![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
244 Cards in this Set
- Front
- Back
|
what is the duration of action of mepivacaine in paralumbar nerve block? |
1.5h |
|
|
what is the preferred technique for suturing up the rumen? |
double layer inverting |
|
|
what are the layers for body wall closure? |
1. transverse abdominus and peritoneum- 2.0 vicryl 2. IAO - 2-0 vicryl 3. EAO- 0 vicryl 4. cutaneous trunci- 2-0 vicryl |
|
|
what is the target birth weight for a lamb? |
3-4kg average 2.5-5kg |
|
|
when are lambs weaned off milk? |
when they are 16kg, 7-8wks old |
|
|
what is the minimum age to mate sheep |
7 months, 30-35kg |
|
|
what % of lameness indicates the whole flock should be investigated? |
5% |
|
|
what % of abortions in a flock indicates there may be endemic or epidemic disease and should be investigated? |
2% |
|
|
what BCS should ewes be in at joining? |
3-3.5 |
|
|
describe nutritional requirements for ewes in their last month of pregnancy |
- an ewe carrying a single foetus requires twice as much feed as a non-pregnant ewe - a twin bearing ewe requires 2.5x as much as a non pregnant ewe - a triplet bearing ewe requires 3x as much feed as a non-pregnant ewe |
|
|
what drug is used to reverse xylazine? |
yohimbine (reversine) |
|
|
list 4 conditions seen in goats, not seen in sheep |
1. pseudopregnancy (hydrometra) 2. CAE virus 3. intersexuality associated with polledness 4. witches milk (kids) |
|
|
list differences between goats and sheep |
- sheep have 54 chromosomes, goats have 60 - sheep graze close to ground, goats browse shrubs etc - sheep are less social than goats - sheep can tolerate rain (wool) but goats will seek shelter - wethers/rams charge forward to butt but wethers/bucks rear up and butt - lambs stay with the ewe during the day, whereas does hide their kids - in sheep the tail hangs down and in goats the tail is usually up - sheep have philtrum, goats have a line but is fused - sheep do not have beards - sheep have interdigital glands, goats do not** |
|
|
what are the highest cost diseases in the Aus sheep industry? |
1. internal parasites 2. fly strike 3. lice 4. post weaning mortality |
|
|
animals suffering from virulent foot rot can lose up to 15% body weight, true or false? |
true |
|
|
list reportable diseases and say if they affect only sheep or only goats or both |
- FMD- both - liver fluke- both - Maedi Visna- both - Nairobi sheep dz- both - new world screwworm- both + cattle, dogs, cats, humans etc - old world screw worm - ovine pulmonary adenomatosis - Johnes- both - S strain (also deer) - Rabies- both - Pestes des petits ruminants- both - Rift valley fever- both - Salmonellosis abortus- sheep - Scrapie - both - sheep scab (Psoroptes ovis)- sheep - TSE- both - Tularaemia - sheep - virulent foot rot - Wesselsbron disease- sheep, goats, humans
|
|
|
what are the potential threats to the sheep and goat industry? |
1. exotic and endemic diseases 2. food safety 3. chemical residues in wool, meat 4. welfare 5. high mortality rates |
|
|
list specific diseases of welfare concern in a) sheep b) goats |
a) sheep - sheep scab - foot rot - lameness b) goats - lameness - teat and udder lesions - pruritis and skin lesions |
|
|
name a breed of goat more prone to hypothermia |
angora goats |
|
|
what are the important characteristics of production animal vets? |
- compassion, knowledge, professionalism - understand economic pressures of farmers - realise financial considerations - good communication skills - enthusiastic - well trained in sheep management and production |
|
|
when is lambing in Australia? |
Autumn and winter |
|
|
what are the farmer life stages? |
young and single - inexperienced - has off farm interests - lacks management skills married with children - highly motivated and very hard working - risk takers, innovative middle aged - may be hand over problems - wants to enjoy life a little - good management skills, good to work with semi retired/retired - wants security and comfort - still wants some involvement |
|
|
what is the most profitable type of sheep enterprise? |
dual purpose fine wool merino = meat and wool |
|
|
what is the biggest factor associated with profitability for merino sheep and wool enterprises in Aus? |
stocking rate lamb weaning % also very important |
|
|
what are the key factors affecting profitability in Aus? |
