![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
206 Cards in this Set
- Front
- Back
|
The most important parameter when assessing a child ?
|
the child's general appearance
|
|
|
where can the best assessment be taken of a child
|
from a distance, ideally while in a parent's arms
-Assessments from a distance are necessary because a stranger can have dramatic influence on a child’s appearance. |
|
|
How would you assess a child's alertness?
|
1. How responsive/perceptive is the child to others?
2. Distractibility: How readily does someone/something draw the child’s attention? 3. Consolability: Can a distressed child be comforted? 4. Speech/Cry: Strong/weak? Absent unless stimulated? 5. Spontaneous Activity: Responds only to stimuli? Appear flaccid? 6. Color: Pallor, flushing, cyanosis, or mottling? Centrally vs. peripherally. 7. Respiratory Effort: Accessory muscle use? 8. Eye Contact: Able to maintain contact with people/objects? Gaze aimlessly? |
|
|
what are the components of general appearance of a child?
|
alertness
airway breathing circulation |
|
|
Airway management of the pediatric patient differs significantly from that of one adult. What are the differences?
|
The trachea and larynx are soft and cartilaginous and will collapse with flexion or hyperextension.
|
|
|
Cuffed ET tubes are generally not used in children < _____________ years because why?
|
< 6 years of age
Narrowest portion of the airway is at the cricoid ring, forming a “physiological” cuff with the ET tube |
|
|
Assessment of respiratory status in children relies on what?
|
general appearance
-Note resp rate, level of consciousness, and use of accessory muscles |
|
|
_______________ is seen with extreme Hypoxia?
|
Bradycardia
|
|
|
As most masks are not tolerated by children, what is best method to provide Supplemental oxygen to a child?
|
Supplemental oxygen is best provided with “blow-by” since masks are not well tolerated by children.
|
|
|
gastric inflation occurs frequently in children during assisted or controlled ventilations with a face mask, especially when?
|
especially in the presence of partial airway obstruction.
|
|
|
You can minimize gastric distention during ventilations on a child by applying what?
|
applying Cricoid Pressure
-Infants- use (1) one fingertip -Children- use the thumb and index finger with children. |
|
|
what is the biggest red flag in a pediatric patient
and is most indicative of shock? |
Sustained Tachycardia
- This is b/c children have a limited capacity to vary stroke volume, so they must increase the heart rate to increase cardiac output |
|
|
If the child is Tachycardic, a _____________ _____________ is necessary to determine the cause.
|
Complete Assessment
|
|
|
why is Blood pressure extremely difficult to measure in children?.
|
The proper cuff size is often not available, making blood pressure measurement extremely inaccurate. Blood pressure is a poor indicator of shock because children have a great ability to constrict their blood vessels at the expense of peripheral perfusion.
|
|
|
Blood pressure is a poor indicator of shock in children because the have a great ability to do what?
|
constrict their blood vessels at the expense of peripheral perfusion.
|
|
|
Hypotension is a late and often ominous sign of cardiovascular collapse, as pediatric patients will generally not become hypotensive until when?
|
they have lost approximately 20% of their circulating volume.
|
|
|
All IV/IO’s established on Pediatrics < 8 y/o, must be administered with a desired amount prefilled into what?
|
a Soluset or 100cc Saline Bag.
|
|
|
Consider the use of a Aeromedical Service when presented with the following:
|
1. Multiple-system trauma patient with prolonged extrication and/or where a lengthy transport time may be required due to the hospital diversion status.
2. Multiple casualty incidents, where ground transport units are unable to manage and transport all patients in a timely manner. 3. Specific pediatric trauma patients who meet the following criteria: a. are required to be transported to a Pediatric Trauma Center b. may have a lengthy transport time. 4. Ventilation dependent or special needs children requiring transport to a specialized Pediatric Center. |
|
|
Transport decisions:
Specific pediatric trauma patients identified by Region III Guidelines (Section 814.000) must meet what criteria in order to consider the use of Aeromedical Service? |
a. are required to be transported to a Pediatric Trauma Center
b. may have a lengthy transport time. |
|
|
Transport Decisions:
who should you notify to request for air transport? -And what additional apparatus will be utilized? |
the Medical Supervisor and Battalion Chief
-Additional Engine to set up a LZ |
|
|
Transport Decisions:
What should you continue while waiting for helicopter arrival or rendezvous? |
Continue patient care and stabilization per SMO's
|
|
|
Transport Decisions:
Do not compromise time for invasive procedures other than airway. Most invasive procedures can be done when? |
while enroute to the trauma center.
|
|
|
For PEDIATRIC ALTERED MENTAL STATUS: What are the steps for treatment?
|
A) Level of consciousness and ABC’s
B) Provide Oxygen as needed. C) Suction as necessary. D) Assess circulation and perfusion. E) Perform glucose check. F) Begin Cardiac Monitoring, and evaluate EKG strip. G) Establish IV Normal Saline. H) Consider Narcan for any unconscious patient. I) Narcan 0.1mg/kg IV/IO/ETT ( 2mg max. >2yrs or 1mg max. < 2yrs ) J) Recheck glucose level after Five min |
|
|
Pediatric Altered Mental Status:
If blood sugar Less Than 60 mg/dl or Glucometer is unavailable and patient is symptomatic of Hypoglycemia: what do you give to a child in the age range of newborn to 2yrs old? |
5ml/kg of Dextrose 10% (Mix 2ml of Dextrose 50% with 8ml of Normal Saline)
|
|
|
Pediatric Altered Mental Status:
If blood sugar Less Than 60 mg/dl or Glucometer is unavailable and patient is symptomatic of Hypoglycemia: what do you give to a child in the age range of 2yr to 8yrs? |
2ml/kg of Dextrose 25% (Mix 10ml of Dextrose 50% with 10ml of Normal Saline)
|
|
|
Pediatric Altered Mental Status:
If blood sugar Less Than 60 mg/dl or Glucometer is unavailable and patient is symptomatic of Hypoglycemia: what do you give to a child in the age range of greater than 8yrs old? |
1ml/kg of Dextrose 50%
|
|
|
If blood sugar Less Than 60 mg/dl or Glucometer is unavailable and patient is symptomatic of Hypoglycemia, And you CANNOT get an IV, what should you do for the patient?
