![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
Case 1:
- 29 yo male recently diagnosed w/ HIV presents to ED w/ seizures - HIV viral load is 72,300 copies/mL and CD4+ count is 75 - History of DM, hyperlipidemia, chronic hepatitis B infection He gets an MRI as shown Which of the following would not be included in your differential diagnosis? a) Progressive multifocal leukoencephalopathy b) Toxoplasmosis c) CNS Lymphoma d) Tuberculosis |
Progressive multifocal leukoencephalopathy (this would present with multiple findings in the white matter of the brain, this usually occurs subacutely - symptoms of forgetfulness, neuropathy, focal deficit)
|
|
|
What are the most common causes of CNS mass lesions in patients with HIV?
|
- Toxoplasmosis
- Lymphoma |
|
|
Besides Toxoplasmosis and Lymphoma, what else can cause a CNS mass lesion in a patient with HIV?
|
• Tuberculosis
• Fungal • Bacterial • Syphilis • Nocardia • Kaposi’s sarcoma • Chagoma • Glioblastoma |
|
|
How do you manage an HIV patient with a brain lesion
|
Check for toxoplasmosis
Brain lesion + Toxo serology positive - Start empiric treatment with sulfadiazine + pyrimethamine + leucovorin - Alt: clindamycin+pyrimethamine - Treat for 6 weeks Monitor for improvement - If improved after 7 days, then continue treatment - If no improvement or decline after 3 days, pursue brain biopsy |
|
|
Case 1:
- 29 yo male recently diagnosed w/ HIV presents to ED w/ seizures - HIV viral load is 72,300 copies/mL and CD4+ count is 75 - History of DM, hyperlipidemia, chronic hepatitis B infection He is started on sulfadiazine and pyrimethamine and leucovorin for empiric toxoplasmosis. He is interested in starting antiretroviral therapy. Which of the following regimens would you initiate? a) atazanavir + ritonavir + emtricitabine + tenofovir b) raltegravir + abacavir + maraviroc c) zidovudine + abacavir + efavirenz d) zidovudine + lamivudine + emtricitabine e) efavirenz + tenofovir + emtricitabine |
efavirenz + tenofovir + emtricitabine
- He has HIV and HepB - if there are drugs that treat both, you would focus on those - For treating HIV, you want to have >1 mechanism - He also has diabetes and hyperlipidemia, must consider whether the drugs will affect those |
|
|
Case 1:
- 29 yo male recently diagnosed w/ HIV presents to ED w/ seizures - HIV viral load is 72,300 copies/mL and CD4+ count is 75 - History of DM, hyperlipidemia, chronic hepatitis B infection He is started on sulfadiazine and pyrimethamine and leucovorin for empiric toxoplasmosis. He is interested in starting antiretroviral therapy. What treatment strategies should you use when treating this patient? |
- Avoid protease inhibitors in this patient (elevate blood glucose and circulating lipids)
- Needs HBV drugs (ideally also target HIV) - Need multiple mechanisms for HIV |
|
|
What HIV drugs are protease inhibitors? Negative side effects?
|
Drugs that end in "-navir" (eg, lopinavir, atazanavir, darunavir, etc)
- These drugs can raise blood glucose and circulating lipids - You should avoid these in patients with DM / hyperlipidemia - Atazanavir has lesser effect on lipids |
|
|
What are the drugs that treat both HIV and HBV?
|
– FDA-approved: lamivudine, tenofovir
– Not approved but has activity: emtricitabine |
|
|
What drugs are Nucleoside Reverse Transcriptase Inhibitors?
|
- Zidovudine
- Lamivudine - Emtricitabine |
|
|
What drug class are these drugs: Zidovudine, Lamivudine, Emtricitabine? What are some side effects associated with these drugs?
|
Nucleoside Reverse Transcriptase Inhibitors
- In general: lactic acidosis, hepatic steatosis - Zidovudine: BM, myopathy, inhibits glucuronyltransferase - Lamivudine, Tenofovir, Emtricitabine: GI - Abacavir: hypersensitivity (assoc. w/ HLA-B*5701 antigen) |
|
|
Which HIV drug is associated with a hypersensitivity reaction? What should you do if a patient has this reaction?
|
Abacavir (NRTI)
- Associated with HLA-B*5701 antigen - Never give this drug to this patient again |
|
|
What kind of drug is Efavirenz? What are the side effects?
|
Non-Nucleoside Reverse Transcriptase Inhibitor (NNRTI)
- CNS / psychiatric symptoms, rash - Induces CYP3A, 2B6 - Inhibits CYP3A, 2C9, 2C19 |
|
|
What are the side effects associated with Maraviroc?