1. stocking rate 2. weight of clean fleece produced per Ha 3. sale price of wool 4. number of surplus sheep sold (determined by weaning percentage*) 5. sale price of surplus sheep 6. time of lambing- match to pasture growth curve 7. pasture production and utilisation 8. feeding 9. genotype- some genotypes of sheep more productive 10. flock structure 11. effective parasite control 12. correct wool (clip preparation) |
|
|
how long should rams be left in with ewes for joining? |
6 weeks |
|
|
what factors should be taken into account when choosing time of joining and lambing? |
1. pasture - pasture growth pattern for district - pasture composition - time of mating/lambing should be matched to pasture growth curve 2. flock - flock structure- number of ewes vs whethers - stocking rate 3. aim of enterprise 4. breeding season of sheep - some breeds i.e. suffolk if put out in Oct won't breed 5. management - time of shearing - don't want to be shearing at same time of lambing - marketing plans - cost of supplementary feed including crop residue - other farm activities |
|
|
what are the presenting problems of infertility in ewes? |
1. low lambing % 2. low lamb marking 3. lactating barren ewes - oestrogenic clovers 4. vulval changes in ewes - oestrogenic clovers - oestrogenic fungal toxins- zearalenone |
|
|
when should ewes be joined? |
at BCS 3-3.5
|
|
|
what can be some presenting problems of ewes in late pregnancy? |
1. low lambing % 2. abortion 3. vaginal discharge 4. deaths of ewes over days/weeks 5. cast, recumbent comatose ewes 6. separated from mob, fall over when driven 7. vaginal prolapse 8. does failing to kid but look pregnant |
|
|
when should abortion be investigated? |
> 5% of flock - occurring over short period of time i.e. 2wks - occur in specific location i.e. specific paddock |
|
|
what is the treatment for pseudopregnancy in does? |
1. prostaglandins - dinaprost 5-10mg/kg IM - if doesn't break water tx again in 12d *make sure confirm not pregnant via US first |
|
|
pregnancy toxaemia is an indicator of... |
poor management |
|
|
what are the predisposing factors for pregnancy toxaemia |
= anything that affects ewes ability or desire to graze - sore feet- always check feet - bad weather - sudden change in diet - stopping supplementary feeding - decline in feed quantity or quality - yarding/trucking/transport - disease i.e. footrot - too fat (ketosis) |
|
|
a farmer calls with a history of neurological signs and death in several of his sheep over a month. You arrive to the farm and find two ewes, separated from the mob, in BCS 1.5-2, blind and recumbent. These ewes are due to lamb in 4 weeks. What is the most likely diagnosis? and the main differential and how would you manage this case? |
pregnancy toxaemia main ddx is hypocalcaemia would euthanase these ewes because too far gone but would evaluate the management and the rest of the flock to prevent the same outcome in the other ewes --> nutritional management very important - ewes should be on high plane of nutrition, provide supplementation |
|
|
how is pregnancy toxaemia diagnosed? |
1. history/clinical signs - thin ewes in last month of pregnancy - neurological signs - stop eating - spread out death within a week - show no fear of man or dog - wool break 2. bloods - hypoglycaemia - ketonaemia: elevated 3-hydroxybutyrate >3000umol/L - Ca levels to differentiate from hypocalcaemia + ketonuria 3. PM - enlarged, pale-yellow, friable fatty liver - often adrenals enlarged - faeces firm and dry - can test aqueous humour for butyrate 3. PM |
|
|
the preferred route of administration for flunixin is IV. true or false? |
false! do not give flunixin IV - can kills sheep! |
|
|
how can early pregnancy toxaemia be treated? |
1. give hay 2. glucose liquid concentrate (Vy-trate), repeat every 4-6h 3. flunixin + Ca + dextrose 4. +/- electrolytes 5. +/- hormonal therpay 6. +/- rumen transfaunation |
|
|
what are the precipitating factors for hypocalcaemia? |
1. sudden deprivation of food 2. inclement weather- sheep don't want to go out and graze 3. stress- management practices i.e. mustering, shearing, crutching
|
|
|
what is the critical level for calcium? |
2mmol/L when drops below this see clinical signs of hypocalcaemia |
|
|
hypocalcaemia is common in sheep shorn in winter. True or false? |
True |
|
|
plants containing _______ can cause hypocalcaemia |
oxalates |
|
|
when are oxalate plants most dangerous? |
after autumn rain - they germinate |
|
|
list differentials for hypocalcaemia |
