnancy lower tract - 10 days with cefixime or nitrofurantoin (avoid near term due to hemolytic anemia) or septra (avoid near term due to hemolytic anemia, jaundice, kernicterus)
Upper tract - 10-14 days with cefixime or ceftriaxone |
|
|
Types of kidney stones and causes |
Calcium oxalate 75% - excess calcium (milk alkali syndrome, high dietary intake, antacids, increased PTH). Oxalate increases in radiation enteritis, IBD, and ethylene glycol ingestion.
Struvite 15% - infection with urea-splitting organisms (pseudomonas, proteus, klebsiella, staph)
Hyperuricemia 10% - gout, tumor lysis syndrome, hematologic malignancies. they are radioluscent.
Cysteine 1% - inborn error of metabolism
Struvite, urate, and cysteine stones can form staghorn calculi. |
|
|
5 locations of urinary obstruction |
Renal calyx UPJ (uretopelvic junction) Pelvic brim UVJ (uretovesicular junction) Vesicular orifice |
|
|
Acute scrotal pain / swelling differential and physical exam features |
Pain -Testicular torsion - negative cremasteric reflex -Torsion of the testicular appendage (appendix testis or appendix epididymis) - blue dot sign -Epididymitis - Prehn's sign -Trauma -Orchitis -Testicular tumor WITH hemorrhage (normally tumor is not painful) -Inguinal hernia (if incarcerated/strangulated)
Swelling -Varicocele (bag of worms) -Ideopathic scrotal edema -Hydrocele
|
|
|
Causes of varicocele |
Venous varicocities of spermatic veins (bag of worms)
-Right spermatic vein -> IVC - generally caused by IVC compression or thrombosis -Left spermatic vein -> left renal vein - generally caused by RCC |
|
|
Approach to priapism |
Determine low (painful) or high (not painful) flow
Treatment of low flow ->4h duration requires treatment -Noninvasive tx - walk up stairs (decrease flow to penis), ice packs, compress -PO treatment - terbutaline 5-10mg PO (beta agonist) -Analgesia with dorsal nerve block -Aspiration of cavernosum -Injection of alpha agonist (phenylephrine) or methylene blue -Sicklers get O2 and hydration as well
Treatment of high flow -Angiography, surgical shunt, if painful can do block |
|
|
Causes of false positive hematuria |
Myoglobin Porphyria Bilirubinuria
Meds -Nitrofurantoin -Rifampin -Chloroquine/Hydroxychloroquine -Iodine bromide
Foods -Food coloring -Beets -Rhubarb -Berries |
|
|
Nephrotic vs Nephritic syndrome |
Nephrotic - HALEH H ypoalbuminea A lbuminurea (>3.5g/d proteinuria) L ipiduria E dema H yperlipidemia (and clotting - produce increased clotting factors)
Nephritic - PHAROH P roteinuria (<3.5g/d) H ematuria (micro or macroscopic) A zotemia (increased urea/Cr) R BC casts O liguria (<400mL/d) H ypertension |
|
|
Causes of amenorrhea |
-Hypothalamic - exercise, stress, anorexia, hypothalamic tumor, GnRH deficiency
-Pituitary - primary hypopituitarism, Sheehan syndrome, pituitary tumor
-Ovarian dysfunction - PCOS, gonadal dysgenesis (Turner's), menopause, radiation/chemo
-Endocrine - Hyperprolactinemia, hyper/hypothyroidism, Cushing's, hyperandrogenism (PCOS)
-Obstruction - imperforate hymen, cervical stenosis |
|
|
Definition and causes of menorrhagia and metrorrhagia |
Menorrhagia is prolonged (>7d) or heavy (>80cc) bleeding
Metrorrhagia is bleeding at irregular intervals (e.g. between periods
Non-structural (COTIPE) C oagulopathy O vulatory dysfunction (ovulation, anovulation, exogenous steroids) I atrogenic (OCP) / I nfectious (endometritis, cervicitis, vaginitis) P regnancy (implantation, ectopic, abortion, molar) E ndometriosis E ndocrine (Cushing's)
Structural (PLAMT) P olyps L eiomyoma A denomyosis M alignancy (Endometrial / Cervical / Ovarian cancer) T rauma (sexual abuse, foreign body) |
|
|
Treatment of unstable (stable) uterine bleeding |
-Premarin 25mg IV q4-6h until bleeding stops along with an antiemetic (2.5mg PO bid-qid - follow up with progesterone for normal withdrawal bleeding OR 5-4-3-2-1 regular OCP's/day then 1 pill x 7 days, then 4 day period and restart) -Tranexamic acid 1g IV (1g PO tid-qid while menstrating) -Intrauterine foley to tamponade bleeding -OR - D&C / Hysterectomy |
|
|
Causes of false BhCG test |
False positive -Post-menopausal (usually <10) -Abortion (x 60 days) -BhCG secreting tumor (hydratiform mole) -Exogenous source (e.g. to induce ovulation) -Incomplete abortion, abortion with 2nd fetus, abortion with heterotopic ectopic
False negative -Dilute urine early in gestation |
|
|
DDx for hematuria (>5RBC / hpf) |
Hematological/Cardiac -Sickle cell (infarcts) -Coagulopathy -Endocarditis
Renal -Glomerular - primary glomerulonephritis (post-strep) or secondary glomerulonephritis (HUS, TTP, SLE, PAN, PAN, Wegener's, Goodpastures) -Nonglomerular - trauma, pyelonephritis, AIN, RCC, infarct, AVM, Polycystic Kidneys, Exercise
Postrenal -Ureter - stone, TCC -Bladder - trauma, TCC, cystitis -Prostate - prostatitis, BPH, prostate cancer -Urethra - Foley, urethritis
False -Myoglobin -Menstration -Traumatic cath -Drugs (rifampin, nitrofurantoin, chloroquine/hydroxychloroquine) -Feeds (beets, berries, food coloring) |
|
|
DDx for proteinuria |
Glomerular (can be >10g/d) -Nephrotic syndrome, minimal change disease, membranous GN, focal segmental glomerulosclerosis, Post-strep GN, IgA nephropathy
Tubular (generally <2g/d) -UTI -AIN -Sickle cell
Overflow -Multiple myeloma, Waldenstrom's macroglobulinemia, Amyloidosis
Other -Orthostatic proteinuria -Pregnancy -Exertion, stress
|
|
|
What is ATN and its diagnostic criteria? |
Acute Tubular Necrosis -Death of the tubular epithelium of the kidney -Generally caused by toxins (HHS, rhabdo, hemolysis, aminoglycosides, contrast) and hypoperfusion (shock) -See FENa >1%, Urine Na >40 |
|
|
Requirements for the use of methotrexate in an ectopic pregnancy |
-Patient is hemodynamically stable -Tubal mass is <3.5cm -No FHR -No signs of rupture (FF) -BhCG <1200-5000 |
|
|
Shoulder dystocia: problem, risk factors, diagnosis, treatment |
Problem: vertical (rather than oblique) shoulder orientation of fetus (sacropubic)
Risk factors: maternal obesity, DM; fetal macrosomia; pregnancy post-date, prolonged 2nd stage
Diagnosis: can not deliver either shoulder, turtle sign
Treatment: HELPER H elp (obs, anesthesia, neonatal) E pisiotomy (oblique) / E mpty bladder L egs flexed (McRoberts maneuver) P ressure suprapublically to push the anterior shoulder down and to the side E nter vagina (Rubin - post most accessible shoulder toward fetal chest; Woods - rotate 180 degrees Rubin plus spin the opposite hip the other direction) R emove posterior arm (grab hand and sweep arm across the chest and deliver it with the shoulder; can have humerus and brachial plexus injury)
Other: -Break the babies clavicle -Symphesotomy
|
|
|
BLS Termination of Resuscitation |
No defibrillation by AED No ROSC prehospital Not witnessed by EMS |
|
|
ALS Termination of Resuscitation |
No defibrillation No ROSC prehodpitsl Not witnessed by EMS Not witnessed by bystanders No bystander CPR |
|
|
Risk factors for death due to asthma |
Asthma history -Intubation/ICU admission for asthma -Hospitalized 2 or more times in past year -To ED 3 or more times in past year -Hospitilization/ED visit in past month ->2 MDI canisters of B-agonist/month -Using or withdrawing from corticosteroids -Difficulty perceiving asthma severity/symptoms
Social history -Low socioeconomic status -Psychosocial problems -Illicit drug use (especially cocaine/heroin)
Comorbidities -Cardiovascular disease -Chronic lung disease -Psychiatric disease |
|
|
Definition and classification of COPD |
Irreversible, progressive airway destruction secondary to an abnormal inflammatory response.