|
Glucagon 0.1ml/kg IM up to 1mg
|
|
|
Pediatric Altered Mental Status:
what medication should you consider for any unconscious patient? |
NARCAN
Narcan 0.1mg/kg IV/IO/ETT ( 2mg max. >2yrs or 1mg max. < 2yrs ) |
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the EYE OPENING Category?
|
SPONTANEOUS eye opening
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the EYE OPENING Category?
|
TO SPEECH
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the EYE OPENING Category?
|
TO PAIN
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the EYE OPENING Category?
|
NO RESPONSE FOR EYE OPENING
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the EYE OPENING Category?
|
SPONTANEOUS eye opening
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the EYE OPENING Category?
|
TO SPEECH
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the EYE OPENING Category?
|
TO PAIN
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the EYE OPENING Category?
|
NO RESPONSE FOR EYE OPENING
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 5 response in the VERBAL Category?
|
oriented
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the VERBAL Category?
|
CONFUSED
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the VERBAL Category?
|
INAPPROPRIATE WORDS
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the VERBAL Category?
|
NON SPECIFIC SOUNDS
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the VERBAL Category?
|
NO VERBAL RESPONSE
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 5 response in the VERBAL Category?
|
COOS, BABBLES
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the VERBAL Category?
|
IRRITABLE
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the VERBAL Category?
|
CRIES TO PAIN
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the VERBAL Category?
|
MOANS TO PAIN
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the VERBAL Category?
|
NO VERBAL RESPONSE
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 6 response in the MOTOR Category?
|
FOLLOWS COMMAND
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 5 response in the MOTOR Category?
|
LOCALIZES PAIN
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the MOTOR Category?
|
WITHDRAWS TO PAIN
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the MOTOR Category?
|
ABNORMAL FLEXION
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the MOTOR Category?
|
ABNORMAL EXTENSION
|
|
|
When determining the GCS for a VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the MOTOR Category?
|
NO MOTOR RESPONSE
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 6 response in the MOTOR Category?
|
NORMAL SPONTANEOUS MOVEMENTS
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 5 response in the MOTOR Category?
|
WITHDRAWS TO TOUCH
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 4 response in the MOTOR Category?
|
WITHDRAWS TO PAIN
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 3 response in the MOTOR Category?
|
ABNORMAL FLEXION
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 2 response in the MOTOR Category?
|
ABNORMAL EXTENSION
|
|
|
When determining the GCS for a PRE-VERBAL PEDIATRIC PATIENT, How would a patient receive a 1 response in the MOTOR Category?
|
NO MOTOR RESPONSE
|
|
|
Pediatric Obstructed Airway
If obstructed: 1 - 8 years what do you perform ? |
(5) five abdominal thrusts (Heimlich maneuver).
|
|
|
Pediatric Obstructed Airway
If obstructed: Less than 1 year perform what? |
(5) five back blows and (5) five chest thrusts
|
|
|
for Pediatric obstruction, what should you perform if a child is greater than 8 years?
|
Perform tongue-jaw-lift if child is greater than 8 years.
|
|
|
For Pediatric Obstruction (< 8 years old), you should perform a finger sweep only if __________________.
|
perform finger sweep only if object is visualized.
|
|
|
For Paramedics Only: Treating Pediatric Airway Obstruction,
If ventilation remains inadequate, what should you perform? |
perform direct laryngoscope and attempt to remove foreign body with suction and/or forceps.
|
|
|
Paramedic Only: treating pediatric airway obstruction,
-If the airway remains obstructed and/or patient is cyanotic, then perform what? |
ENDOTRACHEAL INTUBATION, Pre-Oxygenate and pretreat with Atropine 0.02 mg/kg IV and ventilate with BVM/100% Oxygen.
|
|
|
Pediatric Obstructed Airway:
What are the steps you should take if you are unable to intubate a pediatric patient? |
-Contact Medical Control for orders for needle
-Cricothyroidotomy. -Immediate Transport to NEAREST FACILITY -Establish IV with 20cc/kg bolus, if needed -IO if patient is less than 6 y/o and IV access cannot be obtained! |
|
|
Below what age should you put an IO in a pediatric patient when IV access cannot be established?
|
<6 years old
|
|
|
Is it ok to delay other assessment, treatment, or stay on the scene to secure an advanced airway?
|
NO, Absolutely Not
|
|
|
Pediatric advanced airway management:
-If the airway cannot be maintained by other means, including attempts at assisted ventilations, or if prolonged assisted ventilations are anticipated, what do you need perform ? |
Endotracheal Intubation
|
|
|
Pediatric Advanced Airway Management:
-ET tube size estimates can be based upon what? |
Broselow Tape, the size of the child’s little finger, or nares.
|
|
|
Pediatric Advanced Airway Management:
-What is the equation for the ET TUBE sizes? |
(16 + Age) divided by 4 = tube size
tube size x 3 = tube depth |
|
|
How would you PRE-TREAT a patient <2 years old thats about to have an advanced airway placed?
|
Atropine 0.02 mg/kg
|
|
|
Pediatric Advanced Airway Management:
-Proper ET tube placement should be confirmed by what? |
1. Listen to breath sounds (5 points).
2. Check pulse ox, ECG, and B/P for significant changes pre/post intubation and document. 3. Units that are equipped with LP12/15 monitors shall utilize the continuous End-Tidal CO² monitoring for all intubated patients. Pts should maintain Continuous End-Tidal CO2 levels of 35-45mmHg. |
|
|
Pediatric Advanced Airway Management:
If the patient has a suspected head injury, you should maintain an ETCO2 of _________________? |
Maintain ETCO2 (End Tidal CO2) of 30mmHg.
|
|
|
Pediatric Advanced Airway Management:
What should be utilized when failure to receive a capnography reading. |
the Encor CO2 detector should be utilized. The Encor detector must remain on the tube and confirmed by a physician before transfer of patient from our stretcher.
|
|
|
Pediatric Advanced Airway Management:
You must document depth of ETT at what level? |
at the level at the teeth
|
|
|
Pediatric Advanced Airway Management:
Units that are not equipped with LP12’s shall first utilize the Encor CO² detector then utilize what? |
The LP12 continuous End tidal CO² monitoring.
|
|
|
What should the Encor CO2 detector reflect when placed on the tube?