1. pregnancy toxaemia 2. hypomagnesaemia 3. oxalate poisoning 4.enterotoxaemia 5. superphosphate poisoning 6. mastitis 7. bloat |
|
|
describe how to diagnose and treat hypocalcaemia |
diagnosis: 1. clinical signs and Hx - recent change in management, climate or feeding i.e. sudden deprivation of food, grain/cereal diets or recent stressor i.e. shearing, mustering, drenching etc - mouse or frog position - ataxic, staggery gait - muscle tremors esp facial muscles - sheep going down - tachycardia, tachypnoe - temp normal or decreased - bloat, green contents around nose and mouth - vaginal prolapse - depressed corneal reflex - can be coma and death in 6-12h 2. CBC and biochem - Ca < 2mmol - inorganic phosphorus may be reduced - Mg may be reduced - glucose normal unless concurrent preg fox 3. PM - no gross or histopath changes - unless the hypocalcaemia is due to oxalate poisoning or there is concurrent disease i.e. preg tox--> fatty liver
treatment: 1. Ca borogluconate slow IV - monitor HR - takes 5 mins to respond - or 60-80ml SC over ribs if outbreak* *do not exceed 170ml total 2. management - moved affected mob to new paddock- sometimes prevents further cases - prevent preg toxaemia in surviving ewes- provide feed - warn farmers that pregnant ewes may abort
|
|
|
how can hypoalcaemia be prevented? |
1. avoid predisposing factors i.e. stress, food deprivation in pregnant or lactating animals 2. unimix drench - contains Ca 3. add Ca to rations - 1.5% limestone/Ca Carbonate 4. graze young wheat and oat crops for short time only 5. watch for oxalate containing plants following thunderstorms |
|
|
when do vaginal prolapses most commonly occur? |
< 3 weeks before lambing (last 3 wks of pregnancy) |
|
|
describe normal parturition/lambing |
- ewe separates from the mob, may strain, membranes protrude from vulva - time in stage 2 usually < 30mins for singles, up to an hr for multiples - placenta expelled in 2-3h (stage 3) |
|
|
describe normal parturition/kidding |
- relaxation of ligaments = kidding usually 12-24h later - moves away from other does - kidding takes 1hr max - foetal membranes expelled in 4hrs (stage 3) - lochia lasts about 14d after kidding |
|
|
what are the indications to assist in parturition? |
1. membranes have ruptured but no progress in 30 mins 2. lambing/kidding takes > 90 mins 3. tail, one leg or head delivered |
|
|
when is the best time to determine if a ewe is a single or multiple bearer with US? |
between day 45-90 of gestation (when ewe has not been exposed to a ram for 45d) |
|
|
what drug should be used to induce parturition if a) ewe is < 55 days pregnant? b) ewe is > 55 days pregnant? |
a) prostaglandins b) corticosteroid |
|
|
when is the CL refractory to prostaglandins? |
- days 1-4 after ovulation - days 12-26 after (wks 2-4) - after day 55 (after 8wks) |
|
|
describe management of ewes for gestation, parturition and lactation |
trace element deficiencies 1. iodine drench given in 4th and 5th month of pregnancy 2. copper capsules 3. long acting Se pellet - protects offspring via milk 4. cobalt pellet or vit B12 injection - protection of offspring via milk prevent metabolic diseases: - hypocalcaemia- provide feed, don't deprive, avoid stress factors - preg tox- provide high plane nutrition - hypomagnesaemia vaccinate 1. clostridial vaccine one month prior to parturition for passive immunity for the lamb parasite control - drenches- note WHP, make sure safe to use in pregnant animals crutching - some ewes need to provide access to the udder shearing - ewes shorn within 4 wks of lambing usually seek shelter during lambing and survival of multiple born lambs is increased - shearing winter lambing ewes prior to lambing may result in better lamb growth |
|
|
list 5 diseases of lactating ewes and does |
1. hypoMg 2. hypoCa (more common in gestation) 3. mastitis 4. udder lesions 5. kangaroo gait |
|
|
what is the most common clinical sign of hypomagnasemia in ewes? |
sudden death
neurological signs are rare in sheep (unlike in cattle) |
|
|
compare and contrast pregnancy toxaemia, hypocalcaemia and hypomagnesaemia in regards to signalment, predisposing factors, clinical signs, diagnosis and treatment |
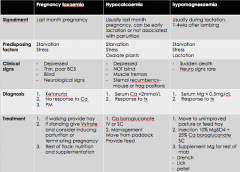
|
|
|
what is the significance of a) clinical mastitis b) subclinical mastitis |
a) clinical - ewe and lamb deaths - tx costs - permanent udder damage resulting in culls b) subclinical - decreased milk yield - reduced lamb growth - lamb deaths |
