![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
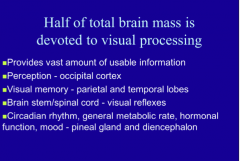
What cortex creates perception? Visual memory? (which lobes) Visual reflexes? What controls circadian rhythm, general metabolic rate, hormonal function, mood?
|
|
|
|
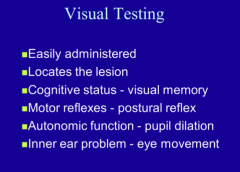
How can you check visual memory? Autonomic function? Inner ear problem? |
|
|
|
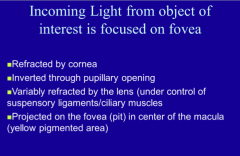
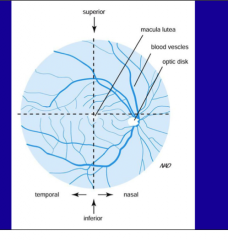
What is incoming light from the object of interest focused on? What is it refracted by? How is it variably refracted? Projected onto what in the center of the macula? |
|
|
|
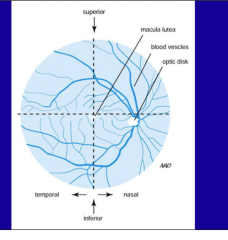
Where is the fovea? |
At the center of the macula of the eye |
|
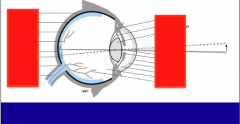
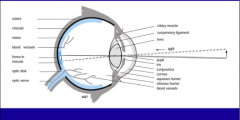
Identify: Sclera, choroid, retina, blood vessels, fovea in macula, optic disk, optic nerve, ciliar muscle, suspensory ligament, lens, light, pupil, iris, conjunctiva, cornea, aqueous humor, virtreous humor, blood vessels |
|
|
|
What is the purpose of sclera, choroid? What maintain visual axis on fovea? |
|
|
|
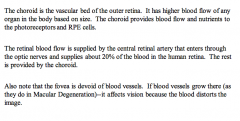
What is retinal blood flow provided by (20%)? What is the rest provided by?
Are there blood vessels in the fovea? What is if called if blood vessels grow there? |
|
|
|
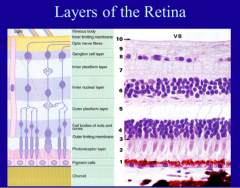
List the layers of the retina.
|
|
|
|
What do the RPE cells do? Where are the cell bodies of photoreceptors located? Where do their projections lie? Where do they signal through?
What is the final layer of neurons in the retina? |
The pigment cells are the retinal pigmented epithelial cells (RPE). They provide a barrier to the retina from the choroid. Photoreceptors (cones and rods--named based on their shape) come in contact with the RPE. The cell bodies of the photoreceptors are located in the outer nuclear layer, while their projections lie in the outer plexiform layer. The photoreceptors signal through the outer plexiform layer to the bipolar cells, whose cell bodies are in the inner nuclear layer. The final layer of neurons in the retina are retinal ganglion cells (located in the ganglion cell layer). Once the visual object is transduced to the retinal ganglion cells, it will enter into the optic nerve and go to the brain. |
|
Review |
|
|
|
What neurons help in convergence of the image from the millions of photoreceptors to hundreds of bipolar cells to tens of ganglion cells? |
Interneurons (horizontal cells and amacrine cells) help in convergence of the image from the millions of photoreceptors to hundreds of bipolar cells to tens of ganglion cells. Ultimately--the image will be sent through the ganglion cells to the optic nerve (optic nerve entry into the retina is the blind spot) In the fovea, the outer segments are present, but the rest of the retinal layers are displaced radially to allow for minimal distortion of the image. |
|
|
What is the layer that separates choroid (vascular) from retina (neural)? What pigment does it contain?
