![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is incisura terminalis |
Area between crus of helix and Tragus which doesn't have cartilage. |
|
|
|
What can be used for reconstructive surgery of middle ear? |
1. Cartilage from tragus 2. Perichondrium from Tragus and concha 3. Fat from lobule |
|
|
|
Dimensions of External auditory canal |
1. 24 mm along it's post wall 2. Cartilagenous part: 8mm (outer 1/3rd) 3. Bony part: 16 mm (inner 2/3rd) 4. Isthmus: 6mm lateral to tympanic membrane |
|
|
|
Glands secreting wax |
1. Ceruminous 2. Pilosebaceous |
|
|
|
Name of deficiencies |
Fissures of santorini |
|
|
|
Where are furuncles formed and why |
Hair is confined only to the outer 1/3rd of canal, hence staph infections are seen only here |
|
|
|
Work of Anterior recess |
Acts as a cesspool for discharge and debris in case of infections |
|
|
|
Location of anterior recess |
Beyond isthmus, anteroinferior part of deep meatus |
|
|
|
Deficiency in anteroinferior part of bony canal |
Foramen of Huschke |
|
|
|
Dimensions of tympanic membrane |
1. 9-10 mm long 2. 8-9 mm wide 3. 0.1 mm thick |
|
|
|
Name of fibrocartlilagenous ring |
Annulus tympanicus |
|
|
|
What is Umbo? |
Central part of pars tensa tented inwards at level of tip of malleus |
|
|
|
Another name of pars flaccida |
Shrapnell's membrane |
|
|
|
Superior relation of EAC |
Middle cranial fossa |
|
|
|
Posterior relation of EAC |
1. Mastoid air cells 2. Facial nerve |
|
|
|
Inferior relation of EAC |
Parotid gland |
|
|
|
Anterior relation of EAC |
TMJ |
|
|
|
When and where is sagging seen? |
Seen in posterosuperior part of deeper canal Noticed in acute mastoiditis |
|
|
|
Nerve supply of pinna |
1. Greater auricular 2. Lesser occipital 3. Auriculotemporal 4. Auricular branch of vagus 5. Facial nerve |
|
|
|
Other name of auricular branch of vagus nerve |
Arnold's nerve Supplies concha and corresponding eminence |
|
|
|
Nerve supply of EAC |
1. Auriculotemporal 2. Auricular branch of vagus 3. Sensory fibres of (2) |
|
|
|
Nerve supply of tympanic membrane |
1. Auriculotemporal nerve 2. Auricular branch of vagus 3. Tympanic branch of vagus (Jacobson's nerve) |
|
|
|
Constituents of middle ear cleft |
Middle ear Eustachian tube Aditus Antrum Mastoid air cells |
|
|
|
Location of mesotympanum |

Opposite to pars tensa |
|
|
|
Location of epitympanum (attic) |

Above pars tensa but medial to Shrapnell's membrane |
|
|
|
Location of hypotympanum |

Below the pars tensa |
|
|
|
Roof and floor of middle ear |
Roof- tegmen tympani: separates TM from middle cranial fossa Floor- thin plate of bone : separates TM from jugular bulb |
|
|
|
Anterior wall of middle ear |
Thin plate of bone : separates cavity from Internal carotid artery Two openings: 1. Upper one: canal for tensor tympani muscle 2. Lower one: Eustachian tube |
|
|
|
Posterior wall of middle ear |
Lies close to mastoid air cells Bony projection : Pyramid Through the summit appears tendon of stapedius to get attached to neck of Stapes. |
|
|
|
Pyramid of middle ear |
Superior: aditus Posterior: facial nerve Depression in posterial wall lateral to pyramid: Facial recess/posterior sinus Medial: Vertical part of 7th nerve Lateral: Chorda tympani Above: Fossa incudis |
|
|
|
Surgical importance of facial recess |
Direct access can be made through this to middle ear without disturbing posterior wall |
|
|
|
Medial wall of middle ear |
Formed by labyrinth Bulge: promotory Oval window Round window |
|
|
|
Oval window |
Attached to the footplate of stapes Above oval window: Canal for facial nerve (Above this canal: Prominence of lateral semicircular canal) Anterior to oval window: Processus cochleariformis |
|
|
|
Importance of Processus cochleariformis |
Marks the level of the first genu of the facial nerve which is an important landmark for surgery of the facial nerve. |
|
|
|
Sinus tympani |
It is medial to pyramid bounded by the subiculum below and the ponticulus above |
|
|
|
Lateral wall of middle ear |
Formed largely by the tympanic membrane and to a lesser extent by the bony outer attic wall called scutum. |