-When documenting this value, what else should you document? |
2-5% YELLOW
-Depth at the Teeth, LEMON, & Cormack-Lehane Grade View |
|
|
If all other attempts to resuscitate the patient have failed and the patient still displays respiratory depression, consider ______________________.
|
NARCAN
- 0.1mg/kg IV/IO/ETT ( 1mg max. less than 2yrs or 2mg max. greater than 2yrs) for continued respiratory depression |
|
|
In a Pediatric Patient with Respiratory Arrest, __________________ may develop after resuscitative efforts have begun.
|
Tension Pneumothorax
|
|
|
Pediatric Advanced Airway Management:
-If Tension Pneumothorax is suspected, What should you consider? |
Needle Decompression
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation:
-If unable to intubate a conscious medical or trauma patient that meets the following criteria, you may administer Sedation Assisted Intubation. |
1. Patient who cannot maintain their airway
2. Patient who cannot protect their airway 3. Patient who cannot be appropriately ventilated or be oxygenated with BVM or other means |
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (TRAUMA)
What is the order of drug administration for SAI? |
1. Atropine (<2 y/o) = 0.02 mg/kg -> 2 mins before intubation.
2. Lidocaine (1 mg/kg IVP/IO) -> Must circulate for 2 minutes and can be given at same time as Atropine. 3. Fentanyl (2 mcg/kg SLOW IO/IVP) 4. Etomidate (0.3 mg/kg SLOW IO/IVP) -> OVER 30 SECONDS |
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (TRAUMA)
-Pediatric TRAUMA: What dose of Atropine is given to a child less than 2 years of age? |
Atropine - (less than 2 years of age) - 0.02mg/kg IVP/IO (Must be given AT LEAST 2 minutes prior to intubation) Minimum dose 0.1mg
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (TRAUMA)
-What dose of Lidocaine should be given ? |
Lidocaine - 1 mg/kg IVP/IO (Given 2minutes prior to intubation and can be given at same time as Atropine)
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (TRAUMA)
-What dose of Fentanyl should be given? |
Fentanyl - 2mcg/kg SLOW IVP/IO
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (TRAUMA)
-What dose of Etomidate should be administered? |
Etomidate: 0.3 mg/kg SLOW IVP/IO ( over 30 seconds)
*post intubation sedation (hemodynamic stable) |
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (MEDICAL)
What is the order of drug administration for SAI? |
1. Atropine (less than 2 years of age) -0.02mg/kg IVP/IO (Must be given at least 2 minutes prior to intubation) Minimum dose 0.1mg.
2. Fentanyl 2mcg/kg slow IVP/IO 3. Etomidate 0.3mg/kg slow IVP/IO (Over 30 seconds) |
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (MEDICAL)
-What dose of Atropine should be given to a child less than 2 years of age? |
Atropine (less than 2 years of age) -0.02mg/kg IVP/IO (Must be given at least 2 minutes prior to intubation) Minimum dose 0.1mg
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (MEDICAL)
-What dose of Fentanyl should be given to a child? |
Fentanyl 2mcg/kg SLOW IVP/IO
|
|
|
Pediatric – (SAI) Sedation Assisted Intubation: (MEDICAL)
-What dose of Etomiate should be given to a child? |
Etomidate 0.3mg/kg SLOW IVP/IO (Over 30 seconds)
*post intubation sedation (hemodynamic stable) |
|
|
For Medical and Trauma SAI -
-How do you perform (Post Intubation Sedation) for a patient that is Hemodynamically Stable / Hemodynamically Unstable? |
Hemodynamically Stable - 0.1 mg/kg VERSED IVP/IO (1 DOSE ONLY)
Hemodynamically Unstable - Contact Med Control |
|
|
Pediatric – (SAI) Sedation Assisted Intubation:
-Etomidate is not recommended for routine use in pediatric patients with evidence of what? |
Septic shock
|
|
|
Describe Croup Symptoms
|
• 3 months to 3 years
• Rapid Onset • Child may lie or sit upright • Barking cough • Lack of drooling • Temperature Less Than 104 F |
|
|
Pediatric Croup:
-If the patient is still Ventilating Adequately, should you attempt to visualize the airway of the Child? |
NO, LEAVE HIM BE!
-you will upset the patient and exacerbate the s/s |
|
|
Pediatric Croup:
-What should you administer 1st by blow by mask at 10 LPM unless it provoke agitation? |
Nebulized treatment of 6 ml of Normal Saline
|
|
|
Pediatric Croup:
-What do you NOT ATTEMPT in a patient with croup? |
DO NOT ATTEMPT IV ACCESS!
|
|
|
Pediatric Croup:
-Prepare appropriate size airway equipment and observe for pending respiratory failure. What are the 8 signs to observe for? |
1. Sleepy, intermittently combative, or agitated.
2. Increased respiratory effort at sternal notch. 3. Marked use of accessory muscles. 4. Retraction, head bobbing, grunting. 5. Central Cyanosis. 6. Marked Tachycardia. 7. Poor Peripheral perfusion. 8. Decreased muscle tone. |
|
|
Pediatric Croup:
-For a Patient with Croup, When would you consider assisting ventilations with 100% Oxygen via BVM |
When the Child becomes:
-Exhausted -Bradycardic and/or -Respirations Decrease |
|
|
Pediatric Croup:
-What medication is given to a child who has SEVERE CROUP? |
For severe Croup administer 0.5 mg/5ml Aerosolized Epinephrine (1:10,000)
|
|
|
Pediatric Croup:
-If a child progresses to Respiratory Arrest, you should do what? |
1. Attempt to intubate
2. If intubation is unsuccessful and the child cannot be adequately ventilated with a BVM: *Contact Medical Control TO PERFORM NEEDLE CRICOTHYROTOMY - (RARE). |
|
|
Pediatric Epiglottitis:
-What are Epiglottitis symptoms? |
• 3 to 7 years
• Slow onset • Child prefers to sit up, leaning forward • No barking cough, possible inspiratory strider • Drooling, pain during swallowing • Temperature Greater Than 104 F |
|
|
Pediatric Epiglottitis:
-If the patient is still Ventilating Adequately, should you attempt to visualize the airway of the Child? |
NO, LEAVE HIM BE!