What are some functions? |
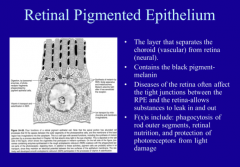
Main function = separation 2nd main function = eat rod outer segments every 10 days (becomes less effective as we age) |
|
|
Specific layers of the retina Macular degeneration results when blood vessels damage the RPE and break through their barrier and grow into the macular region of the eye. Causes visual distortion of the image. The 2nd main function of the RPE is to eat rod outer segments every 10 days. As we age--this becomes less effective. More proteins are left in the RPE, which can cause them to autofluoresce. This autofluorescence is called drusen and is a key factor in dry macular degeneration. The melanin in the RPE help absorb some of the light that comes to the photoreceptors. When this absorption is reduced (blue-eyed people vs. brown eyed people), some think this may contribute to eye disease. |
Specific layers of the retina Macular degeneration results when blood vessels damage the RPE and break through their barrier and grow into the macular region of the eye. Causes visual distortion of the image. The 2nd main function of the RPE is to eat rod outer segments every 10 days. As we age--this becomes less effective. More proteins are left in the RPE, which can cause them to autofluoresce. This autofluorescence is called drusen and is a key factor in dry macular degeneration. The melanin in the RPE help absorb some of the light that comes to the photoreceptors. When this absorption is reduced (blue-eyed people vs. brown eyed people), some think this may contribute to eye disease. |
|
|
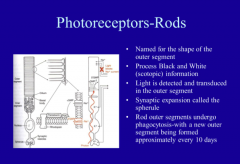
What do rods process? Where it light detected and transduced? What is synaptic expansion called? What do rod outer segments undergo every 10 days? |
|
|
|
What do cones process? What are the three types and the wavelengths associated with each? |
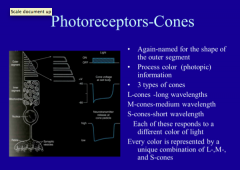
|
|
|
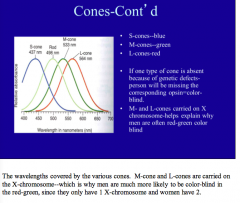
What color does each detect? S cones, M cones, L cones?
What will be the effect if one type of cone is absent?
What chromosome carries M and L cones? |
|
|
|
What is the purpose of photoreceptors?
What do both cones and rods undergo in response to light?
|
|
|
|
What is the pathway of visual phototransduction in rods? |
Light comes in => converts 11-cis-retinal to all-trans retinal => activation of rhodopsin (rod opsin) => GTP activated => activation of cGMP PDE => lowers cGMP enough to hyper polarize membrane and close sodium and calcium channels => VISUAL RESPONSE
Sodium and calcium accumulate in membrane => Ca2+ pumped out through exchanger => cGMP levels rise and depolarize membrane to pre-stimulus levels which re-opens channel
Rhodopsin dephosphorylated slowly => all-trans-retinal converted to 11-cis-retinal
Rhodopsin kinase re-phosphorylates rhodopsin => bound by arrestin to make inactive. If light stimulus occurs => arrestin removed by conversion of 11-cis-retinal to all-trans-retinal |
|
|
Where does phototransduction occur? |
Rods |
|
|
|
|
|
Where is the signal passed once photoreceptors have processed light?
Where to rod photoreceptors transduce their signal to?
What cells help converge the signals from multiple rod photoreceptors to fewer rod bipolar cells? |
|
|
|
What type of ganglion cells predominant in the peripheral retina - receive most input from the rods? Where do they project? |
|
|
|
Where are beta-ganglion cells found? Where do they project? What are they responsive to? |
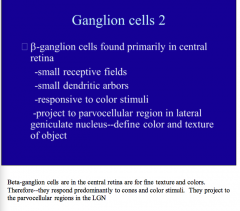
|
|
|
Why does the rest of the signaling pathway (bipolar cells, ganglion cells) project radially away from the fovea? |
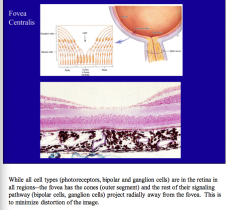
|
|
|
Does convergence occur in the fovea? |
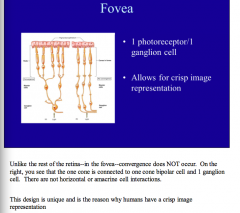
|
|
Review |
|
|
|
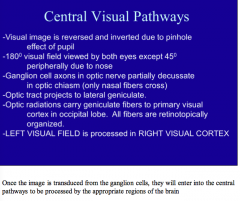
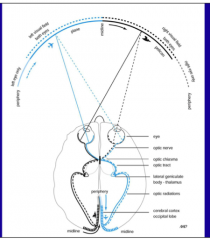
Why is the visual image reversed and inverted?