|
|
|
What is a scutum |
Bony outer attic wall is called scutum. |
|
|
|
Boundaries of mastoid antrum |
Roof- tegmen antri (separates from middle cranial fossa) Laterally- 1.5 cm thick plate of bone Marked externally on surface of mastoid by Mac Ewen's (supremeatal) triangle |

|
|
|
Different types of mastoid |
Depending on development of air: 1. Well-Pneumatized or Cellular 2. Diploetic 3. Sclerotic or acellular |
|
|
|
Different type of mastoid 2 |
Depending on the location 1. Zygomatic cells 2. Tegmen cells 3. Perisinus 4. Reterofacial 5. Perilabyrinthe 6. Peritubular 7. Tip 8. Marginal 9. Squamosal |
|
|
|
What is Korner's septum? |
Mastoid develops from petrous and squamous bones. The petrosquamosal suture may persist as bony plate, separating superficial squamousal cells from deep petrosal cells - called as Korner's septum |
|
|
|
Surgically importance of Korner's septum |
Korner’s septum is surgically important as it may cause difficulty in locating the antrum and the deeper cells; and thus may lead to incomplete removal of disease at mastoidectomy. Mastoid antrum cannot be reached unless the Korner’s septum has been removed. |
|
|
|
Inferior route for draining petrous apex |
Inferior- most common Approach through: 1. Infralabyrinthine- Access is through mastoid. 2. Infracochlear- Access is through the ear canal. |
|
|
|
Footplate of Stapes is held by |
Annular ligament in oval window |
|
|
|
Intratympanic muscles |
1. Tensor tympani 2. Stapedius |
|
|
|
Attachments of Intratympanic muscles |
1. Tensor tympani attaches to the neck of malleus and tenses the tympanic membrane. 2. Stapedius- attaches to the neck of stapes and helps to dampen very loud sounds thus preventing noise trauma to the inner ear. |
|
|
|
Nerve supply of Intratympanic muscles |
Tensor tympani- develops from 1st arch Supplied by branch of mandibular nerve (V3). Stapedius- develops from 2nd arch Supplied by branch of CN VII |
|
|
|
Tympanic plexus is formed by |
Lies on promontory (i) Tympanic branch of glossopharyngeal. (ii) Sympathetic fibres from the plexus round the internal carotid artery. |
|
|
|
What does tympanic plexus supply |
Innervation to the medial surface of the tympanic membrane, tympanic cavity, mastoid air cells and the bony eustachian tube. It also carries secretomotor fibres for the parotid gland. |
|
|
|
Course of secretomotor fibres of tympanic plexus to the parotid: |
Inferior salivary nucleus → CN IX → Tympanic branch → Tympanic plexus → Lesser petrosal nerve → Otic ganglion → Auriculotemporal nerve → Parotid gland. |
|
|
|
Chorda tympani nerve |
Carries taste from anterior two-thirds of tongue and supplies secretomotor fibres to the submaxillary and sublingual salivary glands. |
|
|
|
Lining of Eustachian tube |
Pseudostratified columnar- Cartilagenous part Columnar- Bony part It is lined by ciliated epithelium. |
|
|
|
Lining of Tympanic membrane |
Anterior and inferior- ciliated columnar Posterior part- cuboidal |
|
|
|
Lining of epitympanum and mastoid air cells |
Flat, non-ciliated epithelium |
|
|
|
Major Blood supply of middle ear |
1. Anterior tympanic branch of maxillary artery - which supplies tympanic membrane. 2. Stylomastoid branch of posterior auricular artery - which supplies middle ear and mastoid air cells. |
|
|
|
Minor blood supply of tympanic membrane |
1. Petrosal branch of middle meningeal artery. 2. Superior tympanic branch of middle meningeal artery. 3. Branch of artery of pterygoid canal. 4. Tympanic branch of internal carotid. |
|
|
|
Where do veins supplying middle ear drain into? |
Pterygoid venous plexus Superior petrosal sinus |
|
|
|
Lymphatic drainage of middle ear |