-you will upset the patient and exacerbate the s/s |
|
|
Pediatric Epiglottitis:
-Who should you contact when a child is suspected epiglottitis? -And what should you do first? |
Contact Medical Control - so that appropriate personnel and resources can be made available
-Administer supplemental Oxygen by mask at 15 LPM unless it provokes agitation. Consider “blow-by” Oxygen while child sits. |
|
|
Pediatric Epiglottitis:
-Is it ok to attempt an IV on a patient with suspected Epiglottitis? |
NO!
-You will upset the patient and exacerbate the s/s |
|
|
Pediatric Epiglottitis:
-Prepare appropriate size airway equipment for a child with epiglottitis and observe for PENDING RESPIRATORY FAILURE: what are the 8 signs to observe for? |
1. Sleepy, intermittently combative, or agitated.
2. Increased respiratory effort at sternal notch. 3. Marked use of accessory muscles. 4. Retraction, head bobbing, grunting. 5. Central Cyanosis. 6. Marked Tachycardia. 7. Poor Peripheral Perfusion. 8. Decreased muscle tone. |
|
|
Pediatric Epiglottitis:
-For a Patient with EPIGLOTTITIS, When would you consider assisting ventilations with 100% Oxygen via BVM |
When the Child becomes:
-Exhausted -Bradycardic and/or -Respirations Decrease |
|
|
Treating a child with Epiglottitis, a paramedic should do what 2 things if a child progresses to Respiratory Arrest?
|
1. Attempt to intubate
2. If intubation is unsuccessful and the child cannot be adequately ventilated with a BVM *CONTACT MEDICAL CONTROL to perform Needle Cricothyrotomy - (RARE) |
|
|
Pediatric Asthma:
-What do you do if breathing is adequate? |
Provide Oxygen as needed.
a. Use a NRB mask or BLOW-BY as tolerated. b. Monitor Pulse Oximetry. c. If Level of Consciousness is decreased, then provide 100% Oxygen / BVM with assisted ventilations as needed. d. Consider need for EARLY INTUBATION e. To prevent barotrauma secondary to hyperinflation, deliver decreased tidal volumes at a rate 12 to 20/min and allow for prolonged expiratory time. |
|
|
For Pediatric Asthma :
-What are the steps taken to treat this patient? |
A) If breathing is adequate:
• Provide Oxygen as needed. B) Assess Circulation and Perfusion. C) Assess Mental Status. |
|
|
Pediatric Asthma:
-EMT-I Function- For MILD Exacerbation, what meds should be given? |
Administer
-Nebulized Albuterol 5.0 mg & Atrovent 0.5 mg. *May repeat x2 every 15mins |
|
|
Pediatric Asthma:
-EMT-I Function - for MODERATE to SEVERE Exacerbation, what meds should be given? |
Administer nebulized Albuterol 5.0mg & Atrovent 0.5mg
|
|
|
Pediatric Asthma:
-Paramedic Function - what should a Paramedic administer for MILD Exacerbation? |
Administer Solu-Medrol 1mg/kg up to 125mg.
|
|
|
Pediatric Asthma:
-Paramedic Function - what should a Paramedic administer for SEVERE cases when Albuterol is not effective? |
Administer Aerosolized Epinephrine 1:10,000, 0.5mg/5ml
|
|
|
Pediatric Asthma:
-If a patient is UNABLE TO COOPERATE with aerosol treatment and shows signs of Respiratory Failure what are the next steps for treatment? |
1. Administer Epinephrine 0.01mg/kg (1:1,000) IM.
2. May repeat x 1 in 20 minutes 3. MEDICAL CONTROL OPTION - Mag Sulfate 40 mg/kg 4. Cardiac Monitor 5. Expose the patient only as necessary to perform further assessment 6. Maintain body temperature 7. perform focused history and detailed exam en route. 8. Contact Medical Control if additional instructions are needed. |
|
|
Pediatric Asthma:
What is a Medical Control option for treatment? |
Magnesium Sulfate 40mg/kg
|
|
|
Pediatric Allergic Reaction:
-If a patients breathing is adequate you should what? |
Provide Oxygen as needed.
1. Use a NRB mask or blow-by as tolerated. 2. Monitor Pulse Oximetry. |
|
|
Pediatric Allergic Reaction:
-What steps should you take in treating a pediatric patient with an allergic reaction? |
1. Assess Circulation and Perfusion.
2. Establish IV Normal Saline and 20ml/kg bolus as needed. 3. Begin Cardiac Monitoring, record, and evaluate EKG strip. 4. Expose the patient only as necessary to perform further assessments. 5. Maintain the patient’s body temperature throughout the examination. |
|
|
Pediatric Allergic Reaction:
-What medications can an EMT-I administer to a pediatric pt w/ allergic reaction? |
- Epi Auto Injector 0.15cc - Adult & Pedi IM 1:1000.
-May repeat after 10 minutes with Medical Control Orders. |
|
|
Pediatric Allergic Reaction:
What 3 medications are generally given by a paramedic to a pediatric with an allergic reaction? |
Epinephrine
Benadryl Solu-Medrol |
|
|
Pediatric Allergic Reaction:
-Paramedic - what is the dose of Epi that can be administered? |
Administer Epinephrine 0.01mg/kg (1:1,000) IM
1. Massage injection site vigorously for 30-60 sec. 2. If intubated, administer Epinephrine 0.1mg/kg (1:1,000) ETT. |
|
|
Pediatric Allergic Reaction:
-Paramedic - What is the dose of Benadryl that can be administered? -What can be administered after Benadryl? |
-Benadryl 1mg/kg
-(MAX. Individual dose - 50mg) IV or DEEP IM. -Solu-Medrol 1 mg/kg or up to 125 mg Slow IVP |
|
|
Pediatric Allergic Reaction:
-If bronchospasm is present in a patient with adequate ventilation, you should administer what? |
-Albuterol 5.0mg & Atrovent 0.5 mg via Nebulizer
-Over 10-15 minutes. -May Repeat x 1. |
|
|
Pediatric Seizures:
-What steps should be taken to treat the patient? |
A) LOC and ABC’s
B) Perform glucose check. C) Begin Cardiac Monitoring, record, and evaluate EKG strip. D) Establish IV Normal Saline / INT E) Obtain focused history: F) Perform auxiliary temperature check. |
|
|
Pediatric Seizure:
-When is it ok to obtain an IO on a Seizing Patient? |
-Nasal Versed does not control the seizure activity.