Chronic bronchitis: productive cough for >3 months in the past 2 years; high pCO2 Emphysema: destruction of the lung parenchyma due to imbalance of elastase/antielastase from inflammation; low pCO2 (breath a lot to maintain pO2)
4 classes in the Gold Classification - all have FEV1/FVC < 70% I Mild FEV1>80%; no symptoms II Moderate FEV1<80%; AECOPD and SOBOE III Severe FEV1 <50%; affects QoL IV Very Severe FEV1 <30%; R heart failure 4 |
|
|
Define AECOPD. What decreases mortality in COPD? |
An acute Exacerbation of COPD is characterized by the Antonisen criteria: 1) increased dyspnea, 2) sputum production, or 3) sputum purulence. Generally need 2/3 to treat.
Mortality in COPD is decreased by 1) quitting smoking and 2) chronic oxygen therapy |
|
|
Indications for intubation and mechanical ventilation? |
-Respiratory arrest -Decreased LOC despite maximal therapy -Cardiovascular instability -NIPPV failure or unable to use (exclusion criteria) -Severe dyspnea -Severe tachypnea -Life-threatening hypoxia -Severe acidosis / hypercapnea -Severe illness requiring respiratory support |
|
|
Complications of posterior nasal packing |
B radycardia |
|
|
Distinguish epiglottitis, peritonsillar abscess, retropharyngeal abscess |
Lingual tonsillitis - hot potato voice, pain on tongue depression, scalloped anterior valecula
Epiglottitis - hyoid tenderness and muffled (not hoarse) voice, sniffing position
Peritonsillar abscess - hot potato voice, drooling, hallitosis, trismus, inferomedially displaced tonsil
Parapharyngeal abscess - same as peritonsillar except can have Horner's and oral/nasal/aural bleeding from carotid.
Retropharyngeal abscess - supine with head extended, neck pain, meningismus, cri du canard (duck quack voice) |
|
|
Complications of deep space infections of the posterior pharynx |
Airway compromise Mediastinitis Pericarditis Pneumonia Empyema Lemierre's syndrome (jugular vein thrombophlebitis) Horner's (sympathetic chain) Carotid artery erosion or pseudoaneurysm Cavernous sinus thrombosis Mastoiditis Otitis Meningitis Brain abscess |
|
|
How does O2 increase the speed of PTx resolution? |
Decreases the partial pressure in the blood and as per Henry's gas law this results in the N2 from the PTx being resorbed more quickly into circulation. It increases resorbtion from 1-2%/d to 4-8%/d |
|
|
How do you calculate the size of a PTx in %? |
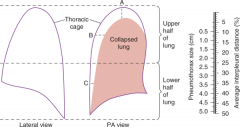
((A + B + C)/3) x 10% |
|
|
What are light's criteria? |
Distinguishes between exudative and transudative effusion
Exudative have at least one of: Pleural fluid >2/3 of upper level of normal serum LDH Pleural LDH/serum LDH >0.6 Pleural protein/serum protein >0.5
Highly sensitive, less specific for exudate |
|
|
Causes of miscarraige |
Two main: -Chromosomal anomolies -Uterine malformations (leiomyoma, bifid uterus, uterine scarring, cervical incompetence)
Other: -Increased maternal/paternal age -Low pre-pregnancy BMI -History of miscarriage -History of vaginal bleeding -Maternal stress -Increased parity -Autoimmune disease -Endocrine disorders (DM) -Maternal infections -Maternal toxin ingestion (cocaine, EtOH) |
|
|
Categories of hypertension in pregnancy |
Hypertension in pregnancy: >140/90 Preeclampsia: A disorder of pregnancy characterized by hypertension and proteinuria during pregnancy that is thought to be due to endothelial dysfunction
Types of hypertension in pregnancy Chronic hypertension: dx'd before 20 weeks Gestational hypertension: dx'd after 20 weeks and no proteinuria Pre-eclampsia with chronic hypertension: proteinuria (>300mg/24h) and BP >160/110 in a patient with known hypertension Pre-eclampsia: proteinuria (>300mg/24h) and BP >140/90 |
|
|
Amniotic fluid embolism: pathophysiology, major causes, presentation |
Pathophysiology: release of amniotic fluid into the circulation causing an anaphylactoid reaction
Causes: labor, amniocentesis, uterine manipulation (version), placental separation. Can also occur during miscarriage/abortion and spontaneously.
Presentation: hypoxemia due to plugging of pulmonary vessels, cardiovascular collapse, non-cardiogenic pulmonary edema, DIC
Treatment: aggressive ventilatory and hemodynamic support. Plasma exchange to remove cytokines. Delivery of fetus. |
|
|
Diagnostic algorithm for PE in pregnancy |
If leg symptoms -> compression U/S (treat if pos) If no leg symptoms or U/S neg -> CXR If CXR clear -> V/Q scan If V/Q inconclusive -> CTPE If CXR abnormal -> CTPE If CTPE neg -> stop
|
|
|
Hyperemesis gravidarum: definition, onset, |
Definition: emesis that causes starvation metabolism with weight loss, dehydration, ketonuria, and ketonemia
Onset: 6-20 weeks
Pathyphys: unsure, associated with increased B-hCG, molar pregnancy, and multiple gestation
Management: fluid rehydration, enteral nutrition, diclectin (doxylamine and B6) up to 8 tabs/d then gravol then zofran/maxeran then methylprednisone |
|
|
What is a teratogen? What characteristics of a drug increase its ability to cross the placenta? |
Any chemical, pharmacologic, environmental or mechanical agent that can cause deviant or disruptive development of the conceptus
Characteristics that increase crossing the placenta Size (small), ionization (uncharged), protein binding (free drug), pKa (weak organic acids get caught in fetal base-ness), lipid solubility (more soluble) |
|
|
List 10 teratogens |
Heavy metals/toxins: Lead, CO, Iodine Anticoagulant: Warfarin Antiarrhythmics: Amiodarone, Quinine Anti-inflammatories: NSAIDs, misoprostol Antiepileptics: Phenytoin, VPA, carbamazepine Chemotherapeutics Busulfan, methotrexate, thalidomide Anti-hypertensives: ACEI, ARBs Dermatologic: Retinoic acid derivatives Androgens/Estrogens: OCP, HRT, diethylstilbestrol Antipsychotics: Lithium Drugs of Abuse: EtOH, cocaine Antibiotics: Erythromycin, tetracycline, aminoglycosides |
|
|
Distinguish true labor from false labor |
True labor -cyclic uterine contractions of increasing frequency, duration, and strength -cervical dilation -bloody show
False labor (Braxton-Hicks contractions) -no cervical dilation or effacement -intact membranes -do not escalate in frequency, duration or strength -not sensed by external monitors |
|
|
What is assessed on pelvic exam in true labor? How can fontanelles be distinguished? |
Cervical dilation, cervical effacement, presenting part, station of presenting part, orientation of presenting part
The anterior fontanelle has 4 sutures while the posterior fontanelle has 3. OA is the most common presentation. |
|
|
Steps to breech delivery |
-Get a C-section instead -Call obstetrics -Monitors -Rule-out prolapsed cord -Open pelvis (knees wide) -Episiotomy -When abdomen is through pull out 10-15cm of cord to try to avoid it getting trapped -Grasp neonate by the pelvis and direct face/abdomen away from the symphysis -Keep the next flexed forward (do not let it extend!! Causes spinal cord injury)
|
|
|
Umbilical cord prolapse: diagnosis and treatment |
Diagnosis: see the cord on pelvic, suddenly non-reassuring FHR
Treatment: emergency C-section, mother in knee to chest position with head down, fingers elevate presenting part, Foley to install 500-750 cc of fluid into bladder, replace cord above the presenting part |
|
|
Uterine prolapse: risk factors, diagnosis and treatment |
Risk factors: -Primip -Oxytocin use -fundal implantation -forceful traction on umbilical cord -MgSO4 use
Diagnosis -Severe abdominal pain -Visualization of the uterus at the os or in the introitus
Treatment -Do NOT remove the placenta while the uterus is out -Give tocolytics (terbutaline, MgSO4, halogenated anesthetics to relax the uterine ring -Replace uterus -Then start oxytocin |
|
|
DDx for diffuse wheeze |