|
- Cardiovascular events
- Hepatotoxicity - Cough - Rash |
|
|
What are the side effects associated with Raltegravir?
|
- GI
- Headache - Myopathy - Skin hypersensitivity |
|
|
What is the cause of Progressive Multifocal Leukoencephalopathy (PML) in HIV patients?
|
Caused by JC virus (papovavirus) that infects oligodendrocytes
- Results in lytic infection inducing demyelination - Also infects astrocytes resulting in bizarre morphology JC virus is re-activated with immunosuppression (80% of PML occurs in AIDS) - Disseminates through bloodstream to CNS |
|
|
Who is infected with JC virus?
|
Most have serologic evidence of prior JC virus infection by adolescence
|
|
|
What are the clinical features of Progressive Multifocal Leukoencephalopathy (PML)?
|
- Acute / subacute focal neurologic deficits
• Cerebral white matter most common but cerebellum and brainstem also seen • Hemiparesis, visual field deficits, aphasia, ataxia • Seizures rare - CD4 typically <100 but cases seen at higher CD4 |
|
|
What are the characteristics of neuroimaging of patients with Progressive Multifocal Leukoencephalopathy (PML)?
|
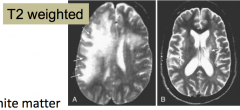
MRI shows T2 bright white matter changes usually WITHOUT ENHANCEMENT OR MASS EFFECT
|
|
|
How do you diagnose Progressive Multifocal Leukoencephalopathy (PML)?
|
CSF: Bland CSF profile with minimal elevation in protein
• Sensitivity of PCR for JC virus ranges from 60% to >95% with excellent specificity Pathology: Patchy demyelination with focal necrosis, enlarged oligodendrocytes and bizarre astrocytes |
|
|
What is the prognosis for Progressive Multifocal Leukoencephalopathy (PML)?
|
Patients typically die within 6 months but 10% will have more prolonged course (helps if you can improve CD4 counts)
CD4+ at diagnosis <100 increases risk of death two-fold |
|
|
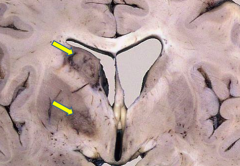
What is the gross appearance of Progressive Multifocal Leukoencephalopathy (PML)?
|
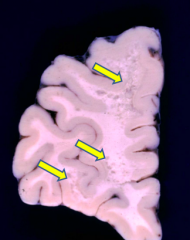
Small foci of gray discoloration in the white matter
|
|
|
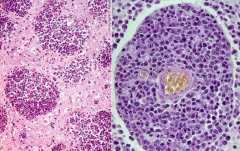
What is the histologic appearance of Progressive Multifocal Leukoencephalopathy (PML)?
|
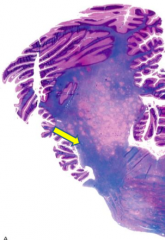
Picture: Irregularly poorly defined areas of demyelination (myelin statin: blue indicated myelin is present and pink means it is absent)
- Bizarre astrocytes and oligodendrocytes with inclusions |
|
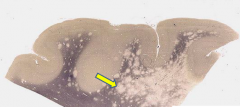
What does this slide show?
|
Progressive Multifocal Leukoencephalopathy (PML)
- Normal myelin is black, affected areas are pale (no myelin) |
|
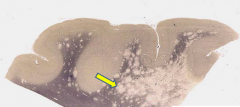
What does this slide show?
|
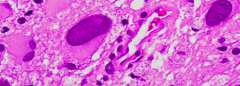
Progressive Multifocal Leukoencephalopathy (PML)
- Bizarre astrocytes |
|
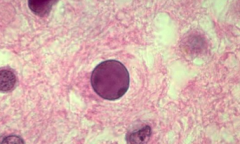
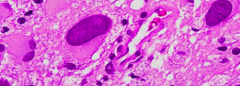
What does this slide show?
|
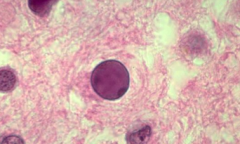
Progressive Multifocal Leukoencephalopathy (PML)
- Oligodendrocyte with inclusion |
|
|
What is the electron microscope appearance of JC virus?
|
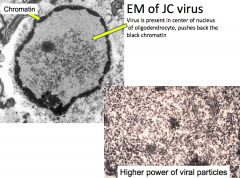
- Virus is present in the center of the nucleus of oligodendrocyte, pushes back the black chromatin
- Bottom right: higher power of viral particles |
|
|
What is the most frequent CNS complication in AIDS patients?
