![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
|
General series of events in theriogenology
|
-mature from birth to puberty
--hormonal control of development of oocyte and sperm ---sexual behavior to induce the joining of oocyte and sperm ----fertilization -----recognition and maintenance of pregnancy ------parturition -------lactation and care of young |
|
|
Hypothalamus
-hormones |
-GnRH
|
|
|
GnRH
-function |
-bind to gonadotrophs in the anterior pituitary release of LH & FSH
|
|
|
GnRH agonists (Rx)
|
-Cystorelin
-Factrel -Fertagyl |
|
|
GnRH agonists
-uses |
-initiate ovulation (estrous synchronization of cattle)
-treat polycystic ovarian disease -reduce fertility in wild animals |
|
|
GnRH control
|
Gonadal steroids
-estrogen -androgens -progesterone |
|
|
GnRH control
-Rx |
-Mebolerone (synthetic androgen for estrus prevention in adult female dogs)
|
|
|
GnRH travels to the anterior pituitary via
|
-portal vessels
|
|
|
LH
-function |
-convert follicular cells to luteal cells
-maturation of tertiary follicles and stimulates estrogen production stimulates androgen synthesis by thecal cells |
|
|
LH surge
-function |
-inc. progesterone conc. in follicular fluid
-reactivate myosis of primary oocyte -inc. estradiol, PGF2a, PGE2 |
|
|
LH
-effect in male |
-stimulation of Leydig cells of testes to produce testosterone
|
|
|
Chorionic gonadotropin
-types & effects |
-eCG (equine): LH and FSH
-hCG (human): LH |
|
|
Action of GnRH or eCG
|
Release of LH
-ovulation/luteinization -initiation of new follicular wave -CL formation |
|
|
FSH
-function |
-stimulate follicle growth in ovaries
-stimulates estradiol production from granulosa cells of follicle |
|
|
FSH
-half life |
-several hours
-longer than LH (10 min) |
|
|
Prolactin
-produced where |
-anterior pituitary
-immune cells -brain -uterus -others |
|
|
Prolactin
-function |
-acts with estrogens to induce lobuloalveolar growth of mammary glands
-stimulate milk production -maintain CL in some species (dog, rodent) -maternal behavior (nesting) |
|
|
Prolactin
-release antagonized by |
-dopamine from hypothalamus
|
|
|
Oxytocin
-produced where |
-hypothalamus and secreted by nerve ending in the posterior pituitary
|
|
|
Oxytocin
-function |
Smooth muscle contraction
-eject milk from mammary alveoli (released from tactile stimulation of teats) -inc. uterine contractions during parturition (rise in estrogen increases the number of oxytocin receptors in myometrium) -establish maternal behavior (rodents) -facilitate sperm transport (male and female tracts) |
|
|
Oxytocin
-Rx -use |
-Pitocin
-Oxytocin -uterine contractor to precipitate and accelerate normal parturition and postpartum evacuation of uterine debris -use post cesarean section to facilitate involution and resistance to large inflow of blood -help with milk letdown |
|
|
Your client want to "superovulate" a female so that she produces more eggs than normal. What hormone should you give?
|
-FSH
|
|
|
How do the hypothalamic hormones reach the anterior pituitary gland?
|
-short portal vessels
|
|
|
Ovarian Follicle
-hormone secreted |
-Estrogen
|
|
|
Estrogen
-function |
-positive feedback loop with LH
-acts on the brain to initiate estrous |
|

|
Ovarian follicle
|
|
|
When can primary follicles start becoming secondary follicles?