Pulmonary -Lower airway o Congenital: CF, Bronchopulmonary dysplasia o Trauma: FB, Aspiration o Infectious: Pneumonia, Bronchiolitis, COPD o Inflammatory: Anaphylaxis o Vascular: PE o Degenerative: Sarcoidosis -Upper airway o Congenital: Vascular ring o Trauma: FB, Caustic ingestion o Infectious: Epiglottitis, Croup, Retropharyngeal abscess o Inflammatory: Anaphylaxis, Angioedema o Neoplastic o Vascular ring Extra-pulmonary -CHF -ARDS |
|
|
Asthma severity classifications |
PEFR Mild >70% predicted Moderate 40-70% predicted Severe <40% predicted Life threatening <25% |
|
|
Side effects of steroids |
SHORT TERM o Insomnia o Mood alterations or Psychosis o GI upset o Increased appetite/weight gain o Fluid retention o Hyperglycemia o Hypokalemia
LONG TERM o Hyperglycemia o Osteoporosis o Thin skin, easy bruising, poor wound healing o Rare: HTN, PUD, AVN, Allergic reaction o Adrenal suppression if > 4 courses/year |
|
|
Soft signs of arterial injury in neck trauma |
FOAHHDDS |
|
|
Risk factors for primary and secondary PTx |
Primary: -Tall, skinny, male smokers with Marfan's and Mitral valve prolapse at altitude
Secondary: -Airway: cystic fibrosis, asthma, COPD -Infectious: TB, PJP, lung abscess, necrotizing -Interstitial: sarcoid, fibrosis, pneumoconioses, tuberous sclerosis -Neoplasm: primary or metastatic -Miscellaneous: endometriosis, pulmonary infarction |
|
|
When is a diagnostic thoracentesis indicated? |
Unexplained pleural effusions
Pneumonic and parapneumonic effusions -Pneumonia with a parapneumonic effusion >10mm wide on decubitus films -Loculated pleural effusion -Thickened pleural core
Diagnosis of a possible malignancy |
|
|
Indications for bicarbonate therapy |
-pH <7.1 -HCO3 <12 -Refractory hypotension (to pressors) -TCA toxicity -ASA toxicity -Phenobarb overdose -Ethylene glycol and methanol ingestion
Empiric dose is 1 mEq/kg with 1/2 as a bolus and 1/2 over 4 hours |
|
|
How can bicarbonate cause a paradoxical intracranial acidosis? Other complications? |
Paradoxical CNS acidosis -HCO3 diffuses over the BBB slowly -HCO3 in the plasma is converted by carbonic anhydrase to CO2 which is then blown off to decrease pH -This CO2 can diffuse quickly over the BBB decreasing the CNS pH -With the improved pH the RR is decreased increasing CO2 which again crosses the BBB
Other complications -Hypernatremia -Hyperosmolarity -Hypocalcemia -Hypokalemia |
|
|
Metabolic alkalosis: causes |
Causes: hypovolemia, hypokalemia, hypochloremia
DDx: -Volume contracted (saline responsive, urine Cl<10): Vomiting, diarrhea, NG suction, diuretics -Normal or expanded volume (saline unresponsive, urine Cl>10): primary hyperaldosteronism (Conn's, CAH), secondary hyperaldosteronism (CHF, cirrhosis, nephrotic syndrome, Cushing's, Barter's, Licorice, ectopic ACTH) -Other: milk-alkali syndrome, citrate, nonparathyroid hypercalcemia
Treatment -Saline responsive: fluid and acetazolamide -Saline resistant: replace K and spironolactone (aldosterone antagonist) |
|
|
K - symptoms of hyperkalemia and hypokalemia |
Hyperkalemia: -CVS: dysrhythmias (heart block, WCT, sine wave pattern) -CNS: muscle cramps, weakness, paralysis, paresthesias
Hypokalemia (sloooow muscles): -CNS: lethargy, depression, irratibility, confusion, paresthesias, decreased reflexes, weakness -CVS: dysrhythmias (heart blocks, AF) -GI: N/V, ileus -MSK: myalgias, rhabdo, weakness |
|
|
Na - symptoms of hypernatremia and hyponatremia |
Hypernatremia: -General: fatigue, malaise, anorexia, N/V -CNS: seizures, AMS, coma -MSK: twitching, hyperreflexia, clonus, tremor -Skin: dry and doughy
Hyponatremia: -Nonspecific: nausea, malaise, anorexia -CNS: HA, AMS, decreased LOC, seizures, focal neural deficits -MSK: cramps, weakness
|
|
|
Definition of DKA |
Due to a lack of insulin and increase in glucagon leading to hyperglycemia, osmotic diuresis, and ketoacidosis.
Glucose >13.9mmol/L (peds <11) pH <7.3 HCO3 <18 (peds <15) Serum or urine ketones |
|
|
How does iodide bolus affect thyroid hormone production? |
2 possible effects:
Wolff-Chaikoff effect: excess iodide inhibits ion trapping, thyroglobin iodination, and blocks the release of thyroid hormone
Jod-Basedow effect: in patients with Graves or multinodular goiter who are iodine deficient it can induce hyperthyroidism |
|
|
Thyroid storm: cause, precipitants, and treatment |
Cause: increased T3/T4 over a prolonged period of time increases B receptors and sympathetic surge activates them all at once.
Precipitants: -Trauma (burns, surgery, thyroid trauma) -Vascular (MI, CVA, PE, CHF) -Toxicologic (Iodine, radiocontrast, hormone ingestion, amiodarone, stopping therapy, ASA, chemo, pseudoephedrine, OP's) -Sepsis -Metabolic: hypo or hyperglycemia -Pregnancy -Psych: mania, emotional crisis
Treatment: -Decrease hormone production with PTU 1g po -Decrease release of preformed hormone with Saturated Solution of Potassium Iodide (SSKI) 5 drops 1h after PTU; Li works too -Beta blockade with propranolol 1-2mg IV q15m -Prevent T4->T3 conversion with hydrocortisone 100mg IV -Prevent enterohepatic circulation with cholestyramine -Prevent entry of thyroid hormone into cell with L-Carnitine -Supportive care with cooling, benzos, acetaminophen -Remove thyroid hormones with plasmapheresis, dialysis, plasma exchange -Treat precipitant -Admit to ICU -Thyroid surgery or ablation |
|
|
Myxedema coma: cause, precipitants, and treatment |
Cause: severe longstanding hypothyroidism with a precipitant
Precipitants: -Trauma, burns -Vascular: CVA, GIB, MI -Toxicologic: lithium/iodide (decrease release), narcotics, benzo's, barbiturates -Metabolic: hypoglycemia, hyponatremia, hypoxia, DKA, hypercapnea -Cold exposure
Treatment -ABC's - note macroglossia/mucosal swelling -IVF - watch Na and glucose (often need to be added) -Thyroid hormone - T4 if old/cardiac hx (T4 300-500ug IV bolus); T3 if young (T3 10-20ug IV bolus). Can also give a bit of each. -Hydrocortisone 100mg IV -Rewarming -Treat precipitant |
|
|
Treatment of upper and lower esophageal foreign body |
Upper: -Magill forceps / Glidescope -Foley -Bougienage -Endoscopy
Lower: -Pop -Glucagon -Maxeran -Nifedipine -SL nitro -Midazolam sedation -Endoscopy |
|
|
Indications for immediate endoscopy of an esophageal foreign body |
-Complete obstruction (unable to handle secretions) -Respiratory distress (FB in esophagus can compress trachea) -Sharp objects -Impacted for 24 hours -Coins in the proximal esophagus -Alkaline button batteries -Failure of medical treatment -Coins in children <2yo (relative) |
|
|
Complications of esophageal FB's |
-Abscess -Tracheo-esophageal fistula -Aorto-enteric fistula -Perforation and mediastinitis / pneumothorax / pneumomediastinum |
|
|
Indications for immediate removal of a foreign body in the stomach |
>2.5cm wide >5cm long Sharp Toxic (e.g. lead) >3-4 weeks impaction
90% of objects that make it to the stomach make it all the way through. If past the pylorus things can generally be left alone (then require surgery rather than endoscopy). Remove if hasn't moved in 3-4 weeks. |
|
|
Indications for surgery to remove a foreign body in the small intestines |
>99% of these pass without problem
-Hasn't moved for >7 days -Hasn't passed in >4 weeks ->1 industrial strength magnet (not a fridge magnet) |
|
|
Grades and treatment of hepatic encephalopathy |
Grades I - Depression, irritability, disordered sleep, mild cognitive dysfunction II - Lethargy, disorientation, asterixis III - Somnolence, disorientation, confused speech IV - Coma
Treatment -Stop all sedatives / CNS depressants -Correct hypokalemia (allows ammonia to be excreted renally) -Remove GI protein (treat bleed, decrease protein intake, treat constipation) -Give lactulose 30mL qid (becomes lactic acid and traps NH4+ and decreases transport time) -Flagyl or Clarithromycin to kill NH3 producing gut flora -Acarbose to decrease NH3 production -MARS |
|
|
How does lactulose correct hepatic encephalopathy? What are other treatments? |
Lactulose is converted to lactic acid, acidifying the bowel contents. This converts ammonia (NH3) to ammonium (NH4+) and its positive charge keeps it trapped in the lumen.