|
Toxoplasma encephalitis (Toxoplasma gondii - protozoa)
|
|
|
What causes Toxoplasma encephalitis in AIDS patients?
|
Infection with Toxoplasma gondii (protozoa)
- Reactivation of latent infection as a result of loss of cellular immunity - Incidence of seropositivity for T. gondii is 30% |
|
|
What is the clinical presentation of Toxoplasma encephalitis?
|
Subacute (days to one month)
- 90% have CD4+ counts <200 cells/µL - Headache, confusion, fever, lethargy - Seizures (30%) - Focal neurologic signs (70%) |
|
|
What happens to CSF in patients with Toxoplasma encephalitis?
|
- Slight increase in protein
- Slight decrease in glucose - PCR for T. gondii DNA (100% specificity but 44% sensitivity) |
|
|
What are the characteristic of imaging of Toxoplasma encephalitis?
|
MULTIPLE lesions with ENHANCEMENT
- May see mass effect - Usually at gray/white matter interface, white matter, or basal ganglia |
|
|
What is the prognosis of Toxoplasma encephalitis?
|
- At one year 10-23% are dead (with treatment
- Persistent neurologic impairment in 37% of those that survive |
|
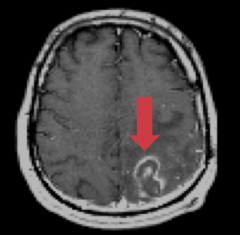
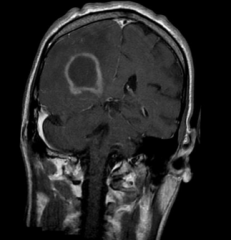
What does this MRI show?
|
Toxoplasma encephalitis
- Multiple lesions with enhancement |
|
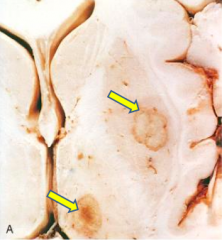
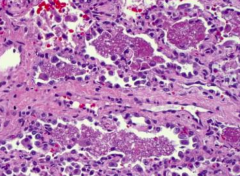
What does this gross image show?
|
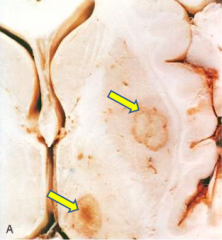
Toxoplasma encephalitis
|
|
|
What are the histologic findings in Toxoplasma encephalitis?
|
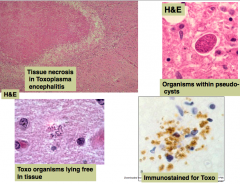
- Tissue necrosis
- Organisms within pseudocysts - Toxo organisms may lie free in tissue - Immunostain for Toxo (brown) |
|
|
How common are primary CNS lymphomas in AIDS patients?
|
10% of AIDS patients (usually late-stage)
|
|
|
What is the clinical presentation of primary CNS lymphoma?
|
- Average CD4+ T cell count is ~50 cells/µL
- Subacute (weeks to months) - Confusion, lethargy, memory loss - With progress: seizures, focal neurologic deficits |
|
|
What are the CSF findings in patients with primary CNS lymphoma in AIDS?
|
- Increased protein
- Mild mononuclear cell increase - Look at cytology and flow cytometry |
|
|
What are the characteristics of systemic lymphomas (outside of CNS) in AIDS patients?
|
They do not usually spread into CNS
|
|
|
What are the characteristics of CNS lymphomas in AIDS patients?
|
Usually do not spread outside of CNS
|
|
|
What are the characteristics of primary CNS lymphoma on imaging in AIDS?
|
Often MULTIPLE lesions in a periventricular location with contrast enhancement and mass effect
|
|
|
What are the typical characteristics of a biopsy of a primary CNS lymphoma?
|
- Usually B-cell lineage
- Usually EBV positive |
|
|
What is the prognosis of primary CNS lymphoma in AIDS patients? How do you treat?
|
Poor prognosis - usually die within one year
- Treat with chemotherapy and radiation |
|
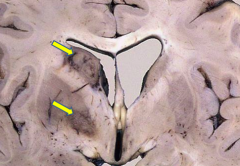
What is this gross pathology indicative of?
|
Primary CNS lymphoma in AIDS
- Periventricular mass lesions with necrosis |
|
|
What is the histologic appearance of primary CNS lymphoma in AIDS?