-Patient is HYPOXIC, less than 6 years old and IV access can not be obtained |
|
|
Pediatric Seizures:
if a pediatric patients temperature is greater than 102 degrees, you should administer what? |
Acetaminophen (Tylenol) - 15 mg/kg PO if patient is awake and cooperative.
|
|
|
What should you do for evidence of fever in a Seizing patient?
-What is the Initial Care? |
For evidence of fever, remove excessive clothing and begin gradual cooling. Place moistened towels in axilla and groin but avoid excessive cooling and shivering.
|
|
|
Pediatric Seizures: (STATUS EPILEPTICUS)
-Paramedic Function - If the pt has 2 or more seizures WITHOUT a lucid interval or continuous seizure lasting greater than 5 minutes, what should you give? |
-Administer Ativan 0.1 mg/kg slow IV push
-(Up to 2 mg.) - If seizures persist, administer Ativan 0.1mg/kg slow IV push up to 2mg |
|
|
Pediatric Seizures:
Paramedic Function - What is the administration procedure of medication if NO IV is established? |
Load syringe with appropriate milliliter volume of Versed (use only 5 mg/ml concentration) and attach MAD Nasal Atomizer. Administer Versed 0.2 mg/kg IN
|
|
|
Pediatric Seizures:
Paramedic Function - How do you administer an MAD Nasal Atomizer of Versed? |
1) Place atomizer within the nostril and briskly compress syringe to administer 1/2 of the volume as atomized spray.
2) Remove and repeat in other nostril, so all the medication is administered. 3) If seizures persist 5 minutes after treating, consider repeating 1/2 dose of Versed either intranasally or intravenously. |
|
|
Pediatric Drug Overdose and Poisoning.
-What is the first thing you should do? |
Contact Poison Control (1-800-222-1222).
|
|
|
Is it ok to expose a patient that is suspected of Child Abuse and/or Neglect?
-How should your treatment for this patient be performed? |
Only as necessary to perform assessments
-Treat obvious injuries |
|
|
Suspected Child Abuse and Neglect:
-Physical abuse and neglect is often difficult to determined. You should do what to treat the patent? |
Note and document unexplained injuries, discrepant history, delays in seeking medical care, and repeated episodes of suspicious injuries.
|
|
|
Suspected Child Abuse and Neglect:
-What are the indicators of possible abused? |
1. Any obvious or suspected fracture in a child less than 2 years of age.
2. Injuries in various stages of healing, especially burns and bruises. 3. More injuries than are usually seen in other children of the same age. 4. Injuries scattered on many areas of the body. |
|
|
Suspected Child Abuse and Neglect:
-If abuse is suspected, who should you contact ? |
Contact a Medical Supervisor
|
|
|
Suspected Child Abuse and Neglect:
-If a patient has not changed clothes, transport the child in clothes in which the child was assaulted. -If clothes have been removed but unwashed, what do you do? |
Bring clothes and underwear with child in a PAPER BAG, (not plastic).
Do not delay transport to search for evidence. |
|
|
Suspected Child Abuse and Neglect:
-If a parent refuses to let you transport the child after treatment is given, what professional steps should you take? |
1. Remain at the scene and notify law enforcement.
2. Request law enforcement place the child in protective custody. 3. Contact Medical Control and advise Doctor of questionable injuries but DO NOT report CHILD ABUSE AND NEGLECT over the radio. |
|
|
Suspected Child Abuse and Neglect:
-ARE YOU ARE LEGALLY RESPONSIBLE for reporting your suspicions? |
YES
|
|
|
Suspected Child Abuse and Neglect:
-While treating a patient with suspected abuse, you should document what? |
-Document any statement the child makes in the child’s own words.
-Document history, physical exam findings, environmental surroundings, and ED notification in the Patient Care Report. |
|
|
Pediatric Trauma and Management:
-The general approach to the pediatric trauma patient Is the same as for adult trauma. what does the approach include? |
-Cervical Spine Control
-ABCD -Head-to-Toe Examination. |
|
|
Where should Pediatric Trauma Patient be transported and according to what guidelines?
|
-Pediatric Trauma Patients should be transported to Pediatric Trauma Centers.
-Per Georgia Region III Guidelines. |
|
|
Scottish Rite does not accept patients with what type
of trauma? |
Thoracic trauma
|
|
|
What are the 2 Metro Atlanta Pediatric trauma center?
|
a. Children’s Healthcare of Atlanta at Egleston
b. Children’s Healthcare of Atlanta at Scottish Rite |
|
|
Pediatric Trauma and Management:
Cervical spine fractures are uncommon in children. What steps should be taken to treat a child with this condition? |
1. The cervical spine of the pediatric patient is best immobilized with the Pediatric Immobilization Device (PID). You must fill all void spaces to secure the cervical alignment.
2. The cervical spine of the awake, frightened toddler, must be immobilized with great care to avoid further damage resulting from the child’s resistance to the procedure. 3. If the mechanism of injury meets any criteria listed in Section 814.001 the patient must be treated as having a suspected cervical injury and must be immobilized. 4. If an infant is stable and no cervical injury is suspected, the child may be transported in his/her car seat secured to the stretcher. |
|
|
What is the Age Limit for the usage of the Pediatric Field Triage Guide?
|
Up to the 15th Birthday
|
|
|
Section 814.001- Pediatric Field Triage Guide (up to the 15th birthday) - STEP 1 Consists of 16 different criteria. If yes to any of them, transport patient to a pediatric trauma center. Name these criteria.
-STEP 1 |
A) Glascow Coma Scale (modified for pre-verbal children) less than 14
B) Systolic Blood Pressure Less Than 90 C) Respiratory Rate Less Than 10 or in distress D) Pediatric Trauma Score Less Than 8 E) Need for any airway adjunct F) Need for fluid resuscitation to support heart rate, peripheral perfusion and/or central pulses G) Cardiac arrest or CPR performed prior to arrival with return of spontaneous circulation H) All penetrating injuries to the head, neck, torso, and extremities proximal to elbow or knee I) Open/Sucking chest wound J) Combination trauma with burns K) Two or more proximal long bone fractures L) Pelvic Fractures M) Open and depressed skull fractures N) Spinal injury with paralysis or any neurologic deficit O) Amputation proximal to wrist and ankle P) Burns greater than 15% BSA or with airway involvement, greater than 20 minute transport time to Grady **If answers to the above are no, go to SMO section 814.002 step 2 |
|
|
Section 814.002 - Pediatric Field Triage Guide (up to the 15th birthday) STEP 2 consists of 16 different criteria. If yes to any of them contact PCT for on-line Medical Control and determination of destination.