|
|
|
|
Recesses in vestibule of bony labyrinth |
1. Spherical - lodges the saccule 2. Elliptical - lodges the utricle |
|
|
|
What passes through aqueduct of vestibule? |
Endolymphatic duct |
|
|
|
What is Crus Commune? |
The nonampullated ends of posterior and superior semicircular canals unite to form a common channel called crus commune. |
|
|
|
What is modiolus? |
The bony cochlea is a coiled tube making 2.5 to 2.75 turns round a central pyramid of bone called modiolus. |
|
|
|
Components of bony cochlea |
(a) Scala vestibuli (b) Scala tympani (c) Scala media or the membranous cochlea |
|
|
|
What is helicotrema? |
It is an opening through which scala vestibuli and scala tympani (filled with perilymph) communicate with each other at the apex of cochlea. |
|
|
|
What is scala Vestibuli closed by? |
By the footplate of stapes which separates it from the air-filled middle ear. |
|
|
|
What is scala tympani closed by? |
By secondary tympanic membrane |
|
|
|
Constituents of membranous labyrinth |
It consists of the cochlear duct, the utricle and saccule, the three semicircular ducts, and the endolymphatic duct and sac. |
|
|
|
Walls of Cochlear duct/scala media/membranous cochlea |
1. Basilar membrane 2. Reissner's membrane 3. Stria vascularis |
|
|
|
Cochlear duct is connected to saccule via |
Ductus reuniens |
|
|
|
What is macula? |
The sensory epithelium of the utricle is called macula and is concerned with linear acceleration and deceleration. |
|
|
|
What is Crista ampullaris? |
The ampullated end of each semicircular duct contains a thickened ridge of neuroepithelium called crista ampullaris. |
|
|
|
Surgical importance of Endolymphatic sac |
It is exposed for drainage or shunt operation in Ménière’s disease. |
|
|
|
Perilymph is rich in? |
Sodium ions |
|
|
|
Endolymph is rich in |
Potassium ions |
|
|
|
Endolymph is secreted by |
It is secreted by the secretory cells of the stria vascularis of the cochlea and by the dark cells. |
|
|
|
Blood supply of labyrinth |
labyrinthine artery, which is a branch of anterior-inferior cerebellar artery but sometimes from the basilar. |
|
|
|
Divisions of labyrinthine artery |
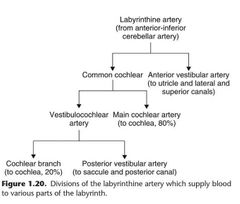
|
|
|
|
Venous drainage of labyrinth |
1. Internal auditory vein 2. Vein of cochlear aqueduct 3. Vein of vestibular aqueduct which ultimately drain into inferior petrosal sinus and lateral venous sinus. |
|
|
|
Development of Tragus and pinna |
Tragus develops from the tubercle of the first arch while the rest of the pinna develops from the remaining five tubercles of the second arch. |
|
|
|
What forms preauricular sinus |
Faulty fusion between the first and the second arch tubercles causes preauricular sinus or cyst |
|
|
|
External auditory meatus develops from |
First branchial cleft |
|
|
|
Pinna is fully developed by |
20th week |
|
|
|
External ear canal is fully developed by |
28th week gestation |
|
|
|
Middle ear cleft develops from |
Endoderm of tubotympanic recess |
|
|
|
Development of ossicles |
Malleus and incus- Mesoderm of 1st arch Stapes- second arch Footplate and and annular ligament - derived from the otic capsule |
|
|
|
What forms otocyst/auditory vesicle? |
Ectoderm in the region of hindbrain thickens to form an auditory placode, which is invaginated to form auditory vesicle or the otocyst. |
|
|
|
Development of ear in nutshell |
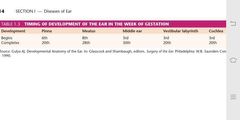
|
|