|
|
what are the causes of mastitis? |
1. acute clinical mastitis - Staph aureus alone or in mixed infection - Mannheima haemolytica 2. gangrenous mastitis - Staph aureus - E.coli 3. chronic mastitis - Staph aureus - Corynebacterium pseudotuberculosis - Arcanobacterium pyogenes 4. subclinical mastitis - Staph aureus - Staph epidermidis - Staph stimulans - Streptococci spp 5. mycoplasmal mastitis -Mycoplasma agalactiae = contagious agalactia - not in Aus 6. viral mastitis - CAE in goats - Orf related mastitis (scabby mouth) - Maedi visna (ovine progressive pneumonia)- not in Aus 7. fungal mastitis - rare |
|
|
what are the predisposing factors for mastitis? |
1. stage of lactation - after parturition and weaning most common times 2. environment - improved pastures increase milk production 3. teat injuries i.e. from lambs teeth facilitate microorganism entry into teat 4. loss of lamb/kid or inability to suckle causes milk to build up 5. increased prevalence with age |
|
|
what are the clinical signs of mastitis? |
- separates from mob - lameness - signs of toxaemia- stops eating, pyrexia (40.5-42oC), abscesses may break out on skin - udder hot painful +/- enlarged - agalactia - appearance of milk variable - with gangrenous mastitis get black dead skin on udder that may slough and also fleece break and udder may get fly strike - death in 1-4d |
|
|
name an organ that should always be inspected when you see fleece break and/or lameness? |
the udder |
|
|
what are some indicators of mastitis in the field? |
1. bleating/starving lamb 2. ewe not letting lamb suckle 3. ewe looks lame 4. recumbent ewe 5. part of udder missing 6. fleece break (severely stressed) |
|
|
describe diagnostic intervention and management and control of ewes with mastitis |
1. post milking mid stream culture - 5ml - submit for C+S 2. milk somatic cell counts nb goats have higher SCC and can have SCC for reasons other than mastitis, whereas in ewes high milk SCC = mastitis
management: - treat with empirical parenteral or intramammary broad spec ABs whilst awaiting results of C+S and give an NSAID - in acute cases response to tx is poor- if flock problem would cull - chronic mastitis - ewes usually have permanent damage to udder- cull
control: - identify and cull infected animals - improve hygiene at milking - give dry ewe therapy i.e. intramammary sodium cloxacillin |
|
|
describe how to do milk culture |
- post milking samples best - swab teat with 70% alcohol and collect approx 5ml of mid stream milk into sterile container - collect a separate sample for each mammary gland - submit for C + S |
|
|
list differentials for teat skin lesions |
1. contagious ecythema (contagious viral pustular dermatitis) 2. capripox infection 3. staph folliculitis/ pustular dermatitis - Staph aureus 4. zinc responsive dermatitis/zinc deficiency 5. neoplasia - papilloma - SCC 6. ringworm 7. abscess 8. chorioptic mange |
|
|
Witch's milk in goat kids should be treated asap to prevent permanent damage. True or false? |
false. Not treated |
|
|
when does a ewe reach maximal productivity? |
3rd lactation declines after 6th lactation |
|
|
when should dairy does be dried off? |
2 months before due to kid |
|
|
what are some unique characteristics of goats milk? |
1. high digestibility 2. alkalinity 3. high buffering capacity 4. certain therapeutic value |
|
|
how can u tell if a ewe has lambed? |
- large udder - blood encrusted wool on back of udder - normal milk, teats clean and soft (cleaned by lamb) - may have wool break (stress) - non lactating ewes have better BCS |
|
|
what are the normal vitals for a lamb? |
Temp: 38.6- 39.4 (>40 = hyperthermia, <37 = hypothermia) HR: 70-90bpm RR: 12-20bpm |
|
|
the most prominent sign of a lamb with pneumonia is it will be coughing. True or false? |
false. lambs with pneumonia don't normally cough |
|
|
list congenital and heritable diseases in lambs |
1. entropion 2. cerebellar atrophy 3. congenital goitre- iodine deficiency 4. congenital Se deficiency 5. congenital Cu deficiency 6. Border disease |
|
|
what are the treatment options for congenital entropion? |
1. manual eversion within 48h of birth 2. surgical staples to evert eyelid 3. injection SC into affected eyelid of sterile saline, sterile air or AB such as benzathine penicillin or oxyte = best option cull sire rams and don't breed from affected offspring |
|
|
