![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
|
where are the spermatogonium located and what do they do?
|
line the seminiferous tubules and provide a pool for primary spermatocytes
|
|
|
what are the 2 secretions of sertoli cells and their functions?
|
1. androgen binding proteins- to keep testosterone in the testes
2. inhibin- to keep FSH in check |
|
|
what kind of physical prtection do the sertoli cells offer the spermatozoa? from what?
|
they form tight junctions to form a blood-testes barrier to protect the developing sperm from the immune system
|
|
|
what happens to sertoli cells in higher heat? what functions are lost? 2
|
1. lose inhibin secretion
2. spermatogenesis rate goes down |
|
|
what are 2 conditions that cause the testes to be too warm? how so?
|
1. varicoceles- blood is being suck there and not in the counter current exchange
2. cryporchidism- testes too high |
|
|
function of leydig cells?
|
just to secrete testosterone
|
|
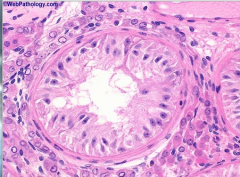
where are the sertoli and leydig and sperm cells? what separates them?
|
inside seiniferous tubules- sertoli and spermatozoa
interstitium- leydig cells in between is a basement membrane |
|
|
where are the oldest spermatids?
|
closer to the lumen of the tubules
|
|
|
list the stages from spermatogonium to the final stage
|
spermatogonium --> primary spermatocyte --> secondary spermatocyte --> spermatids --> spermatozoa (sperm cells)
|
|
|
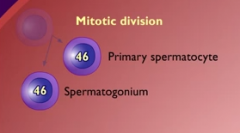
say the process that causes each stage change and the chromosome number in each.
spermatogonium --> primary spermatocyte --> secondary spermatocyte --> spermatids --> spermatozoa |
spermatogonium 46n -(mitosis)->
primary spermatocyte 46n -(first meiotic division)-> secondary spermatocyte 23n -(second meitic division)-> spermatids 23n -(maturation)-> spermatozoa 23n |
|
|
how can you divide twice in meiosis and still only have haploid cells?
|
the chromosomal material doubles before the first meiotic division
|
|
|
what happens in the first step of spermatogenesis? cells produced?
|
1 spermatogonium to replenish and 1 primary spermatocyte to make sperm
|
|
|
What do the chromosomes look like during meiosis? what sticks together?
are any of the germ cells the same? (in terms of whole chromosomes not counting crossing over) |
1. prophase- each mommy and daddy chromosome doubles and hangs onto it's sister
2. 1st meiotic division - the mommy and daddy chromosomes get scrambled to different primary germ cells, but still have their sisters 3. 2nd meiotic division- sister chromatids must separate and the two ovum/spermatids are the same 23n |
|
|
|
|
|
difference between spermatogenesis and spermiogenesis?
|
spermiogenesis is the final phase of spermatogenesis where the spermatids mature inro spermatozoa
|
|
|
what is the critical step in spermatogenesis not present in poogenssis that allows sperm to be created infinitey?
|
the first mitosis step to regenerate the spermatogonium
|
|
|
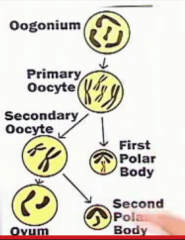
when does a primary oocyte become secondary?
a secondary to become an ovum? mnemonic for both? stages and events. |
primary to secondary- prOphase I for Ovulation
secondary to ovum- metaphase II for fertilization (the egg MET the sperm) |
|
|
in a graffian follicle, what kind of oocyte is inside? how do you know?
|
primary in prophase 1 or secondary in metaphase II depending on how far along the graffian follicle is
|
|
|
what does the sperm gain in spermiogenesis? what is lost? how is the shape changes
|
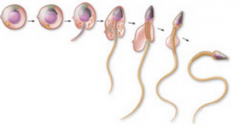
acrosomal cap, midpiece
loss of cytoplasm to be more oval than round |
|
|
what stage of life does spermatogenesis begin? implications for early sex havers?
|
puberty
a boyu having sex before pubertty cannot impregnate someone |
|
|
what is the ploidy change in meiosis 1?
|
fro diploid to haploid (but with sister chromosomes)
|
|
|
what cells will accumulate if you lose the abiloty for meiosis 1?
|
primary spermatocytes
|
|
|
change in cells in meiosis II?
cell accumulation in failure of this process? |