Remove other sources of protein (e.g. NG for GIB, protein-restricted diet) Clarithromycin or Flagyl (alter gut flora to decrease ammonia production) Acarbose (changes bacterial activity to decrease ammonia) |
|
|
What is the SAAG? How is it interpreted? |
SAAG = serum-ascites albumin gradient (serum albumin - ascites albumin) This replaces the distinction between transudate/exudate
SAAG<11 = inflammation or decreased oncotic pressure (Carcinomatosis, TB, Pancreatic or biliary ascites, nephrotic syndrome) SAAG>11 = portal hypertension (Cirrhosis, Alcoholic hepatitis, portal-vein thrombosis, Budd Chiari, liver mets) |
|
|
Diagnosis of SBP. Differentiating primary versus secondary bacterial peritonitis |
Diagnosis: -PMN >250 cells/mm3 -Positive culture -Ascites fluid pH <7.34 or a gap between blood pH of >0.10
Primary: -Protein <10 -Prior SBP -Bili >42mmol/L -Platelets <98 -Single bacteria cultured
Secondary: -Protein >10 -Glucose <2.8 -LDH > upper limit of normal serum LDH -Multiple types of bacteria cultured |
|
|
The triad and tetrad of ascending cholangitis |
Charcot's triad: -Fever -Jaundice -RUQ pain
Raynaud's pentad: -Charcot's triad plus altered mental status and shock (hypotension/tachycardia) |
|
|
Sonographic findings of an abnormal TV ultrasound |
-BhCG >3000 and no gestational sac -Gestational sac >13mm and no yolk sac ->5mm crown rump length and no fetal heart tones -No fetal heart tones after 10-12 weeks -Gestational sac >25mm and no fetus |
|
|
Risk factors for ectopic pregnancy |
PMHx - PID, previous ectopic or abortion, tubal surgery, infertility, abnormal anatomy Patient factors - smoker, age Pregnancy factors - has IUD, embryo transfer fertility treatments |
|
|
What is a molar pregnancy? What are the types? How does it present |
-Disordered proliferation of chorionic villi
Two types: -Complete hydatidiform mole: absence of fetal tissue -Incomplete hydatidiform mole (much less common): fetal tissue with focal trophoblastic hyperplasia -Can also get choriocarcinoma (responds well to chemo, can metastasize)
Presentation -Hyperemesis gravidarum -Crazy high BhCG -Snowstorm U/S |
|
|
Numbness or pain to the outer side of the thigh associated with pregnancy or obesity |
-Meralgia paresthetica -Due to compression of the lateral femoral cutaneous nerve of the thigh as it passes the inguinal ligament |
|
|
Cause and treatment of postpartum hemorrhage |
Cause: Tissue - retained products, accreta (placental villi adhere to myometrium) / increta (enter the myometrium) /percreta (through the myometrium) make more likely Tone - diagnosis of exclusion Trauma - perineal tears, vulva/vaginal epithelium trauma Thrombin - vWD, coagulopathy, DIC
Treatment Uterine massage Repair lacerations Remove products of conception Oxytocin - run 40U/1L fast; 10U IM Misoprostol (PGE1) - 800-1000mcg PR Hemabate (PGFalpha) - 250mcg IM Pack uterus Foley in uterus Embolize vessels D&C Hysterectomy |
|
|
Types of lactic acidosis |
A - tissue hypoxia B1 - systemic disorders (DM, renal insufficiency, leukemia, sepsis) B2 - substance associated (biguanides, methanol, salicylates, INH) B3 - heritable metabolic disease |
|
|
Risk factors, presentation, and treatment of cerebral edema in DKA |
Risk factors -New onset diabetes -Children <5yo -Extremely ill on presentation -Treated with HCO3 -Excessive fluid replacement -Rapidly dropping serum osmolality
Presentation -HA -Behavioral changes -Incontinence -Seizures -Autonomic (BP and temp) Then coma, respiratory arrest, death
Treatment -Mannitol 1-2g/kg over 15m -Decrease IVF and insulin rate -Intubate, hyperventilate, CT head
NB - cause is unknown - ? idiogenic osmoles |
|
|
4 characteristics that determine the toxicity of a hydrocarbon |
•Viscosity |
|
|
Diagnostic criteria of HHS |
Glucose >33 Sosm >320 pH >7.3 HCO3 >15 |
|
|
Complications of long-term DM |
Infection (immunocompromised secondary to decreased neutrophil and lymphocyte activity) Diabetic foot Insulin allergy (must go desensitization or change type) Cutaneous manifestations (diabetic dermopathy, dermal hypersensitivity at injection sites as well as hypo or hypertrophy, acanthosis nigrans, necrobiosis lipoidica diabeticoricum, xanthoma diabeticorum) Macrovascular complications (CAD, CVD, PVD) Microvascular complications (Nephropathy, Retinopathy, Neuropathy) |
|
|
Causes of rhabdomyolysis |
Traumatic -Crush -Compartment syndrome -Excessive exertion
Non-traumatic (relate to lack of ATP) -Electrolytes (HypoK or HypoP) -Ischemia -Congenital ATP deficiency due to inborn errors of metabolism -Environmental (electrical injury, heat stroke, hypothermia, rattle snake bite) -Endocrine (pheochromocytoma, DKA, HHS, hypo/hyperthermia) -Toxin (SS, NMS, statins, alcohol) -Infections (all types) -Seizures -Rheumatic (polymyositis, dermatomyositis, Sjogren's) |
|
|
Thyroid diseases |
Hyperthyroid -Graves (TSH receptor antibodies) -Toxic multinodular goiter (multiple overactive and big areas, can cause SVC syndrome) -Toxic adenoma -Acute thyroiditis (gland is tender) --> Autoimmune (Hashimoto's antibody to thyroid peroxidase; Postpartum; Sporadic) --> Infectious (De Quervian's viral; suppurative bacterial) --> Drug induced (amiodarone, iodine, interferon, lithium) -Pituitary adenoma -Gestational trophoblastic / germ cell tumors (create TSH-like hormone)
Hypothyroid -Hypothalamic and pituitary underactivity (tumors, Sheehan's, amyloidosis, sarcoidosis, radiation) -Late thyroiditis (as per above) -Iatrogenic (thyroidectomy, ablation, lithium, iodine, amiodarone) -Congenital (causes cretinism)
|
|
|
Primary versus secondary adrenal dysfunciton |
Primary is a disease of the gland itself and affects all 3 functions (glucocorticoids, mineralocorticoids, androgens) -See hyperpigmentation, hyperkalemia, hyponatremia, salt craving, and acidosis from the lack of aldosterone / excess ACTH
Secondary is a disease of the pituitary and does NOT affect mineralocorticoids (regulated by the RAAS) -Still get hyponatremia, but it is due to increased ADH