|
Perivascular arrangement of neoplastic cells
|
|

Case 2:
- 54 yo man with HIV presents w/ 3-4 weeks of SOB - Previously viral load was undetectable on efavirenz, tenofovir, emtricitabine - Also taking lovastatin, omeprazole, and prn ergotamine for other medical conditions - SOB occurs at rest and w/ minimal exertion - Dry cough associated - He is tachypneic and SaO2 on RA is 91% He gets a chest x-ray done. How would you describe these findings? |

Patchy alveolar infiltrates bilaterally
|
|

Case 2:
- 54 yo man with HIV presents w/ 3-4 weeks of SOB - Previously viral load was undetectable on efavirenz, tenofovir, emtricitabine - Also taking lovastatin, omeprazole, and prn ergotamine for other medical conditions - SOB occurs at rest and w/ minimal exertion - Dry cough associated - He is tachypneic and SaO2 on RA is 91% His chest x-ray shows patchy alveolar infiltrates bilaterally. Which of the following is the most likely diagnosis? a) CMV Pneumonitis b) Bacterial Pneumonia c) Pneumocystis jiroveci pneumonia d) Lymphoma e) None of the above |

Pneumocystis jiroveci pneumonia (PCP)
- CMV pneumonitis is more common in transplant or BM transplant patients, does occur in immunosuppressed patients only; CMV more typically causes retinitis and gastric ulcers in HIV patients - Bacterial pneumonia is more common with consolidated infiltrate (less likely to be widespread / diffuse) - Lymphoma usually doesn’t present as a pneumonia like this picture |
|
|
Case 2:
- 54 yo man with HIV presents w/ 3-4 weeks of SOB - Previously viral load was undetectable on efavirenz, tenofovir, emtricitabine - Also taking lovastatin, omeprazole, and prn ergotamine for other medical conditions - SOB occurs at rest and w/ minimal exertion - Dry cough associated - He is tachypneic and SaO2 on RA is 91% His chest x-ray shows patchy alveolar infiltrates bilaterally. Most likely a Pneumocystis jiroveci pneumonia. What do you want to ask this patient about his anti-retroviral therapy? Why? |
- Has he been taking all of his HIV drugs every day
Lack of compliance allows for - HIV replication - High replication rate and poor proofreading activity of reverse transcriptase leads to spontaneous mutations which can result in drug resistance If this patient is taking his meds he should not be getting an opportunistic infection like P. jiroveci! |
|
|
What is the most effective mechanism to prevent opportunistic infections in patients with HIV?
a) Drug combination that inhibits ergosterol synthesis and blocks folate synthesis b) Drug combination that inhibits dihydrofolate reductase and dihydroopteroate synthase c) An acyclic guanosine analog plus a dihydrofolate reductase inhibitor d) Ubiquinone analog plus a 50S ribosomal inhibitor e) HAART therapy Why? |
HAART Therapy
- Blocking HIV replication keeps the CD4 counts high enough to decrease the probability of opportunistic infections |
|
|
What is the mechanism / function of Fluconazole?
|
Antifungal - blocks ergosterol synthesis
|
|
|
What is the mechanism of Clindamycin?
|
50S ribosomal inhibitor
|
|
|
What is the mechanism / use of Ganciclovir?
|
- Acyclic guanosine analog
- Used for CMV |
|
|
What are the characteristics of Pneumocystis pneumonia in AIDS patients? When is it more likely?
|
- Caused by Pneumocystis jiroveci
- Frequent sentinel opportunistic infection in HIV positive patients - Occurs when CD4+ T cell count <50 cells/µL |
|
|
What are the clinical findings of Pneumocystis pneumonia?
|
- Subacute / chronic illness
- Fever, SOB, dyspnea |
|
|
What is the typical CXR finding for Pneumocystis pneumonia?
|

Diffuse interstitial infiltrates
|
|
|
How can you diagnose Pneumocystis pneumonia?
|
Sputum sample stained for the organism
|
|
|
What is the histologic appearance of lung tissue with Pneumocystis pneumonia infection?
|
- Fluffy, intraalveolar exudates and sparse inflammatory infiltrate, pathognomonic of PCP
- Blue dot-like structures in acellular exudates |
|
|
What stain is special for Pneumocystis pneumonia? Appearance?
|
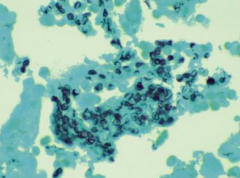
GMS stain
- Numerous, intraalveolar, boat-shaped and crescentic cyst forms of Pneumocystis |
|
|
Which of the following is the most common first-line regimen for the prophylaxis and treatment of Pneumocystis jiroveci?
a) Trimetrexate b) Sulfamethoxazole + trimethoprim c) Clindamycin + primaquine d) Dapsone e) Atovaquone |
Sulfamethoxazole + trimethoprim
All of these drugs can be used for Pneumocystis, but the first line is TMP/SMX |
|
|
Which drugs can be used for Pneumocystis pneumonia? What is the first line?