|
-puberty
|
|
|
Pituitary dependent phase of follicular growth
-describe |
-FSH
-growing follicles are stimulated to undergo further growth and maturation -increased number of granulosa cells -liquor folliculi moves between granulosa cells |
|
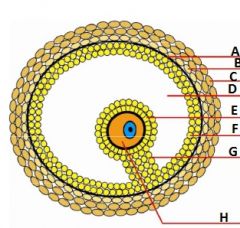
-follicle type
-letters |
Graafian follicle
-A: basal lamina -B: theca interna -C: theca externa -D: antrum filled with follicular fluid -E: corona radiata (after ovulation) -F: granulosa cells -G: cumulus oophorus -H: primary oocyte (mare, dog); secondary oocyte (other species) |
|
|
Progesterone
-produced where |
-granulosa cells
-theca cells |
|
|
Intrafollicular progesterone
-precursor for |
-testosterone
-estrogen |
|
|
Steroid hormone production from cholesterol
-flow -produced from |
-cholesterol
--progesterone ---testosterone ----estrogen -cholesterol from liver -hormones from adrenal glands and gonads |
|
|
PGF2a
-produced where |
-uterus
-non-pregnant endometrium |
|
|
PGF2a
-function |
-lyse CL
-initiate process to ovulation |
|
|
PGF2a
-Rx |
-Lutalyse
-Estrumate |
|
|
PGF2a
-reason to use |
-lyse a mature CL (diestrus) causing a decline in progesterone production by the CL
|
|
|
PGF2a
-side effects in horses |
-sweating
-colic -trembling |
|
|
Induced ovulator
-definition |
-require stimulation in order to ovulate (copulation, genital stimulation)
|
|
|
Induced ovulator
-example spp |
-rabbit
-cat -camel -ferret |
|
|
Hormonal effect of copulation in a queen
|
-copulation stimulated LH secretion by anterior pituitary
-more copulations-->higher LH |
|
|
Progesterone
-produced where |
-CL
|
|
|
Progesterone
-function |
-prepare the uterus for the egg
-acts on the brain to override estrogen and prevent estrus behavior |
|
|
Progesterone
-Rx |
-Melengestrol acetate
-Regu-Mate -CIDR insert (natural) |
|
|
Why you rely on the fact that estrus behavior is not being seen to know if there has been ovulation?
|
-more progesterone is needed to prevent ovulation than is needed to prevent estrus
|
|

|
-Corpus luteum
|
|
|
Graafian follicle
-what is it |
-large tertiary follicle that is ready to ovulate
|
|
|
Testosterone
-formed where |
-Leydig cells in the interstitial spaces of the testis
|
|
|
Testosterone
-conversion from cholesterol stimulated by |
-LH
|
|
|
LH
-inhibited by |
-estrogen
|
|
|
Hormone necessary for male farm animals to reach puberty
|
-LH
|
|
|
Hormones required for the induction of spermatogenesis during puberty
|
-FSH
-LH |
|
|
Functions of LH and FSH in inducing spermatogenesis
|
-LH stimulated testosterone production
--testosterone stimulates sertoli cells -FSH decreases percentage of germ cells that degenerate during spermatogenesis |
|
|
Can spermatogenesis be sped up?
|
-NO
|
|
|
Spermatogonia
-chromosome number |
-diploid (2n)
|
|
|
Spermatogonia
-effect of mitosis -effect of meiosis |
Mitosis
-more spermatogonia Meiosis -differentiation to spermatocytes --> 4 haploid spermatids |
|
|
Length of time for spermatocytes to become spermatids
|
-3 wks
|
|
|
Length of time for spermatids to differentiate to sperm
|
-3 weeks
|
|
|
Importance of progesterone produced by placenta
|
-if enough progesterone is produced by the placenta, a CL is not needed to maintain pregnancy
-human -sheep -cat |
|
|
Progesterone
-roles |
-support endometrium for fetal survival
-suppress contractility of uterine smooth muscle -inhibit LH & FSH --> prevents ovulation during pregnancy |
|
|
Estrogen production by placenta
-function |
-prepare uterus for fetal expulsion (block progesterone)
-stimulate mammary gland development |
|
|
Placental estrogens
-derived from |
Depends on spp:
-fetal androgens -placental progestins -steroid precursors |
|
|
Chorionic gonadotropins
-function |
-invade maternal tissues and act similar to LH/FSH (pituitary gonadotropins)
|
|
|
hCG
-function |
Human Chorionic Gonadotropin
-binds to LH receptros preventing CL regression |
|
|
Chorionic gonadotropins
-species found in |
-humans
-equine |
|
|
Placental lactogen
-function |
-relative of prolactin and oxytocin
-development of mammary gland prior to parturition -stimulate CL function |
|
|
Placental lactogen
-species found in |
-primates
-ruminants -rodents |
|
|
Relaxin
-function |
-maintain pregnancy
-relaxation of pelvic ligaments at end of gestation |
|
|
Relaxin
-produced where |
-placenta
-CL -both |
|
|
Relaxin
-species that can produce a lot of hormone |
-Guinea pigs (large babies)
|
|
|
What type of hormones are orally active?
|
-steroid hormones
-protein hormones get digested |
|
|
Which species can maintain a pregnancy even if an ovariectomy is performed?
|
-sheep
|