Both -Hypotension -Depression, delerium, HA, abdominal pain, emesis, hypoglycemia, hyponatremia (differnet reasons), hypercalcemia, fevers, ARF |
|
|
Steroid equivalency (hydrocortisone, prednisone, methylprednisolone, dexamethasone) |
Hydrocortisone = 1 Prednisone/Prednisolone = 4 Methylprednisolone = 5 Dexamethasone = 25 |
|
|
Esophageal narrowings and risk factors for obstruction / dysphagia |
Narrowings -Upper esophageal sphincter (cricopharyngeus) -Aortic arch -Left mainstem bronchus -Lower esophageal sphincter
Causes of obstruction / dysphagia
Poor dentition (they don't chew)
Intrinsic -Esophageal carcinoma -Shatzki's ring -Peptic stricture -Esophageal web
Extrinsic -Cardiomegaly -Aortic aneurysms or anomylous right subclavian -Goiter -Mediastinal tumor -Enlarged lymph nodes -Zenker's diverticulum
Neuromuscular (Neuro - head trauma, brain tumor, CVA, Alzheimer's, Parkinsons, MS, ALS, Myesthenia; Muscular - achalasia, scleroderma)
Toxic (Lead or EtOH)
Infectious (Bacteria - diptheria, botulism, syphilis, tetany OR Viral - rabies, polio) |
|
|
What is Mackler's triad? How can the problem be diagnosed? |
Suggests esophageal rupture
-Subcutaneous emphysema -Chest pain -Vomiting
Diagnose with contrast study. Use gastrograffin if no risk of aspiration (safer but less sensitive test; pneumonitis if aspirated) THEN barium (worse inflammatory response through perforation). Try CT if normal or unsafe to do. |
|
|
Contributors to thte development of GERD and evidence-based ways to get rid of it |
-Decreased sphincter tone (anticholinergics, caffeine, benzo's, nicotine, nitrates, peppermint, chocolate, estrogen, progesterone) -Decreased esophageal motility (DM, achalasia, scleroderma) -Increased intraabdominal pressure (pregnancy, obesity) -Decreased gastric emptying (anticholinergic, diabetic gastroparesis, outlet obstruction)
Evidence-based treatments: weight loss and bed elevation |
|
|
Eradication treatment for H Pylori |
Triple: Clarithromycin 500bid / Amoxicillin 1000bid OR Metronidazole 500bid/ PPI x 10-14d
OR
Quadruple: Bismuth subsalicylate (pepto-bismol) 525qid / metronidazole 250qid / Tetracycline 500qid / PPI x 10-14d |
|
|
Poor predictors of outcome in upper esophageal bleed |
Components of the Rockall score
Age >60 Heart failure Ischemic heart disease Renal failure Liver failure Metastatic cancer Gastric cancer Vigorous bleeding |
|
|
DDx for transaminitis |
-Structural: o Inflammatory/ Autoimmune/ Infiltrative: autoimmune hepatitis (PBS, PSC), NASH (? d/t insulin resistance), amyloid o Vascular: Budd-Chiari (thrombosis of hepatic veins or IVC/SVC), portal vein thrombosis, ischemia, CHF o Congen/Degen: neonatal hepatitis -Toxicology: acetaminophen, EtOH, INH, iron, phenytoin, ecstasy (autoimmune hepatitis) -Infection: o Viral: HAV, HBV, HCV, HDV, HGV, EBV, CMV o Protazoan: amoeba o Toxoplasmosis o Associated with bacterial sepsis -Metabolic: Wilson’s disease (copper overload), Reye’s syndrome, hemochromatosis -Pregnancy: Fatty liver of pregnancy -GI: gallstones, strictures, cholangitis, biliary/pancreatic cancer, annular pancreas (obstructive causes) |
|
|
Hepatitis serology |
Hep A -For acute infection send HAV IgM -For chronic infection send HAV IgG
Hep B -For acute infection send HBV sAg and HBV cAb IgM -For chronic infection send HBV cAb IgG -For vaccine immunity send HBV sAb
Hep C -HCV Ab |
|
|
Hepatitis post-exposure prophylaxis |
A: HAIg to unvaccinated close personal contacts, childcare workers/attendees (people who wipe their bum), similar food-borne source in last 2/52
B: HBIg to: -unvaccinated / low titer recipients exposed to source that is HBV sAg + OR high risk -neonates with HBV sAg + mothers
C: N/A |
|
|
Signs of cholecystitis on ultrasound |
-Stones / biliary sludge -Wall thickening (2-4mm) -Distension of GB (>4cm wide or 10cm long) -Pericholecystic fluid -Air in the GB wall (emphysematous or gangrenous cholecystitis) -Murphy's sign (sonographic) |
|
|
Treatment of hyponatremia with focal neurologic symptoms, seizure, or coma. Complication of rapid correction. |
Hypertonic (3%) saline 100mL over 10m then 100mL over the next hour (approximately 3mL/kg total)
After this aim to correct by 0.5mEq/L/h if chronic, 1mEq/L/h is okay if acute
Complication: central pontine myelinolysis |
|
|
Causes, diagnosis and treatment of SIADH |
Lung masses -Cancer, pneumonia, TB, abscess CNS disorders -Infection (meningitis, abscess), mass (subdural, postop, CVA) Drugs -Thiazides, narcotics, oral hypoglycemic agents, barbiturates, neoplastic agents, vasopressin
Diagnosis - low Sosm (<280), high Uosm (>100) with no other explanation
Treatment - water restriction, treat cause |
|
|
Causes of hypercalcemia and hypocalcemia |
Hypercalcemia -Increased intake (Ca supplements, milk-alkali) -Decreased losses (HCTZ) -Bone resorption (primary hyperparathyroidism, parathyroid-like hormone from small cell lung tumor, lytic bone lesions) -OD - estrogens, vitamin A, vitamin D, Lithium -Endocrine - hyperthyroid, adrenal insufficiency -Granulomatous disorders (activate macrophages that convert vit D to make active) - sarcoid, TB, coccidiomycosis, histoplasmosis
Hypocalcemia -Hypoparathyroidism (congenital, maternal, thyroid surgery) -Tox (EtOH, chemo) -Hyperphosphatemia, tumor-lysis syndrome |
|
|
Ca - symptoms and treatment of hypercalcemia and hypocalcemia |
Hypercalcemia -CNS - AMS, ataxia, fatigue -CVS - HTN, short QT, brady, STE -GI - N/V, anorexia, ileus, constipation -Renal - polyuria, dehydration, nephrolithiasis Treatment - IVF, zaledronic acid, calcitonin, steroids, lasix, underlying cause
Hypocalcemia -Neuromuscular - paresthesias, tetany (Chvostek's, Trousseau's) -CV - long QT, hypotension, brady, arrest -Resp - bronchspasm, laryngospasm -Psych/CNS - confusion, psychosis, dementia, depression, anxiety, irritability Treatment - asymptomatic CaCO3 1-4g/d po, stable CaGluc 10mL IV, unstable CaCl4 10mL IV |
|
|
Conditions that can cause a false positive lipase result (not pancreatitis) |
Many false positives at standard cutoff. Quite specific at 5x standard level, but down to 60% sensitivity. 2x cutoff is best for maximal sensitivity/specificity.