from haploid sister chromatids (secondary spermatocytes) to haploid spermatids
accumulation of secondary spermatocytes |
|
|
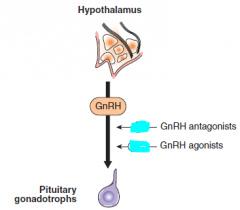
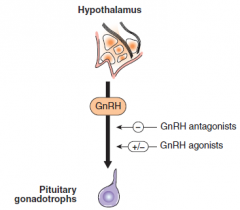
what is the pattern of GnRH release in males?
|
pulsatile
|
|
|
What is the effect of GnRH agonists and antagonists?
2 effects of agonists based on style of administreation. |
antagonist- lower pulsatile GnRH
agonist- will lower if continuous, but raise if also pulsatile |
|
|
what two drugs can inhibit leydig cell production of testosterone? how? what enzymes?
|
ketoconazole- inhibits desmolase
spironolactone- inhibits 17 a-hydroxylase and desmolase |
|
|
what other anti androgen effect does spironolactone have? how do you know?
what off label uses is it used for? |
it is a potent androgen antagonist because it also antagonizes another steroid, aldosterone
can be used to treat male pattern baldness or hirsuitism |
|
|
what can excess DHT do to you besides hair loss?
|
benign prostatic hyperplasia
|
|
|
what drug can be used to treat both male pattern baldness and BPH? mechanism?
|
finasteride- inhibition of 5-a reductase
|
|
|
what are 3 androgen receptor blockers? do they work for just DHT or testosterone?
mnemonioc? |
works for both
flutamide, cyproterone, spironolactone a bald cyclop[s tripping on acid playing a flute that is also a spear used to cut his hair - all these things block androgen receptors |
|
|
|
|
|
what organs produce DHT, testosterone, and androstenedione in males?
|
testes- testosterone
adrenals- androstenedione periphery- DHT |
|
|
what does testosterone do in embryonic develpopment?
|
helps devlop all the mesonephric ducts things
epididymus, VD, seminal vesicles not prostate |
|
|
What does testosterone help do in puberty??
|
growth spurts (why boys are taller) and closing of epiphyseal plates
deepening of voice develops sperm, penis, seminal vesicles, etc |
|
|
why may you not want to give testosteone to a person who hasn;t finished puberty yet"?
|
you could close their epiphyseal plates
|
|
|
what common thing does testosterone do in males and females?
|
stimulate sex drive
|
|
|
what is the function of DHT early and late in life?
|
early- differetiation of early external genitalia (helpful!)
late- continues to make prostate grow and causes increased sebaceous gland activity and hair loss |
|
|
how do you remember that testosterone doesn't induce prostate growth? 2 reaons
|
1. it is only responsible for the mesonephric duct early on and prostate is past this
2. it is DHT that causes BPH |
|
|
what 2 places can testosterone become estrogen? what is special about these places?
|
1. sertoli cells
2. fat they have aromatase |
|
|
what are some consequences of taking male steroids for body building? why?
|
hypogonadism and azoospermia
you suppress the HPG axis and no longer get gonadotropins keeping the testes in function |
|
|
what is the synthetic testosterone that we use?
|
methyltestosterone or just testosterone
|
|
|
What are 3 clinical uses of methyltestosterone?
|
1. giving secondary male sex characteristics
2. supplement for hypogodnadism in males 3. stimulation of anabolism to increase recovery rate after burn or injury |
|
|
What does overdoase of testosterone do in fameles vs males?
|
females- masculinization
males-hypogonadism or even atrophy |
|
|
at hwta point does exogenous testosterone cause azoospermia?
|
at gonadal atrophy
|
|
|
What is the bone risk of giving too much testosterone?
The blood lipid risk? mnemonic? |
bone- premature plate closure
blood lipid- increase LDL, lower HDL (why men get more heart attacks) |
|
|
What disease that a pt has should be a big warning not to give testosterone? why?
|
prostate cancer- could make it grow more
|
|
|
what are some mechanisms of antiandrogens?
|
decrease testosterone synthesis
decrease T-->DHT conversion decrease androgen binding to receptor |
|
|
full name for desmolase?
|
17, 20 desmolase
|
|
|
2 mechanisms to treat BPH?
|
1. inhibit DHT synthesis
2. relax the smooth muscle there |
|
|
what medications will do the following?
1. inhibit DHT synthesis 2. relax the smooth muscle there |
