![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
What defines a technically adequate CXR? |
Film must be "RIPE": - Rotation: clavicular heads are equidistant from thoracic spinous processes - Inspiration: diaphragm is at or below ribs 8-10 posteriorly and ribs 5-6 anteriorly - Penetration: disk spaces are visible but no bony detail of spine; bronchovascular structures are seen through heart - Exposure: make sure all lung fields are visible |
|
|
How should a CXR be read? |
Check the following: - Tubes and lines (check placement) - Patient data (name, date, history #) - Orientation (up/down, L/R) - Technique (AP or PA, supine or erect, decubitus) - Trachea (midline vs deviated, caliber) - Lungs (CHF, mass) - Pulmonary vessels (artery or vein enlargement) - Mediastinum (aortic knob, nodes) - Hila (masses, lymphadenopathy) - Heart (transverse diameter should be <1/2 transthoracic diameter) - Pleura (effusion, thickening, pneumothorax) - Bones (fractures, lesions) - Soft tissues (periphery and below the diaphragm) |
|
|
What CXR is better: PA or AP? Why? |
PA - less magnification of the heart (heart is closer to x-ray plate) |
|
|
Classically, how much pleural fluid can the diaphragm hide on upright CXR? |
It is said that the diaphragm can overshadow up to 500 cc |
|
|
How can CXR confirm that the last hold on a chest tube is in the pleural cavity? |
Last hold is through the radiopaque line on the chest tube; thus, look for the break in the radiopaque line to be in the rib cage |
|
|
How can a loculated pleural effusion be distinguished from a free-flowing pleural effusion? |
Ipsilateral decubitus CXR; if fluid is not loculated (or contained), it will layer out |
|
|
How do you recognize a pneumothorax on CXR? |
Air without lung markings is seen outside the white pleural line - best seen in the apices on an upright CXR |
|
|
What x-ray should be obtained before feeding via a nasogastric or nasoduodenal tube? |
Low CXR to ensure the tube is in the GI tract and NOT in the lung |
|
|
What C-spine views are used to rule out bony injury? |
CT scan |
|
|
What is used to look for ligamentous C-spine injury? |
Lateral flex and extension C-spine films, MRI |
|
|
What CXR finding may provide evidence of traumatic aortic injury? |
- Widened mediastinum >8 cm (most common) - Apical pleural capping - Loss of aortic knob - Inferior displacement of left main bronchus; NG tube displaced to the right, tracheal deviation, hemothorax |
|
|
How should a CT scan be read? |
Cross section with the patient in supine position looking up from the feet |
|
|
How should an abdominal x-ray (AXR) be read? |
Check the following: - Orientation: up/down, left-right - Technique: A-P or P-A, supine or erect, decubitus - Air: free air under diaphragm, air-fluid levels - Gas dilatation (3, 6, 9 rule) - Borders: psoas shadow, preperitoneal fat stripe shadow fecalith - Stool |
|
|
How can you tell the difference between a small bowel obstruction (SBO) and ileus? |
- In SBO there is a transition point (cut off sign) between the distended proximal bowel and the distal bowel of normal caliber (may be gasless) - In ileus, the bowel is diffusely distended |
|
|
What is the significance of the air-fluid level? |
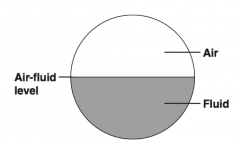
Seen in obstruction or ileus on an upright x-ray; intraluminal bowel diameter increases, allowing for separation of fluid and gas |
|
|
What are the normal calibers of the small bowel, transverse colon, and cecum? |
Use the "3, 6, 9" rule: - Small bowel <3 cm - Transverse colon <6 cm - Cecum <9 cm |
|
|
What is the rule of 3's for the small bowel? |
- Bowel wall should be <3 mm thick - Bowel folds should be <3 mm thick - Bowel diameter should be <3 cm thick |
|
|
How can the small and large bowel be distinguished on AXR? |
By the intraluminal folds: - The small bowel plicae circulares are complete - The large bowel plicae semilunares are only partially around the inner circumference of the lumen |
|
|
Where does peritoneal fluid accumulate in the supine position? |