what are the clinical signs of congenital Se deficiency? |
sudden death affects cardiac muscle |
|
|
congenital Cu deficiency is treatable. True or false? |
false |
|
|
what are the clinical manifestations of border disease virus when the ewe is infected at certain times during gestation? a) day 14 b) day 16-25 c) day 25-45 d) day 45-50 e) day 50-90 f) after day 90 |
a) day 14- no effect, zygote resistant to infection b) day 16-25- early embryonic death c) day 25-45- abortion due to placental damage d) day 45-50- still birth e) day 50-90 - teratogenic effects- hairy shaker lamb born and dies in a few days f) after day 90- no clinical signs |
|
|
clinical evidence of border disease only occurs if ewe is infected between day __-__ of ingestion |
16-90 |
|
|
what 2 diseases should be ruled out to make diagnosis of border disease? |
1) copper deficiency 2) meningitis
PM |
|
|
list the causes of perinatal death in order of importance |
1. birth stress- 60% - effects on thermogenesis, suckling and locomotor function 2. starvation- mismothering exposure complex - 25% - i.e. aberrant maternal behaviour, primary hypothermia, management induced mismothering and inadequate milk supply 3. disease - 15% - malformations, infections, TE deficiencies and predation |
|
|
what are the predisposing factors to starvation-mismothering complex? |
1. poor mothering ability - maiden ewes 2. ewe cannot feed lamb - i.e. exhaustion after parturition 3. lamb is weak or does not suckle/can't suckle - i.e. lamb has brain damage = no suckle reflex |
|
|
what are the predisposing factors to exposure/hypothermia of neonatal lambs? |
1. birth injury i.e. dystocia 2. low birth weight i.e. twins, triplets 3. lambs received no colostrum or inadequate milk 4. cold, wet weather 5. excessive disturbance of lambing flock 6. ewes long fleece prevents feeding |
|
|
list post natal conditions that occur within 48h of birth |
1. starvation - mismothering 2. exposure/hypothermia 3. predation 4. neonatal infection 5. watery mouth |
|
|
when are the 2 main times of hypothermia risk in lambs? |
1) birth - 5hrs due to excessive heat loss in wet newborn lamb exposed to cold wet weather hypoglycaemia uncommon 2) 10hrs to 3 days old due to depressed heat production due to starvation and exhaustion of energy reserves hypoglycaemia common |
|
|
how should you manage a hypothermic lamb within 5hrs of birth? |
1. take rectal temp - n = 39oC - < 37oC = severe hypothermia 2. dry lamb with towel 3. warm lamb until rectal temp reaches 38oC 4. feed colostrum via stomach tube or milk if too old for colostrum |
|
|
what is the treatment for polyarthritis in neonatal lambs? |
5 daily injections of penicillin |
|
|
what is the treatment for umbilical infections in neonatal lambs? |
5 daily injections of penicillin |
|
|
list 3 ways to prevent bacterial infections in neonates |
1. good hygiene - during lambing - dip umbilicus with iodine 2. colostrum 3. vaccination of ewes
|
|
|
what are conditions that affect 2-7 day old lambs? |
1. desertion by ewe- orphan lamb 2. starvation 3. enteritis |
|
|
list conditions that affect lambs 1-4wks old (delayed post natal conditions) |
1. Se deficiency/ white muscle dz 2. Cu deficiency/swayback |
|
|
what time of the year do most cases of Se deficiency occur? |
winter and spring on clover dominant pasture |
|
|
selenium deficiency is incurable. True or false? |
false, it is readily treatable |
|
|
what are the differentials for white muscle disease in suckers? |
1. infectious arthritis 2. spinal abscess 3. Cu deficiency 4. enterotoxaemia (sudden death) 5. vitamin E responsive myopathy - looks the same clinically but is usually in weaners, not lambs |
|
|
which sheep breed is highly susceptible to Cu toxicity? |
texels so ALWAYS confirm Cu deficiency before tx |
|
|
what is the cause and what are the clinical signs of delayed sway back? |
caused by Cu deficiency - lambs bc ewes on Cu deficient feed i.e. fresh green pasture
clinical signs: - BAR - willing to suck, normal temp - uncoordinated movement and knuckling - swaying gait - goes into dog sitting when driven - may have pale mm--> anaemia |
|
|
describe diagnosis and treatment of Cu deficiency in lambs 2-12wks old |
diagnosis: 1. history and CS - swayback - dog sits when driven - BAR etc 2. bloods i. CBC: macrocytic, normochromic anaemia iii. superoxide dismutase assay 3. PM - if flock problem sample 5-10 animals - no gross changes - histopath of kidney, liver,brain and spinal cord |