-Cholecystitis -Bowel obstruction -Peritonitis -Duodenal ulcer -DKA -Trauma -Post ERCP -Idiopathic |
|
|
x-ray and ultrasound findings of pancreatitis |
x-ray -Pleural effusion -Pancreatic calcification -Free air (? due to perf'd something) -Ileus -ARDS
Ultrasound -Occasionally can see CBD stone and/or enlarged hepatic duct (suggesting distal obstruction) |
|
|
Causes of simple and closed loop SBO |
Top 3: -Adhesions -Hernias -Cancer
Intrinsic - congenital, IBD, radiation enteritis, cancer, intussusception, hematoma
Extrinsic - hernias, adhesions, volvulus, compressing tumors, abscesses, hematomas
Intraluminal - FB, gallstones, bezoar, barium, ascaris |
|
|
X-ray signs of intussusception |
Crescent sign Target sign Abdominal mass (no air in one area - usually RUQ) / No liver edge sign Air fluid levels (SBO) Dilated loops of bowel (SBO)
NOTE: In adults (as opposed to children) you do not want to reduce this with enema as it is often caused by cancer and this can result in seeding |
|
|
X-ray signs of mechanical SBO, closed loop obstruction, ileus. Normal measurements of bowel. |
Mechanical -Dilated proximal loops and flattened distal loops -Sharply angulated or step-ladder loops of small bowel -Multiple air-fluid levels -'String of pearls' (pockets of gas trapped in the plicae semicircularis when the bowel is full of fluid)
Closed-loop -Coffee bean sign (U-shaped bowel loop also seen in sigmoid volvulus) -Pseudotumor sign (fluid filled loop resembling a mass)
Ileus -Dilated loops throughout the entire bowel including the colon -Dilation less prominent -Air fluid levels less prominent
Bowel measurements: -Small 3cm -Large 6cm -Cecum 9cm |
|
|
Causes of mesenteric ischemia and risk factors |
-Arterial embolism ~50% - mostly SMA (CAD, valvular disease, AF, aneurysms, dissections, coronary angiography) - needs embolectomy -Arterial thrombosis >15% - mostly SMA and have h/o abdominal angina (elderly, PVD, hypertension) - needs revascularization, heparin -Venous thrombosis <15% (same risk factors as DVT/hypercoaguability; Factor V Leiden most common) - needs heparain, thromboplasty -Non-occlusive - 20% (all shock states, cocaine, vasopressors; >50yo)
Lactate is highly sensitive CT angiography is most helpful diagnostic test; Angiography is gold standard and early angiography decreases death |
|
|
Modified Alverado score, WBC/CRP, U/S and CT for Appy |
Alverado score History: Migratory RLQ pain, Anorexia, N/V PE: T>37.5, RLQ tender (2 points), Rebound tenderness, Leukocytosis (2 points)
WBC<10 and CRP<12 have a -LR of 0.09 (very sensitive) but less helpful in peds.
U/S 75-95% sensitive, 85-95% specific - operator dependent but 1st choice for kids/women - see non-compressible, thick-walled (>2mm), dilated (>6mm), thickened mesentary, pain with compression, appendicolith
CT 95% sensitivity and specificity |
|
|
Rome III criteria for IBD |
Recurrent abdominal pain/discomfort for at least 3d in the past 3m associated with 2/3 of: -Improvement with defecation -Onset associated with a change in stool frequency -Onset associated with a change in stool appearance |
|
|
Causes of large bowel obstruction |
1 - Colorectal cancer 2 - Volvulus 3 - Diverticulitis 4 - Extrinsic compression from mets
Also: Abscess, stricture due to chronic ischemia, fecal impaction, IBD, CF, Hirschsprung's, body packers/stuffers, Ogilvie's (pseudo-obstruction) |
|
|
AXR findings of large bowel obstruction |
Distended colon Air-fluid levels Cecal dilation >12cm has increased risk of perforation |
|
|
Volvulus types, risk factors, x-ray findings |
Gastric: hiatal hernia, either between 40 and 50yo or <1yo. Often have diaphragmatic defects, gastric ulcer or cancer, adhesions, paralyzed diaphragm. Can't pass NG tube!!
Cecal: pregnancy, 'coffee bean sign' pointing to LUQ, also can have air-fluid levels in the small bowel, paucity of colonic gas. Treatment surgical.
Sigmoid: elderly, psych/neuro disease, institutionalized, constipation, high fiber diet, 'coffee bean sign' pointing to RUQ, bird's beak contrast. Treatment endoscopic detorsion or surgery. |
|
|
Crohn's versus colitis |
Crohn's affects mouth to anus / Colitis large colon and rectum only
Crohn's commonly found in terminal ileum and colon / Colitis starts at rectum and moves proximally
Crohn's is transmural / Colitis is superficial mucosa
Crohn's has skip lesions / Colitis is continuous
Crohn's gets primary sclerosing cholangitis / Colitis gets colon cancer |
|
|
Extra-intestinal manifestations of IBD |
ULCERATIVE U rinary stones L iver cirrhosis / sclerosing cholangitis C holelithiasis E rythema nodosum / erythema multiforme / pyoderma gangrenosum R etardation of growth A rthralgias / arthritis / ankylosing spondylitis T hrombophlebitis I atrogenic (steroids) V itamin deficiency E yes (uveitis, episcleritis)
Also pulmonary fibrosis |
|
|
Intestinal manifestations of IBD |
COLITIS C ancer O bstruction L eakage / perf I ron deficiency T oxic megacolon I nanition (wasting) S tricture
Also: abscess, fistula |
|
|
What is toxic megacolon? What causes it? What's the treatment? |
Inflammation of the smooth muscles of the colon leads to dilation and perforation if untreated. Patients look toxic and have dilated colon on AXR (>6cm).
Often due to infection (C Diff gets po vanco or po/iv flagyl; other gets ceftriaxone/flagyl), IBD (gets tazo and steroids), antimotility agents (anticholinergic or opioid - stop them). May need OR. |
|
|
What is required to prove negligence in a malpractice suit? |
-Health care provider has a duty of care -That duty of care is breached by breaking the standard of care -The patient is harmed -There is a direct link between the breach and the harm |
|
|
Mimics appendicitis Backpacker's diarrhea Raw/undercooked poultry Associated with GBS Diarrhea and seizures Associated with Reiter's Raw oysters/shellfish Prolonged diarrhea Dysentry without fever Fried rice GI and neuro Cold allodynia / hot/cold reversal Worse after EtOH ingestion Mayo/potato salad Eggs |
Mimics appendicitis: campylobacter and yersinia Backpacker's diarrhea: giardia lamblia, campylobacter Raw/undercooked poultry: campylobacter Associated with GBS: campylobacter Diarrhea and seizures: shigella Associated with Reiter's: salmonella Raw oysters/shellfish: vibrio parahemolyticus, plesiomonas Prolonged diarrhea: yersinia, aeromonas, parasite Dysentry without fever: e coli O157:H7 Fried rice: bacillus cereus (toxin mediated) GI and neuro: ciguatera toxin Cold allodynia / hot/cold reversal: ciguatera toxin Worse after EtOH ingestion: ciguatera toxin Mayo/potato salad: staph aureus Eggs: salmonella |
|
|
Bacterial causes of diarrhea; antibiotic treatment |
CSS Yalk Constantly - So Believe Every Child Vomiting And Pooping
C ampylobacter S higella - treat dysenteriae for public health S almonella - treat typhi and all food handlers for public health Y ersinia C lostridium jejuni S taph aureus (toxins) B acillus cereus (toxins) E coli (toxins) C difficile and perfringins (toxins) V ibrio cholera (toxins) and parahemolyticus A eromonas P lesiomonas
Toxin-producing generally do not respond to antibiotics
Antibiotics for severe infectious diarrhea with no evidence of HUS with cultures pending - children cefixime/azithro x 3-14d; adults cipro x 3-14d |
|
|
Causes of free fluid in the abdomen |
-Blood -Urine -Peritoneal dialysis fluid -Ascites > Liver disease - cirrhosis, alcoholic hepatitis, portal vein thrombosis, Budd-Chiari, liver mets (SAAG>11) > Abdominal or ovarian malignancies / carcinomatosis (SAAG<11) > TB peritonitis (SAAG<11) > Pancreatitis (SAAG<11) > Nephrotic syndrome (SAAG<11) > CHF > Hemodialysis |
|
|
Internal hemorrhoid classification and treatment |
1st degree - sense of fullness, no prolapse, medical management 2nd degree - prolapse during defecation and spontaneously reduce, medical management 3rd degree - prolapse spontaneously and during bowel movement, reduce spontaneously, medical or surgical management 4th degree - permanent prolapse with risk of thrombosis, surgical repair |
|
|
Medical and surgical hemorrhoid treatment |
Medical: WASH W arm water A nalgesia (topical nifedipine, lidocaine for external; internal controversial) S tool softeners H igh fiber diet
Surgical: sclerotherapy, hemorrhoidectomy, banding |
|
|
What is the anal fissure triad? Treatment? |