Where do ganglion cell axons decussate? Where do optic tracts project? Where do optic radiations carry geniculate fibers? Where is the left visual field processed? |
|
|
Review |
|
|
|
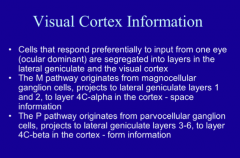
Where does the M pathway originate and project to? What type of information?
Where does the P pathway originate and project to? What type of information? |
|
|
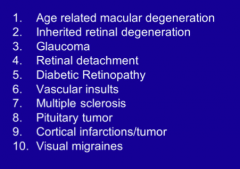
What are all of these? |
Vision related diseases |
|
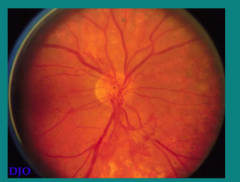
What disease does this patient have?
What are the light spots at the bottom of the image?
What is happening in the inferior region below the optic disc? |
Proliferative diabetic retinopathy
Blood vessel is damaged => edema occurring |
|
|
What are two major changes of DR? |
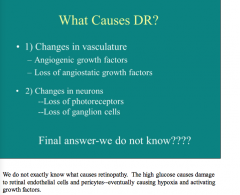
|
|
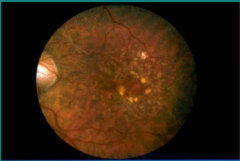
What is shown here? |
A retinal image of a patient with macular degeneration
Hyperfluorescence and areas of non vascularity |
|
|
Compare AMD and DR:
Which involves choroid NV, retina NV? Which is age induced? No age effect? Which have some genetic components? Which loses all vision? Lose central vision? |
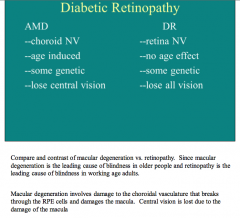
|
|
|
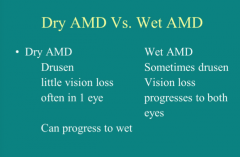
What are the two types of macular degeneration?
Which type sometimes has drusen, has vision loss, and progresses to both eyes? |
|
|
|
There are 2 types of macular degeneration. Normally all people have a little drusen. When a patient has abnormal amounts of drusen and begins to lose vision--often in 1 eye--it is termed _____ macular degeneration or atrophic macular degeneration. This represents about ____% of the cases of macular degeneration. With visual aids, these people can continue to function In the wet form (__% of cases)--the blood vessels grow into the macula and cause significant vision loss. |
There are 2 types of macular degeneration. Normally all people have a little drusen. When a patient has abnormal amounts of drusen and begins to lose vision--often in 1 eye--it is termed dry macular degeneration or atrophic macular degeneration. This represents about 90% of the cases of macular degeneration. With visual aids, these people can continue to function In the wet form (10% of cases)--the blood vessels grow into the macula and cause significant vision loss. |
|
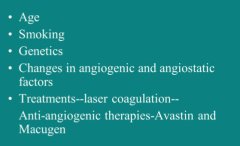
What are these all causes of? |
AMD Biggest cause is age
The biggest cause of AMD is age. Smoking is also a big contributor. Some new research has shown some genetic predisposition due to altered inflammatory responses. In the last 5 years--patients with AMD have hope. Using intravitreal injections (about monthly)--they can get a drug that blocks the vascular growth. It does not restore vision in most patients, but it often helps them maintain what vision they have. Eventually they will still lose vision, but the drugs are much better than previous options. |