-STEP 2 |
A) Head injury with any loss or alteration of consciousness
B) Spinal injury with risk of paralysis or neurologic deficit C) Blunt chest trauma with contusion or tenderness, or with potential for D) Hemo/Pneumothorax E) Blunt abdominal trauma with contusion, tenderness, or distention F) De-gloving injury of extremity or laceration greater than 7cm G) Penetrating wound involving joint and/or significant vascular injury H) Ejection from automobile I) Death in passenger compartment J) Extrication time greater than 20 minutes K) Falls greater than 20 feet L) Rollover M) High speed auto crash: initial speed greater than 40mph, major auto deformity greater than 20 inches N) Passenger space intrusion greater than 12 inches O) Auto-Pedestrian/auto-bicycle injury with significant impact greater than 20 mph P) Motorcycle crash greater than 20 mph or with separation of rider from bike |
|
|
What are the Pediatric Field Triage Guide EXCEPTIONS?
|
Presence of one of the following conditions requires transport to the nearest facility:
A) continuing cardiac arrest due to penetrating trauma B) continuing cardiac arrest due to blunt trauma C) inability to establish patent airway D) unstable blood pressure |
|
|
What are the steps to follow for Pediatric
Bradycardia ALS Care? |
Pediatric Bradycardia ALS Care
A) LOC and ABC’s B) Manage Airway and Oxygen C) IV/IO Normal Saline KVO D) Begin Cardiac Monitoring, record, and evaluate EKG strip. E) Evaluate for severe cardio-respiratory compromise. F) Perform chest compressions, if despite oxygenation and ventilation heart rate remains less than 60/min. infant or child. G) If asystole develops, see SMO Section 816.000 H) Consider treatment of specific cause if persists despite: 1. Adequate ventilation and oxygenation: 2. Hypoglycemia 3. Severe acidosis 4. Consider fluid challenge, NS 20cc/kg I) Review history |
|
|
What medication should you administer for Pediatric Bradycardia ALS care and what dose?
|
-Epinephrine 0.1ml/kg, 0.01mg/kg (1:10,000) IV/IO OR -
-Epinephrine 0.1ml/kg, 0.1mg/kg (1:1,000) ETT with 5ml flush. -Repeat every 3-5 minutes -Atropine 0.2ml/kg - (0.02mg/kg) - IV/IO OR Atropine 0.4ml/kg (0.04mg/kg) ETT with 5ml flush. -Repeat every 3-5 minutes -Atropine Minimum dose – 1ml (0.1mg) Atropine -Maximum dose – 5ml (0.5mg) for child and 10ml (1mg) for adolescent -May repeat x 1 |
|
|
You should consider treatment of specific cause, if what conditions should persist regarding ALS care?
|
1. Adequate ventilation and oxygenation:
2. Hypoglycemia 3. Severe acidosis 4. Consider fluid challenge, NS 20cc/kg |
|
|
what steps would you take or treating Asystole / Pulseless electrical Activity?
|
A) LOC and ABC’s
B) Manage Airway and Oxygen C) Begin CPR, per ASHI Guidelines D) Begin Cardiac Monitoring, record, and evaluate EKG strip. E) IV/IO Normal Saline KVO *Consider Normal Saline 20cc/kg Bolus |
|
|
identify and treat the cause of Asystole/Pulseless electrical activity What steps ?
|
1. Severe Hypoxemia- Oxygen / BVM
2. Severe Acidosis- Sodium Bicarb 3. Severe Hypovolemia- Fluids 4. Tension Pneumothorax - Decompress 5. Profound Hypothermia - Rewarm 6. Cardiac Tamponade - Pericardiocentesis |
|
|
What medications are give for a patient with Asystole?
|
Epinephrine 0.01mg/kg (1:10,000) IV/IO OR
-ETT -First Dose Epinephrine 0.1ml/kg, 0.1mg/kg (1:1,000) ETT with 5ml flush. |
|
|
Pedi Asystole/PEA:
What is the second & subsequent dose of Epinephrine? |
Second and subsequent doses Epinephrine 0.1ml/kg, 0.1mg/kg (1:1,000) IV/IO or ETT with 5ml flush.
• Repeat every 3-5 minutes |
|
|
What are the steps in Managing and Treatment of Pediatric VFIB and Pulseless VTAC?
|
A) LOC and ABC’s
B) Manage Airway and Oxygen C) CPR for 2 minutes D) Begin Cardiac Monitoring, record, & evaluate EKG strip. E) Defibrillate at 2 joules/kg F) CPR for 2 minutes G) Pulse check H) IV/IO Normal Saline KVO I) Epinephrine 0.1ml/kg, 0.01mg/kg (1:10,000) IV/IO OR J) Epinephrine 0.1ml/kg, 0.1mg/kg (1:1,000) ETT with 5ml flush • Repeat every 3-5 minutes K) Defibrillate at 4 joules/kg L) Cordarone 5 mg/kg IV/IO with 300 mg maximum M) Continue CPR N) Defibrillate at 4 joules/kg O) Epinephrine 0.1ml/kg, 0.01mg/kg (1:10,000) IV/IO P) Continue CPR Q) Defibrillate at 4 joules/kg R) Cordarone 2.5mg/kg IV/IO with 150mg maximum S) Continue CPR T) Defibrillate at 4 joules/kg U) Epinephrine 0.1ml/kg, 0.01mg/kg (1:10,000) IV/IO V) Continue CPR W) Defibrillate at 4 joules/kg X) Consider other Anti-Fibrillatory Measures: (Lidocaine 1mg/kg) |
|
|
In Pediatric Nausea/Vomiting:
-If breathing is adequate what should be done? |
• Provide Oxygen as needed.