Deep ulcer Sentinal pile (hypertrophic edematous skin tag) Enlarged anal papilla
Treatment with WASH (warm water, analgesia with nitro/lidocaine/nifedepine, stool softeners, high fiber diet) as per hemorrhoids. |
|
|
Types of rectal abscess |
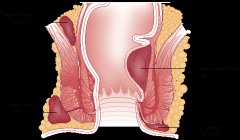
-Supralevator (high and deep) -Intersphincteric (internal, above pectinate line) -Ischiorectal (lateral; may be able to drain in ED - controversial) -Perianal and Perirectal (only ones we'd drain in ED)
Always tx with tetanus; Abx if DM/ immunocompromised/ valvular disease |
|
|
Causes of fecal incontinence |
Pediatric -Congenital (meningocele, myelomeningocele, spina bifida) -Post-op imperforate anus -Sexual abuse
-Neuro (demential, spinal cord injury, autonomic neuropathy from DM, pedental nerve damage from surgery/obstetrics, Hirshsprung's) -Trauma to sphincter -Mass (colorectal cancer, foreign body, hemorrhoids, fecal impaction) -Medical (rectal prolapse, diarrhea, IBD, laxatives) |
|
|
Gastroenteritis bugs that require treatment |
1) Culture positive, 2) immunocompromised, and 3) not improving
Also: -Shigella dysentariae (even if asymptomatic - public health) -Yersinia (even if asymptomatic - public health) -Salmonella typhi in food handlers, healthcare workers, severe colitis, <3m/o, >50yo -Bacillus anthracis -C difficile -Giardia Lambia -Entamoeba histolytica |
|
|
When can anti-diarrheal medications be given? |
AVOID in <2yo and those with fever or dysentery (blood +/- pus or mucous)
Consider in patients with severe symptoms along with antibiotics |
|
|
Diarrhea history - key questions |
Travel - parasites Antibiotics - c diff Ingestions - food poisoning Well-water - parasites Infectious contacts - virulent bacteria Pets at home - salmonella |
|
|
DDx for bilateral CNVII palsy |
Gosh, bilateral CNVII isn't just B2E2LLS3
GBS (Millar-Fischer variant) Ethylene glycol toxicity |
|
|
Characteristics of self-induced knife wounds |
-Multiple superficial incisions to trunk/arms/face -Multiple superficial stabs to trunk/arms/face -Parallel incisions on the non-dominant side of the body in close proximety to each other -Sparing of sensitive areas -Linear or curved incisions toward the hand inflicting the wound -Intact clothing covering the wound -Evidence of similar prior wounds |
|
|
Types of abuse |
3 categories: -Domestic -Institutional -Self
Multiple types -Physical -Emotional -Sexual -Neglect -Abandonment -Financial -Factitious disease (Munchausen's by proxy) |
|
|
Risk factors for child abuse |
Child -Premature -Difficult temperament -Developmental delay or chronic medical condition -Social isolation
Caregiver -EtOH or substance abuse*** -Abused as a child -Intimate partner violence -Mental illness -Single parent
Demographic -Low SES -Ethnic minority |
|
|
Shaken baby syndrome; imaging studies |
-Generally <1yo; can be <3yo -No evidence of impact -SDH and SAH -On fundoscopy see retinal hemorrhages (>75%), papilledema due to increased ICP
CT is better for SAH, imaging of intracranial injuries, easier to perform. MRI is better if subacute/chronic, deel cerebral injuries, extraaxial fluid, smaller SDH's |
|
|
Historical indicators of child abuse |
-Magical injuries -Inconsistent story -Inconsistent with childhood development (can't bruise if can't cruise; 3 week-old 'rolling' off of a table) -Unexplained delay in seeking care -History does not explain the injury |
|
|
Risk factors for HIV transmission via sexual intercourse |
Victim -Anal > vaginal -Coexisting STD's or genital lesions -Trauma evident -Ejaculate on mucous membranes -Cervical ectopy -Active menstration -Currently pregnant
Assailant -Foreskin -Primary infection -Late stage infection -Viral load in genital tract -STI's or genital lesions -Not on HAART -Multiple offenders -Incarcerated, homosexual, bisexual |
|
|
Risk factors for interpersonal violence |
Victim -Demographics (<35yo, female, immigrant, separated or divorced) -Environment (low SES, homeless, previous exposure to violent caretakers) -History (disabled, previous physical or sexual assault)
Perpetrator -Demographics (young) -Societal (low income, unemployed, low SES, low academic achievement, criminal behavior) -Psych (low self-esteem, personality disorder, emotional dependence, insecure) -Substance abuse -History (abused as a child, violence in family of origin, history of TBI) |
|
|
Medical problems on DDx with interperesonal violence |
-Depression, PTSD, suicidal ideation -Headaches -Stress-related illnesses -EtOH / substance abuse -Trauma in pregnancy -Chronic pain -STI/HIV |
|
|
Historical indicators of elder abuse |
Implausible mechanism of injury Inconsistent history between patient and caregiver Delay to presentation
Unexplained injuries Elder being called 'accident prone' Past history of frequent injuries
Noncompliance with meds, appointments, directions Caregiver does not know patient's history/meds Caregiver answers all questions Caregiver/patient reluctant to give answers
Strained patient/caregiver interactions Poor living situation |
|
|
Diagnostic criteria for a manic episode |
Manic episodes are characterized by a >2 week period with elevated/irritable mood and >3 of the following
GST PAID G randiosity S leep (decreased) T alkative
P leasurable activities / P ainful consequences A ctivity I deas (flight of) D istractable
Is not mixed, causes marked impairment or requires hospitalization, not due to a general medical condition. |
|
|
Anxiety definitions: Anxiety, Panic attack, Agoraphobia, Social phobia, Phobia, OCD, Generalized anxiety, PTSD, acute stress disorder |
-Anxiety: a specific unpleasurable state of tension that forewarns the presence of danger (uneasiness stems from the anticipation of some imminent danger, the source of which is unknown or unrecognized)
-Panic attack: discrete period of sudden onset of intense apprehension, often associated with feelings of impending doom
-Agoraphobia: Anxiety about place or situations from which escape might be difficult (fear of being along in public places).
-Panic disorder with agoraphobia: Pts have recurrent unexpected panic attack and become fearful of situations where they might occur
-Specific phobia: irrational fear of something that is perceived as dangerous (normal in children)
-Social phobia: anxiety d/t social or performance situations
-Obsessive-Compulsive Disorder: Obsessions → stress or anxiety which is relieved by a compulsive behaviour
-Generalized anxiety disorder: persistent, excessive anxiety or worry for > 6 months
-Post-traumatic stress disorder: Heightened arousal and avoidance of stimulus following a significant traumatic exposure
-Acute stress disorder: similar to PTSD occurring immediately in the aftermath of an extremely traumatic event |
|
|
Predictors of organic anxiety disorders |
Predictors -Onset after 35yo -Lack of childhood, personal, or family history of anxiety/phobias -Lack of avoidance behavior -Absence of live events that would exacerbate anxiety -Poor response to anxiolyticsiD |
|
|
Disorders that can manifest as anxiety |
Substance abuse: sympathomimetics (caffeine, amphetamine, cocaine), hallucinogens (LSD, PCP, Ecstasy, marijuana) Withdrawl: depressants (benzos, barbiturates, EtOH) Cardiac: arrhythmias, mitral valve prolapse Endocrine: hypo/hyperthyroid, hypoglycemia, pheochromocytoma, hyperadrenocortism Resp: asthma, PE Medications: alpha agonists, theophylline, corticosteroids, thyroid hormone |
|
|
What is somatization disorder? |
Somatization disorder -Unexplained physical symptoms beginning before 30yo -At least 4 sites of pain, 2 GI symptoms, 1 reproductive/sexual symptom, 1 neurologic symptom -Not explained by another medical condition -Not intentionally feigned/produced
Risk factors -Women, low SES, alcoholism, addictions, poor education, interpersonal problems |
|
|
What is conversion disorder? |
-A somatoform disorder -Sudden onset of a single symptom not under the patient's control and often associated with la belle indifference -Generally neurological (motor: tremors, paralysis, pseudoseizures, aphonia, ataxia; sensory: anesthesia, blindness, tunnel vision) -Often a psychiatric coping mechanism |
|
|
What is somatization? List the somatoform disorders. |
Somatization The unconscious experience and communication of psychological distress through physical symptoms.