|
|
How is Cu deficiency treated? |
cannot be treated if diagnose the aim is to prevent for future by oral or parenteral Cu * oral Cu oxide particles early in pregnancy is the recommended way |
|
|
how can you prevent Cu deficiency? |
1. oral - PO copper oxide particles tx of choice - mineral blocks, licks - drenches 8 and 4 wks before lambing 2. injection - less safe, can cause toxicity and death 3. top dress pasture |
|
|
what is the most common reason to foster a lamb? |
dam has died or abandon lamb |
|
|
what are the risks of lambs not getting adequate high levels of colostrum in first 24h of life? |
- unthrifty - infection - no passive immunity - hypothermia - high mortality |
|
|
how much colostrum should be fed to orphan lambs? |
50ml/kg per feed (to avoid distending stomach) |
|
|
contrast ewes milk to cows and goats milk |
ewes milk is higher in fat, protein and caloric density |
|
|
at what age range are lambs usually marked? |
1-6wks old |
|
|
what is the best milk substitute for orphan lambs? |
full cream powdered milk alone mix 200g powder with warm water to make 1L milk gives a liquid of 20% DM |
|
|
what are the necessary components of ewe milk replacer? |
fat: 20-30% of DM protein: 25-30% lactose: < 160g/d fibre: 0-1% vitamins and mineral |
|
|
list 2 sheep breeds that don't require shearing |
- damara - wiltshire |
|
|
how can selenium deficiency be prevented in orphan lambs? |
1mg Se added to milk every 4-6wks |
|
|
what is the one marking procedure that is compulsory in WA? |
ear marking |
|
|
list procedures that may be carried out at marking |
1. ear marking (compulsory) 2. ear tagging 3. tail docking 4. castration 5. vaccination - 6 in 1 (clostridial diseases, CLA) - Johnes - scabby mouth 6. mulesing 7. shearing 8. hoof trimming |
|
|
what diseases can be prevented by marking procedures on lambs? |
1. breech strike 2. pizzle strike 3. body strike 4. poll strike 5. ectoparasites 6. foot rot, foot abscess 7. fighting, mismating |
|
|
list alternatives to: a) surgical tail docking b) mulesing c) surgical castration |
a) surgical tail docking 1. rubber rings 2. use breeds that don't need docking - Awassi, Dorper, Damara 3. breed for short tails - but tends to be associated with other defects i.e. spina bifid a
b) mulesing 1. chemical mulesing 2. clips 3. breed plain bodied sheep 4. use less wrinkle skinned breed - British, European, Middle eastern or African 5. Crutch more often 6. drench for internal parasites 7. select for resistance to internal parasites 8. jet with long acting chemicals
c) surgical castration 1. chemical castration - injection of sclerosing agent i.e. calcium chloride, formaldehyde 2. rubber rings 3. leave entire |
|
|
list potential problems post marking |
1. death 2. pain and distress 3. tetanus 4. spinal abscess 5. vaccine reaction 6. rectal prolapse 7. cutaneous miasis 8. tail lesions 9. perineal SCC |
|
|
what are the clinical signs of tetanus? |
- saw horse stance - muscle tremor - trismus (lock jaw) - 3rd eyelid prolapse - stiff gait - exaggerated response to stimuli - tetanic convulsions - splaying of digits - death in 3-4 days |
|
|
there is an outbreak of tetanus in a mob of lambs following marking. You euthanise 3 lambs that are severely affected. What can you do for the remaining lambs if they have been affected < 10 days ago |
consider giving 100 units of TAT and give toxoid and repeat toxoid injection in 6wks |
|
|
how can tetanus be prevented? |
- good hygiene at making - vaccinate ewes with 6 in1 2-4wks before lambing annually - vaccinate lambs at marking, weaning and give an annual booster - take care when trimming feet- don't cut so bleeds and then walking around |
|
|
when investigating weaner ill thrift, how many sheep should be weighed? |
10% of the mob or 50 sheep if 10% of the mob is >50 5-10 sheep = representative sample |
|
|
what is weaner ill thrift and what is the most common cause? |
= failure of a weaner to grow well at a time when all other classes of sheep appear to be in good health and body condition |
|
|
mineral deficiency that causes scaly ears? |
Cobalt deficiency (vit B12) |
|
|
What causes steel wool? |
Cu deficiency |
|
|
what is the most common nematode to cause diarrhoea in sheep? |
Trichostrongylus - black scour worm |
|
|
when animals are investigated for weaner ill thrift a) how many animals should be sampled? b) what samples should be taken?