1. inhibit DHT synthesis- finasteride, butasteride
2. relax the smooth muscle there- a1 A,D anatagonists - ending with "zosin" or "osin" |
|
|
What drug will treat BPH via the SM relaxation mechanism? how does it not cause hypotension?
mnemonic? |
Tamsulosin
it is selective for a1 A,D instead of the a1 B in blood vessel smooth muscle must TAME the angry prostate |
|
|
mechanism and only approved use for flutamide?
|
non steroidal competitive inhibitor of androgen receptor
used for prostatic carcinoma If the prostate is malignantly angry, sooth it with a flute |
|
|
what drugs are used to treat PCOS and what aspect of it specifically? 2
mechanism for each? mnemonic? |
ketoconazole and spironolactone used to preven hirsuitism in females
ketoconazole- block synthessis with desmolase spironolactone- block synthesis with desmolase and 17 a hydroxylase AND androgen receptor antagonist Landon with a spear going to cut the beard off the PCOS peacock |
|
|
side effects of spironolactone and ketoconazole? 1 male and 1 female
|
males- gynocomastia
females- amenorrhea don't understand cause these drugs are used to treat women |
|
|
what kind of defect do people with androgen insensitivity syndrome have?
what is their chromosomes? |
something wrong with androgen receptor/response sequence
they are 46XY and normal |
|
|
what is responsible for pubic hair?
|
testosterone
|
|
|
what do males with androgen insensitivity syndrome look like on the outside? Why?
what reproductive structures do they have? |
they are externally female- no DHT
they have no internal female structures- no testosterone no secondary male sex characteistics- no testosterone |
|
|
What kind of vagina with men with androgen insensitivity have? Why?
|
only the lower 2/3rds because they did have MIF that prevented paramesonephric duct development
|
|
|
will men with androgen insensitivity have pubic hair? why?
|
no because no testosterone
|
|
|
will men with androgen insensitivity syndrome have female secondary sex characteristics without ovaries?
|
yes because the excess androgen will be turned into estrogen at the periphery
|
|
|
what kind of external feature can you look for to check for androgen insensitivity syndrome? where?
|
two lumps in the labia majora that are the testes
|
|
|
What does a man with AIS look like?
|
strikingly tall and beautiful female
|
|
|
why may you want to take these testes in the labia majora out?
|
to prophylactically prevent malignancy.
|
|
|
What do you need to do after taking out the testes? consequence if you don;t?
|
treat with estrogens to prevent menopause sx
|
|
|
will you have a normal amount of testosterone and estrogen in the bod of AIS? Why?
|
raised because the body is insensitive to it and even the hypothalamus think that there is none
all of this will be pushed over to estrogen |
|
|
what are some differences in the structure (inside and out) of people with AIS vs people with 5a-reductase deficiency? why for each?
|
AIS- no male maturation inside or out. genitals are female from estrogen.
5aRD- male maturation, but externally ambiguous (no DHT or estrogen) until puberty |
|
|
Compare testosterone, estrogen, and LH levels in people with AIS vs 5aRD
|
AIS- raised T and LH and E
5aRD- normal T and LH and E |
|
|
define pseudohermaphroditism.
|
difference between phenotype and sex
disagreement between inside and outside |
|
|
difference between pseudohermaphrodotism and hermaphrodistism
|
hermaphrodites have both gonads
|
|
|
what is a female with hermaphroditism? what do they look like inside and out?
|
female internal organs
outside is either male or ambiguous |
|
|
2 possible causes of female pseudohermaphroditism? common mechanism?
|
exposure to androgens during development
1. congenital adrenal hyperplasia 2. mother is exposed to testosterone |
|
|
example of disease causing male pseudohermaphroditism?
|
AIS
|
|
|
what karyotypes can be true hermaphrodites?
|
46 XX or 46 XXY
|
|
|
alternate name for true hermaphroditism?
|
ovotesticular disorder of sex development
|
|
|
what do hermaphrodites look like on the outside vs the inside?
|