-Somatization disorder -Conversion disorder -Pain disorder -Hypochondriasis |
|
|
What is hypochondriasis? DDx for it? Treatment? |
4 key features: -Symptoms are more than the organic disease that is evident -Fear of disease and conviction that one is sick -Preoccupied with their body -Persistent and unsatisfying pursuit of medical care
DDx -Endocrine (hyperparathyroid, thyroid disorders, Addison's, insulinoma, panhypuitarism), MS, porphyria, Lupus, Wilson's disease, Myesthenia Gravis, GBS, Uremia
Treatment -Reassurance, legitimize, share diagnostic uncertianty, assure ongoing care, avoid drugs that cause dependency, come up with realistic treatment goals focused on symptom control, arrange single-physician follow-up |
|
|
Compare factitious disorder, Munchausen's Syndrome, Munchausen's syndrome by proxy, Malingering, |
Factitious disorder: symptoms and signs produced or feigned in the absence of external symptoms to take on the sick role, IS a mental disorder, unmarried educated women <40yo with healthcare background.
Munchausen's: a form of factitious disorder, wide variety of illnesses with intent of gaining hospital admission, hospital shoppers, believe they are very important, initially praise care -> become disruptive -> rage and AMA
Munchausen's by proxy: a form of factitious disorder where illness produced/feigned in a child. Persistent presentations with symptoms that stop when perperator is removed. Parents work in healthcare. Notify protective services and consult psych for mother.
Malingering: Malingerers ARE motivated by external incentives! Assume somatization unless otherwise proven. Often medicolegal context, discrepancy between findings and disability, poor cooperation, antisocial behavior. Don't want to get better; gaming the system. |
|
|
Diagnosis of schizophrenia |
>2 of these symptoms for >1 month -Delusions (if delusions bizarre counts as 2) -Hallucinations (if running commentary counts as 2) -Disorganized speech -Disorganized or catatonic behavior -Negative features (avolition, poverty of speech, flat affect)
As well as: -Sharp deterioration -Disturbance for >6 months (with prodrome) -Other causes ruled out |
|
|
Complications of neuroleptic use and treatment |
-Orthostatic hypotension - alpha blockade, give fluids -Acute dystonia - cholinergic, treat with anticholinergic benztropine (cogentin) 1-2mg IV/IM +/- benadryl -Akathisia - motor restlessness, decrease dose or try beta-blocker -Parkinsonism - can be indistinguishable from Parkinson's, tends to resolve over time, decrease dose or start parkinson's meds -Tardive dyskinesia - occurs over years, bad, choreathetoid movements (tongue, grimace, writhing), no known treatments, try switching to atypical or benzo's -NMS |
|
|
Symptoms (in order) of NMS, medications that cause it, treatment |
MR HA altered M ental status (agitated or catatonic) R igidity (lead pipe, tremor) H yperthermia A utonomic instability
Medications: typical and atypical antipsychotics, lithium, Parkinson's medications, maxeran
Treatment: Benzo's, stop neuroleptics, bromocriptine/dantroline/amantidine, cool, ICU, electroconvulsive therapy (Seriously? Seriously??) |
|
|
Simple vs complex skull fracture |
Simple: -Linear not crossing suture lines -<2mm of separation
Complex: -Linear crossing suture lines ->2mm of separation -Stellate -Comminuted -Depressed -Compound -Diastatic |
|
|
Triad of shaken baby syndrome |
-Subdural hematoma -Cerebral edema -Retinal hemorrhages |
|
|
DDx for retinal hemorrhages |
-Vaginal delivery (resolve in 10-14 days) -Bleeding disorders -AV malformations -Meningitis -Severe accidental head injury |
|
|
Physical exam signs of sexual abuse |
-Unexplained vulvar bruising -Hemorrhage -Hymenal or vulvar tears -Loss of hymen out to the margin of the vagina -Signs of STI's (gonorrhea, chlamydia, hsv2, syphilis, trichomonas)
Can get HPV, HSV1, Gardnerella vaginosis, Hepatitis B/D and AIDS without assault. |
|
|
Bronchiolitis treatments |
-Oxygen - yes if hypoxic
-IVF - yes if dehydrated
-Beta agonists - not generally recommended (perhaps 10% responders, atopic people more likely)
-Steroids - no
-Epinephrine - some bad evidence that it can help prevent hospitalization, but not enough evidence to use it
-Epi and steroids together - may be a synergistic response, but more evidence needed. NOT recommended.
-Nebulized hypertonic saline - evidence moving towards its use, but it is still not in the guidelines |
|
|
Inadequate view of prevertebral soft tissue in children |
-View taken on EXpiration -Flexed or neutral (rather than extended) neck |
|
|
Esophageal button battery - mechanisms of injury |
-Current from the battery forming a circuit -Release of hydroxide -Pressure necrosis due to esophageal foreign body |
|
|
What are the goals / indications of PSA? |
Analgesia Anxiolysis Sedation Immobility Amnesia |
|
|
Crisis vs psychiatric emergency |
Crisis: acute emotional upset arising from situational or developmental problems that results in temporary inability to cope
Psychiatric emergency: acute behavioral disturbance related to severe mental or emotional instability or dysfunction requiring medical intervention |
|
|
HEADSS social history |
H ome E ducation A fter school D rugs S exual history S uicidal thoughts/attempts |
|
|
Mental status exam |
Appearance Attitude Behavior Mood Affect (appropriateness, lability, eye contact) Orientation (date/time/place) Speech Thought process (disorganized) Thought content (delusions) Perceptions (hallucinations) Cognition (memory, content of thought, preoccupations, coherent speech, ability to reason, insight, judgement) Insight Judgement Suicidal ideation Homicidal ideation Capacity (CURVES)
|
|
|
Substance dependence |
WITHDraw IT
W ithdrawal I nterest or Important activities neglected T olerance H arm to physical and psychosocial are known but they continue to use D esire to cut down, control it
I ntended time, amount exceeded T ime spent too much |
|
|
Pediatric vs adult bones |
-Thicker and more stable periosteum -Faster healing with less immobilization -Better remodeling capability and vascularity -Growth plates weaker than ligaments -More porous and pliable |
|
|
Toddler's fracture characteristics |
-Minimal or no history of trauma -Red flags for NAT are: more transverse fracture with an associated fibular injury -Generally 9m to 3y of age -On physical exam spiral oblique axial load provokes pain (put axial load and twist ankle) -Generally treat with an above knee backslab - sometimes don't need anything. |
|
|
Seven pulmonary complications of pneumonia |
-Pleural effusion / empyema -Pneumothorax -Lung abscess -Bronchopleural fistula -Necrotizing pneumonia -Pneumatocele -Acute respiratory failure |
|
|
How long are these pediatric rashes congagious for? (varicella, rubella, measles, parvovirus) |
-Varicella - 2 days before until lesions are all crusted over -Rubella - 1-2 weeks before they present with rash -Measles - 5 days before and 4 days after -Parvovirus - a week before until the rash starts |