|
** Sulfamethoxazole + trimethoprim (first line)
- Trimetrexate - Clindamycin + primaquine - Dapsone - Atovaquone |
|
|
Case 2:
- 54 yo man with HIV presents w/ 3-4 weeks of SOB - Previously viral load was undetectable on efavirenz, tenofovir, emtricitabine - Also taking lovastatin, omeprazole, and prn ergotamine for other medical conditions - SOB occurs at rest and w/ minimal exertion - Dry cough associated - He is tachypneic and SaO2 on RA is 91% His chest x-ray shows patchy alveolar infiltrates bilaterally. Most likely a Pneumocystis jiroveci pneumonia. What do you need to consider when switching his HIV regimen? |
Considerations:
- Viral resistance profile - Drug interactions (he is also taking lovastatin, ergotamine (CYP3A), and omeprazole (CYP2C19) |
|
|
Case 2:
- 54 yo man with HIV presents w/ 3-4 weeks of SOB - Previously viral load was undetectable on efavirenz, tenofovir, emtricitabine - Also taking lovastatin, omeprazole, and prn ergotamine for other medical conditions - SOB occurs at rest and w/ minimal exertion - Dry cough associated - He is tachypneic and SaO2 on RA is 91% His chest x-ray shows patchy alveolar infiltrates bilaterally. Most likely a Pneumocystis jiroveci pneumonia. What HIV drugs could he be on without worrying about viral resistance or drug interactions? |
- Protease inhibitors (strong inhibitors of CYP3A, some also affect P-glycoprotein and other drug transporters)
- Efavirenz (competitive inhibitor of CYP3A and 2B6) - Maraviroc (CYP3A substrate) - Raltegravir, NRTIs, enfuvirtide (no significant CYP interactions) |
|
|
Which HIV drugs do not have significant CYP interactions?
|
- Raltegravir
- NRTIs - Enfuvirtide |
|
|
Which HIV drugs are metabolized by glucuronyltranferases (UGTs)?
|
Zidovudine and Raltegravir
|
|
|
Which HIV drugs inhibit CYP3A?
|
- Protease inhibitors
- Efavirenz |
|
|
What organ system is a major target of HIV infection?
|
Nervous system
|
|
|
What are the most common cells infected by HIV?
|
Microglia (macrophages residing in the CNS)
|
|
|
How does HIV get into the brain?
|
Carried into brain by monocytes
|
|
|
How does HIV mediate its damage to the brain?
|
Soluble factors produced by infected microglia:
- IL-1 - TNF - IL-6 |
|
|
What are the types of CNS involvement by HIV infection?
|
- HIV meningitis
- HIV encephalitis / leukoencephalopathy - Vacuolar myelopathy |
|
|
How does HIV meningitis present?
|
Presents during acute flu-like illness at time of seroconversion
|
|
|
How does HIV encephalitis / leukoencephalopathy present? How common?
|
- Present in >75% of autopsied HIV patients
- Presents as AIDS dementia complex: cognitive and behavioral deterioration, eventually dementia, ataxia, and tremor |
|
|
What is the classic lesion associated with HIV encephalitis / leukoencephalopathy?
|
Microglial nodule containing multinucleated microglial cells (containing HIV virus)
|
|
|
What are the other histologic signs of HIV encephalitis / leukoencephalopathy?
|
- Perivascular lymphocytes
- Patchy demyelination - Astrocytosis - Slight diffuse atrophy |
|
|
What is the presentation of Vacuolar Myelopathy in HIV patients? How common?
|
- Resembles subacute combined degeneration of the spinal cord (which occurs d/t vitamin B12 deficiency)
- Present in up to 25% of HIV patients |
|
|
What happens to the CNS in Vacuolar Myelopathy in HIV patients?
|
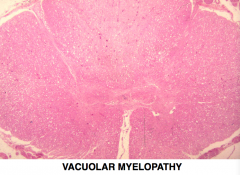
- Vacuolation of white matter, predominantly posterior and lateral columns
- Initially myelin and then axons degenerate |
|
|
What are the histologic findings associated with AIDS dementia complex?
|
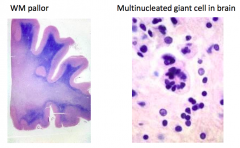
- White matter pallor
- Multinucleated giant cells in brain |
|
|
What are the histologic findings associated with HIV Encephalitis?
|
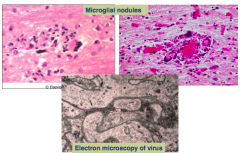
Microglial nodules
|