outside- ambiguous genitalia and features
inside- have ovotestes |
|
|
what do ambiguous genitalia look like?
|

|
|
|
how many carbons are on testosterone and androstenedione?
|
19
|
|
|
what is the cause of klinefelter's?
|
nondysjunction of sex chromosomes in meiosis II
|
|
|
what is the karyotype of klinefelter's?
|
47 XXY
|
|
|
what can you see under the microscope to check for kline felter's?
|
barr body
|
|
|
how common is kline felter's?
|
pretty common 1/850
|
|
|
what are some physical appearances of XXY? 5
|

1. gynocomastia
2. long limbs 3. female hair pattern 4. small penis 5. testicular atrophy 6. eunuchoid body habitus |
|
|
what are the Lh and FSH levels in males with klinefelter's?
|
both high
|
|
|
Why is FSH high in XXY?
|
dysgenesis of seminiferous tubules --> sertoli cells secrete less inhibin --> FSH rises
|
|
|
why do you get raised LH in XXY?
|
abnormal leydig function --> low testosterone --> high LH
|
|
|
physical appearance in turner's syndrome?
|

short stature
|
|
|
signs of epididymitis on physical exam?
where is it in the testes? |
very tender lumps in back of testes
|
|
|
physical manipulations to reduce tenderness in epididymitis? 2 why does this work?
|
put pressure on it or elevate it like all inflammation
|
|
|
1 cause of epididymitis
|
bacteria infection through the urinary tract
|
|
|
most common 2 causes of epididymitis in men under 35. why?
|
chlamydia and gonorrhea because they are acute STI's
|
|
|
what about men over 35? why?
|
e. coli because then it;s probably from the rectum
|
|
|
what is twisted in testicular torsion?
|
the spermatic cord
|
|
|
what can go wrong in torsion if not fixed soon?
|
the testes become ischemic and die
|
|
|
what do they do in surgery to prevent future torsion? specific name and describe and dissect
|
orchiopexy- tack the testes to the scrotum
testes- orchio surgical fixation- pexy |
|
|
dissec cryptorchidism
|
mysterious/hidden
testes |
|
|
what happens in cryptorchisidsm? is it symmetric usually?
|
failure of testes to descend, usually unilateral
|
|
|
when do the testes descend?
|
in the 1st year of life
|
|
|
why would we care so much about cryptorchidism clinically? 2
|
the high temperature predispose males to germ cell malignancy
can lead to decreased fertility |
|
|
what is the treatment for cryporchidism?
|

orchiopexy
drab the testes down and fixate it |
|
|
so why can't people with AIS keep their beauty producing testes?
|
35x greater risk of malignancy with undescended testes
|
|
|
why would you do a oriectomy rather than a orchioplexy?
|
when there is nowhere for the testes to descend like in AIS or in male cryporchidism past infancy
|
|
|
what should you rule out before diagnosing cryptorchidism? 2 why?
|
that this isn't actually a masculinized woman
congenital adrenal hyperplasia and early exposure to testosterone |
|
|
what proportion of testicular cancers will be germ cell tumors?
|
95%
|
|
|
what exam can you do to see if a testicular mass may be a tumor?
|
transilluminate it and see if it shines through- cancer should not
|
|
|
what if the enlarged testes does transilluminate?
|
hydrocele
|
|
|
picmonic for 5 a-reductase deficiency
|

|
|
|
picmonic for AIS
|

|
|
|
wjhy is estrogen increased in klinefelter?
mnemonic? |
xxy- more x's mean more estrogen
unknown mechanism so stop trying to rach your brain over it! |
|
|
picmonic for klinefelter's
|

|
|
|
mnemonic for name of process of creating barr bodies?
|

lyonization- lions are cats. cats have calico color from shutting off one x chromosome.
|
|
|
is klinefelter's always xxy?
|
no it can have many X's
|
|
|
what are some variations of Turner's syndrome chromosomes? most common?
|
a missing or partially defective X chromosome
45 XO with it completely missing is the most common |
|
|
what is wrong with the lymph vessels in Turner's? name and description
|
the lymph vessels are dilated- lymphangiectasis
|
|
|
what are 3 consequences of lymphangiectasia in Turners? location and reason why
|
cystic hygroma- dilation of lymph vessels out the posterior triangle of the neck
webbed neck- a reminant of skin from the cystic hygroma lymphedema of hands and feet- where lymph tends to accumulate |
|
|
what is the estrogen level in people with turner's? mnemonic?
|
again with the X's
low due to only having 1 X |
|
|
why is the estrogen low?
|
turner's pts have poorly developed ovaries, wich are the main sources of estrogen
|
|
|
level of FSH and LH in Turner's? Why?
|
high due to lack of neg feedback
|
|
|
what kind of menstrual disorder do Turner's have?
|
primary amenorrhea
|
|
|
define primary amenorrhea
|
menstruation that never starts
|
|
|
what stages get mixed up in primary amenorrhea?
|
menopause comes before menarche
|
|
|
what other endocrine disorder do Turner's pts frequently suffere from? mnemonic?
|
hypothyroidism
think about a goiter on the neck along with the webbing |
|
|
what kind of associated congenital malformations are with Turner's? 3
|
bicuspid aortic valve
preductal aortic coarctation horseshoe kidney |
|
|
what cancer is associated with Turner's
picmonic? |
dysgerminoma
"disc-german-gnome" |
|
|
what kind of chest do Turner's pts have?
|
shield chest with widely spaced nipples
|
|
|
picmonic for Turner's?
|

|
|
|
difference between hydrocele and varicocele? pathogenesis and feel.
|
variicocele- veins engorging from being backed up- bag of worms
hydrocele- tunica vaginalis unfused and letting in fluid- very tight scrotum in newborns |
|
|
treatment for hydrocele? why?
|
nothing, it usually goes away on it's own
|
|
|
what happens in a spermatocele?
|
you have a dilated epididymal duct where sperm gathers
|
|
|
which of the last 3 celes transilluminate?
|
all 3
hydrocele, varicocele, and spermatocele |