Morison's pouch (hepatorenal recess), the space between the anterior surface of the R kidney and the posterior surface of the R lobe of the liver |
|
|
What percentage of kidney stones are radiopaque? |
~90% |
|
|
What percentage of gallstones are radiopague? |
~10% |
|
|
What percentage of patients with acute appendicitis have a radiopaque fecalith? |
~5% |
|
|
What are the radiographic signs of appendicitis? |
- Fecalith - Sentinel loops - Scoliosis away from the R because of pain - Mass effect (abscess) - Loss of psoas shadow - Loss of pre-peritoneal fat stripe - Very rarely, a small amount of free air, if perforated |
|
|
What does KUB stand for? What is it? |
Kidneys, Ureters, and Bladder: commonly used term for a plain film AXR (abdominal flat plate) |
|
|
What is the "parrot's peak" sign? |
Evidence of sigmoid volvulus on barium enema |
|
|
What is the "bird's beak" sign? |
Evidence of achalasia on barium swallow |
|
|
What is a "cut off sign"? |
Seen in obstruction, bowel distention, and distended bowel that is "cut off" from normal bowel |
|
|
What are "sentinel loops"? |
Distention or air-fluid levels (or both) near a site of abdominal inflammation (eg, seen in RLQ with appendicitis) |
|
|
What is loss of psoas shadow? What does this suggest? |
Loss of clearly defined borders of the psoas muscle on AXR; loss signifies inflammation or ascites |
|
|
What is loss of the peritoneal fat stripe? What does this imply? |
Loss of the lateral peritoneal / pre-peritoneal fat interface - Implies inflammation |
|
|
What is "thumb-printing"? |
Non-specific colonic mucosal edema resembling thumb indentations on AXR |
|
|
What is pneumatosis intestinalis? |
Gas within the intestinal wall (usually means dead gut) that can be seen in patients with congenital variant or chronic steroids |
|
|
What is free air? |
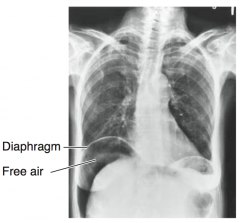
Air free within the peritoneal cavity (air or gas should be seen only within the bowel or stomach); results from bowel or stomach perforation |
|
|
What is the best position for the detection of FREE AIR (free intraperitoneal air)? |
Upright CXR - air below the right diaphragm |
|
|
If you cannot get an upright CXR, what is the second best plain x-ray for free air detection? |
Left lateral decubitus, because it prevents confusion with gastric air bubble; with free air both sides of the bowel can be seen; can detect as little as 1 cc of air |
|
|
How long after a laparotomy can there be free air on AXR? |
Usually 7 days or less |
|
|
What is Chilaiditi's sign? |
Transverse colon over the liver simulating free air on x-ray |
|
|
What should a post-op abdominal/pelvic CT scan for a peritoneal abscess be performed? |
POD #7 or later, to give time for the abscess to form |
|
|
What is the best test to evaluate the biliary system and gallbladder? |
Ultrasound (U/S) |
|
|
What is the normal diameter of the common bile duct with gallbladder present? |
<4 mm until age 40, then add 1 mm per decade (eg, 7 mm at age 70) |
|
|
What is the normal common bile duct diameter after removal of the gallbladder? |
8-10 mm |
|
|
What U/S findings are associated with acute cholecystitis? |
- Gallstones - Thickened gallbladder wall (>3 mm) - Distended gallbladder (>4 cm AP) - Impacted stone in gallbladder neck - Pericholecystic fluid |
|
|
What type of kidney stone is not seen on AXR? |
Uric acid (think Uric acid = Unseen) |
|
|
What med should be given prophylactically to a patient with a true history of contrast allergy? |
Methylprednisolone or dexamethasone; the patient should also receive non-ionic contrast (assoc. w/ 1/5 as many reactions as ionic contrast, the less expensive standard) |
|
|
What is a C-C mammogram? |

Cranio-Caudal mammogram, in which the breast is compressed top to bottom |
|
|
What is an MLO mammogram? |

MedioLateral Oblique Mammogram, in which the breast is compressed in a 45 degree angle from the axilla to the lower sternum |
|
|
What are the best studies to evaluate for a pulmonary embolus? |
- Spiral thoracic CT scan - VQ scan - Pulmonary angiogram (Gold standard) |