1. Use a NRB mask or blow-by as tolerated. 2. Monitor Pulse Oximetry. |
|
|
After providing treatment for adequate breathing what should the next 7 steps taken in treating
Pediatric Nausea/vomiting? |
1 Assess circulation and perfusion.
2 Establish IV Normal Saline and 20ml/kg bolus as needed. 3 Begin Cardiac Monitoring, record, and evaluate EKG strip. 4 Expose the patient only as necessary to perform further assessments. 5 Maintain the patient’s body temperature throughout the examination. 6 Perform glucose check. 7 Consider causes |
|
|
what can a paramedic administer to a Pediatric Patient who is experiencing Nausea/Vomiting?
|
-For cases of severe Nausea/Vomiting with patient’s ≥ 2 years of age:
-Administer 0.1mg/kg Zofran IVP (max dose 4mg). |
|
|
What can the **MEDICAL CONTROL** advise you to administer to a patient less than 2 years old?
|
Zofran Administration for patients < 2 yrs. Old.
|
|
|
When establishing an IV on a pediatric patient under the age of 8 you must utilize a ____________.
A. 60 gtts set B. Solu-Set C. pressure infusion bag D. 22 or 24 gauge needle SMO 801.000 D3 |
B. Solu-Set
|
|
|
What is the proper mixture for Dextrose 10%?
A. 10 mL D50 with 20 mL NS B. 10 mL D50 with 10 mL NS C. 8 mL D50 with 2 mL NS D. 2 mL D50 with 8 mL NS SMO 803.000 E1 |
D. 2 mL D50 with 8 mL NS
-Use a flush and spray out 2 ml of Saline; you should then fill up that remaining 2 ml with D50 |
|
|
What is the pediatric dose for Narcan?
A. 0.1 mg/kg B. 0.2 mg/kg C. 1 mg/kg D. 2 mg/kg SMO 803.000 I |
A. 0.1 mg/kg
|
|
|
What are the four ways to determine ETT size in a pediatric patient?
_ _ _ _ SMO 806.002 B |
-Age + 16 / 4
-Broselow Tape -Nare Size -Pinky Size |
|
|
What is the max dose of Narcan in a child less than 2 years old?
A. 1 mg B. 2 mg C. 3 mg/kg D. 0.4 mg SMO 806.002 G |
A. 1 mg
|
|
|
When performing SAI on the pediatric patient you must pre-treat with Atropine at what dose?
A. 0.5 mg/kg B. 0.01 mg/kg C. 0.02 mg/kg D. 0.75 mg/kg SMO 806.003 B1 |
C. 0.02 mg/kg
|
|
|
What is your treatment for a patient suffering from severe croup?
A. 1 mg/kg Benadryl IV B. 1 mg/k Solu Medrol IV C. 0.5 mg Aerosolized Epinephrine 1:10,000 D. 0.5 mg Aerosolized Epinephrine 1:1,000 SMO 807.000 |
C. 0.5 mg Aerosolized Epinephrine 1:10,000
|
|
|
What is the dose of Albuterol for a 10 YOM asthma patient?
A. 1 mg/kg B. 0.5 mg/kg C. 2.5 mg D. 5 mg SMO 808.000 D1 |
D. 5 mg
|
|
|
You are on scene with a 6 YOF patient suffering from an allergic reaction from a bee sting. After establishing an IV, what is the dose of Benadryl you would administer?
A. 0.5 mg/kg B. 1 mg/kg C. 25 mg D. call medical control SMO 809.000 J |
B. 1 mg/kg
|
|
|
You are on scene with a 3 YOM patient with an axillary temperature of 104˚F. What is the dose of Acetaminophen you would administer this patient?
A. 1 mg/kg B. 5 mg/kg C. 10 mg/kg D. 15 mg/kg SMO 810.000 G |
D. 15 mg/kg
-325 mg in 10.15 ml -325 / 10.15 = 32mg's per 1 mL -Example: -Pt weighs 25 lbs = 11.4 Kg's -15 x 11.4 = 171 mg's needed - 171 / 32 = 5.3 mL's Administered |
|
|
You are on scene with an 8 YOF patient suffering from recurrent seizures. You are unable to establish IV or IO access. What drug would administer and at what dose Intra Nasal?
A. Versed 0.2 mg/kg B. Tylenol 10 mg/kg C. Ativan 0.1 mg/kg D. none of the above SMO 810.000 H4 |
A. Versed 0.2 mg/kg
|
|
|
Does Scottish Rite accept patients with thoracic trauma? If Not, Why???
A. Yes B. No SMO 813.000 B |
B. They don't accept Thoracic Trauma Patients
-They ARE NOT the Designated Pedi Hospital in Metro Atlanta |
|
|
Does Egleston accept patients with thoracic trauma? If no, why???
A. Yes B. No |
A. Yes
-Egleston will accept all patients, because THEY ARE THE DESIGNATED PEDI TRAUMA HOSPITAL IN METRO ATLANTA. |
|
|
The Pediatric Field Triage Guide is valid up to the pediatric patient’s____________ birthday.
A. 15th B. 16th C. 17th D. 18th SMO 814.001 |
A. 15th
|
|
|
You are working a 4 YOM in cardiac arrest. The patient is on the cardiac monitor showing asystole. CPR is in progress and ventilations are being performed. IO access is established. What is your dose of Epinephrine 1:10,000?
A. 0.2 mg/kg B. 0.02 mg/kg C. 0.1 mg/kg D. 0.01 mg/kg SMO 816.000 G |
D. 0.01 mg/kg of 1:10,000 Epi
|
|
|
You are working a pediatric arrest on a 7 YOF that weighs 50 pounds. You note the cardiac monitor is showing V-Fib. Your partner placed the pads on the patient. How many joules do you defibrillate for your initial shock?
A. 50 B. 45 C. 120 D. 90 SMO 817.000 E |
-Dose of Joules = 2 joules/kg #1
-Dose of Joules = 4 joules/kg #2,3,4… -50 lbs = 22.5 kg's Dose |
|
|
What is the dose of Cordarone in a pediatric patient showing pulseless V-Tach on the monitor.
A. 1 mg/kg B. 2 mg/kg C. 5 mg/kg D. 150 mg SMO 817.000 L |
C. 5 mg/kg
|
|
|
You are working a pediatric arrest showing PEA on the monitor at a rate of 70 bpm. What is your dose of Atropine?