|
a) 3-10 samples per mob from live animals b) - blood in EDTA and lithium heparin - serum in plain vacutainer - 10 faecal samples (1/3 yellow container) + 3 affected weaners for necropsy |
|
|
what parasites can cause diarrhoea/ill thrift in weaners? |
- nematodes - Coccidia - Cryptosporidium - Giardia |
|
|
what is the definition of a clean paddock? |
spelled for 6 months in winter or 3 months in summer (not achievable for a lot of farmers) |
|
|
which trace elements are most commonly deficient in weaners? |
Cobalt and selenium |
|
|
what are the causes of weaner ill thrift syndrome? |
multifactorial some major causes include: 1. internal parasitism 2. TE deficiency 3. nutritional 4. chronic infections
|
|
|
what are the clinical signs of copper deficiency in weaners? |
- pale mm- anaemia - ataxia, swayback, dog sitting - knuckling HL - depigmentation of coloured wool - steely wool |
|
|
describe diagnostic work up for weaner ill thrift syndrome |
1. rule out parasitism - faecal samples 2. rule out TE deficiency - measure Co or MMA (preferred) - measure glutathione peroxidase (or Se) +/- CK - measure Cu? |
|
|
what is the bench mark for weaner deaths? |
4% |
|
|
describe how to manage weaners |
- length of joining should be only 5-6wks - should be put onto clean paddock (spelled for 6m in winter or 3m in summer) - short (4-8cm) legume based (clovers, medics) crops or standing fodder crops are best. Weaners are not good on long grasses - perennial ryegrass > annual ryegrass - require high protein diet fro growth i.e. a 25kg weaner needs 15% protein in digestible foodstuffs containing adequate energy - mark 6-7wks after starting lambing - teach grain feeding: 2 feeds given over one week to the ewes while lambs are at foot a couple weeks before weaning. Rumen is fully functional at 8wks - wean at 12-13wks - monitor BCS and weigh 50 sheep monthly - vaccination - first at marking and 2nd (booster) at weaning (and then annual) - drench +/- DRT at weaning onto clean pasture - pellets given to weaners to prevent Cu, Co, Se deficiency - calculate weaner death rates from last 5y, get a benchmark
|
|
|
describe best practice management to avoid weaner deaths |
1. draft off tail (lightest) sheep at weaning and feed supplements - weigh every 4 months - feed 2.5kg/head/month of oats + lupins if no green feed - aim for 0.25-.05kg weight gain/month 2. do not shear weaners in Autumn - 4 x increased risk of death - most farmers sheet for first time when still lambs or weaners - results in increased growth rate bc tend to eat more bc cold |
|
|
what are the reasons farmers shear lambs/weaners? |
1. makes management easier 2. increases growth weights bc are cold so eat more 3. stops grass seeds 4. makes lice control easier 5. makes fly control easier 6. improved wool return 7. lambs do better if shorten |
|
|
when can weaner ewes be bred? |
british breeds at 7-9months if they weigh > 45kg merinos at 8-9 months if they weigh > 37kg |
|
|
when do most rams reach puberty? |
27kg |
|
|
list economic impact of posthitis in wethers/rams |
1. death via uraemia, infection 2. welfare concerns 3. fly strike 4. decreased wool production (<0.5kg/sheep) 5. decreased growth rate 6. decreased sale value of affected sheep 7. ram wastage |
|
|
biggest risk factor for posthitis? |
high protein diet i.e. lupin grain, clover pasture |
|
|
antibiotics are the mainstay for treating posthitis. True or false? |
false. They are NOT recommended |
|
|
cereal grains are low in __ and high in __ and __ |
low in Ca high in P and Mg |
|
|
what are the causes of the following uroliths: a) phosphate b) silica c) Ca carbonate d) organic complexes |
a) phosphate - feeding concentrarte diets --> supersatuted urine --> precipitation of Mg and Ca. alkaline urine favours this - cereal grain diets - low in Ca, high in P - cereal diets also decrease salivation so that there is less excretion of P via saliva and more via urine - high Mg in cereal diets may also cause in grain fed lambs
b) silica - plants such as cereals esp oat stubble, hay and grain as well as native grasses - urine pH has no effect
c) Ca carbonate - alkaline urine causes to precipitate - plants such as mulga, portulaca, parakelia etc (high in Ca and oxalates)
d) organic complexes - phyto-oestrogen induced calculi in sheep on high oestrogen sub clovers - oxalate calculi - cysteine - xanthine |
|
|
how is a diagnosis of bladder rupture/uroperitoneum confirmed? |
abdominocentesis and bloods creatinine in abdominal fluid: creatinine in blood > 3:1 |
|
|
Brucella ovis affects both sheep, goats and humans. True or false? |
False. Brucella ovis only affects sheep so does not affect humans or goats |
|
|
what is the usual presenting complaint associated with Brucella ovis? |
abortions in ewes or decreased lambing % |
|
|
what is the primary test for diagnosing Brucella ovis? |
CFT (complement fixation test) - serological titre - will be positive 10-20d after infection - gel diffusion test and ELISA can be used to supplement this test |
|
|
describe the best method for eradicating B.ovis on a property? |
1. examine all rams > 6 months - palpate scrotum and collect blood for CFT 2. cull +ve rams 3. re-palpate and bleed -ve rams at 2-3wks until completely clear 4. re-test again in 2m and if clear can declare negative 5. cull suspicious reactors (isolate and re-test) 6. repeat CFT annually and PE rams |