A. 1 mg B. 0.02 mg/kg C. 0.01 mg/kg D. you do not administer Atropine in pediatric PEA SMO 816.000 |
B. 0.02 mg/kg
|
|
|
You have gained IV access in a 10 YOM patient suffering from recurrent seizures. What medication and dose are you going to administer?
A. Ativan 0.1 mg/kg SIVP B. Versed 0.1 mg/kg IN C. Ativan 0.1 mg/kg RIVP D. Ativan 0.2 mg/kg SIVP SMO 810.000 H1 |
A. Ativan 0.1 mg/kg SIVP
|
|
|
You have a 6 YOF patient suffering from a moderate case of croup. What is your first-line treatment?
A. 5 mL Aerosolized Epinephrine 1:10,000 B. 6 mL Aerosolized Normal Saline C. 5 mL Aerosolized Epinephrine 1:1,000 D. 0.01 mg/kg Epinephrine 1:1,000 IM SMO 807.000 B |
B. 6 mL Aerosolized Normal Saline
|
|
|
You are on scene with a 7 YOM patient suffering from low blood sugar. He exhibits an altered mental status with a D-stick of 32. You are able to obtain IV access. What would your most appropriate medication be?
A. 5 mL/kg D10 B. 2 mL/kg D25 C. 1 mL/kg D50 D. 0.1 mg/kg Glucagon SMO 803.000 E |
B. 2 mL/kg D25
|
|
|
ETT depth is calculated by multiplying the tube length by_____________.
A. 1 B. 2 C. 3 D. 4 SMO 806.002 B2 |
C. 3
|
|
|
Personnel must receive orders from Medical Control for needle cricothyroidotomy.
A. True B. False SMO 806.002 E2 |
A. True
|
|
|
The ideal end-tidal CO2 readings for an intubated pediatric patient are between __________and__________.
A. 35-50 B. 30-40 C. 25-45 D. 35-45 SMO 806.002 C3 |
D. 35-45
|
|
|
. If you transport a pediatric to the hospital who is the first person you should notify if you suspect child abuse?
A. ER nurse B. TAC 2 operator C. MS officer D. the parent SMO 812.000 G3 |
A. ER nurse
|
|
|
Perform chest compressions, if despite oxygenation and ventilation heart rate remains less than _________ bpm in infant or child.
A. 100 B. 60 C. 120 D. 80 SMO 815.000 F |
B. 60
|
|
|
Fill in the blanks for traumatic pediatric SAI patient.
Atropine ________mg/kg if <2 y/o Given_________minutes prior to intubation Minimum dose __________mg ___________1 mg/kg – IVP/IO Given 2 minutes prior to intubation and can be given at the same time as Atropine Fentanyl __________mcg/kg- IVP/IO ________________0.3 mg/kg SIVP/IO Post Intubation sedation (hemodynamic stable) 0.1 mg/kg __________IVP/IO X 1 dose What should you do for Post Intubation sedation (hemodynamic unstable)? SMO 806.003 |
-0.02 mg/kg
-2 minutes -0.01 mg -Lidocaine -2 Mcg/kg -Etomidate -Versed -Contact Med Control |
|
|
What are the components of the Pediatric Trauma Score?
|
-Weight
-Airway -Systolic B/P -Level of Consciousness -Open Wounds -Fractures |
|
|
Pediatric Trauma Score
How would you get a +2 in the Weight Category? |
> 20 kg or ( > 44lb)
Same thing |
|
|
Pediatric Trauma Score
How would you get a +1 in the Weight Category? |
10 - 20 kg or (22 - 44 lbs)
Same thing |
|
|
Pediatric Trauma Score
How would you get a -1 in the Weight Category? |
< 10 kg or (<22 lbs)
Same thing |
|
|
Pediatric Trauma Score
How would you get a +2 in the Airway Category? |
Normal Airway
|
|
|
Pediatric Trauma Score
How would you get a +1 in the Airway Category? |
Assisted Airway or Breathing
|
|
|
Pediatric Trauma Score
How would you get a -1 in the Airway Category? |
Advanced Airway
|
|
|
Pediatric Trauma Score
How would you get a +2 in the Systolic B/P Category? |
>90 mm Hg
-Good peripheral pulses and perfusion |
|
|
Pediatric Trauma Score
How would you get a +1 in the Systolic B/P Category? |
-50-90 mmHg
-Central pulses present -Peripheral pulses thready or absent |
|
|
Pediatric Trauma Score
How would you get a -1 in the Systolic B/P Category? |
<50mmHg
-Thready to absent central pulses |
|
|
Pediatric Trauma Score
How would you get a +2 in the Level of Consciousness Category? |
Awake, alert
-Peds GCS = 15 |
|
|
Pediatric Trauma Score
How would you get a +1 in the Level of Consciousness Category? |
-Less than fully awake, but not comatose
-Peds GCS = 9-14 -Any History of LOC |
|
|
Pediatric Trauma Score
How would you get a -1 in the Level of Consciousness Category? |
Comatose
-Peds GCS <8 |
|
|
Pediatric Trauma Score
How would you get a +2 in the Open Wounds Category? |
None
|
|
|
Pediatric Trauma Score
How would you get a +1 in the Open Wounds Category? |
-Contusions
-Abrasions -Lacerations <7cm |
|
|
Pediatric Trauma Score
How would you get a -1 in the Open Wounds Category? |
Tissue loss, exposed, muscle/fascia or any penetrating injury.
|
|
|
Pediatric Trauma Score
How would you get a +2 in the Fractures Category? |
None
|
|
|
Pediatric Trauma Score
How would you get a +2 in the Fractures Category? |
Single Closed Fracture
|
|
|
Pediatric Trauma Score
How would you get a +2 in the Fractures Category? |
Open and/or MULTIPLE
|
|
|
On the Pediatric Pain Score (Smiley Faces - Wong Baker Scale) -
-What do each of the values represent? |
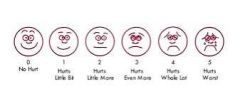
0- NO HURT
2- HURTS A LITTLE BIT 4- HURTS LITTLE MORE 6- HURTS EVEN MORE 8- HURTS WHOLE LOT 10- HURTS WORST |