|
|
what diagnostics are used for investigating B.ovis? |
combination of diagnostics should be used 1. history 2. palpate testes 3. bloods - CFT (can get false -ves) +/- ELISA, +/- gel diffusion test 4. semen sample - culture and cytology - +ve culture confirms but -ve culture does not rule out 5. histopath of testes if dead ram/sacrificial euth 6. histopath and samples from foetus and placenta |
|
|
list ddx for B.ovis |
1. Actinobacillus seminis 2. Histophilus ovis 3. traumatic granuloma of tail of epididymis 4. Brucella miletensis - rare cause of orchitis and exotic in Aus |
|
|
pyrexia is a major clinical signs of rams that have oB.ovis. True or false? |
False. Pyrexia does not occur with B.ovis if rams have scrotal lesions and pyrexia think Actinobacillus seminis, especially in virgin rams |
|
|
what is the etiological agent for swelled head in rams? |
Clostridium novyi |
|
|
when should lameness in a flock be investigated? |
> 5% flock lame (bench mark is < 2-3%) |
|
|
OID (ovine interdigital dermatitis) occurs sporadically in individual animals, true or false? |
false up to 90% of flock can be affected |
|
|
how is OID differentiated from foot rot? |
positive culture of Dichelobacter nodosus = foot rot |
|
|
what are the differentials for OID? |
1. footrot 2. foot abscess 3. FMD 4. blue tongue |
|
|
what are the common sources of foot rot infection and how is it transmitted? |
stray sheep and introduced infected sheep more common source source of infection from discharge from infected feet |
|
|
virulent foot rot only affects sheep. True or false? |
false, affects sheep and goats |
|
|
describe survival of Dichelobacter nodosus |
to survive needs moisture and ambient temp > 10oC (common in spring) can only survive 4-7d away from foot doesn't live long in environment (7 day max) |
|
|
describe the economic importance of virulent foot rot |
- about $3000 plus one week of farmers time and one week of livestock inspectors time - $2.95/head/yr loss of production in a flock of 3000 sheep - eradication cost $7.41/ head - 10% reduction in fleece weight - increase in sheep with tender wool - loss of body weight- sore feet = reluctant to graze - risk of fly strike - death - loss in value of sale- no one wants to buy sheep with foot rot - restrictions in marketing sheep from affected properties - severe welfare implications- extremely painful |
|
|
in regards to foot rot what are the a) early clinical signs b) clinical signs if severely affected c) systemic signs |
a) early: - swelling and redness and moistness in interdigital skin - hair loss between claws -> 1 foot affected, often all 4 - lameness severe when extensive under running and separation of horn tissue from wall and sole of hoof b) severely affected - holding leg up - grazing on knees - shifting lameness - recumbent - lamb with foot rot look like coal walkers c) systemic signs - anorexia and inappetance - loss of BCS - fever - preg tox - wool break - secondary bacterial infection up legs - cutaneous miasis |
|
|
what are the aetiological agents responsible for: a) virulent footrot b) OID c) foot abscess |
a) Dichelobacter nodosus (S strain) b) Fusobacterium necrophorum and Arcanobacterium pyogenes c) Fusobacterium necrophorum and Arcanobacterium pyogenes |
|
|
foot abscess is common in ______________ and uncommon in_______________ |
common in lambing ewes and rams uncommon in lambs |
|
|
describe treatment of foot abscess |
treatment if structures are not permanently damaged: 1. put onto dry environment - i.e. shed 2. walk through 10% ZnSO4 foot bath 3. individual tx - remove scabs and exidate - if infection is deeper or pus is present- express pus and irrigate with chlorex then poultice and bandage. change bandage daily 4. systemic ABs - long acting oxtet - may be useful in early stages
5. if structures are damaged amputate or euth |
|
|
how is toe abscess treated? |
1. pare the horn overlying necrotic laminae to release pus 2. 10% ZnSO4 foot bath |
|
|
what is the incubation period of tetanus? |
3-10 days |
|
|
how does FMD manifest in goats? |
subclinical infection most common if clinical- lameness is the most common clinical sign |
|
|
___________deficiency is associated with fertilised pastures, acid soils and high rainfall |
selenium |
|
|
what are the clinical signs of myopathy? |
- abnormal posture, gait, hunched, stiff, weak - staggery - paddle limbs when in lateral recumbency - froth at mouth and nostrils - red urine (myoglobinuria) |
|
|
describe diagnostic work up of myopathy |
1. history - housing i.e. vit E deficiency common in housed animals - rainfall i.e. Se deficiency associated with high rainfall - supplementation? ask to see product - any deaths (cardiomyopathy- Se deficiency) - class of animals affected at different times of yr- weaners vs lambs - stress? i..e mustering, yarding, weaning 2. clinical signs - hunched stance, staggery gait, stiff, weak - paddle when recumbent - froth from nose and mouth - red urine 3. bloods (10 affected sheep) - elevated CK and AST - alpha tocopherol- vit E deficiency - glutathione peroxidase- Se deficiency 4. necropsy 3 recently dead animals - bilaterally symmetrical pale muscle, esp HL, also cardiac m - liver, kidneys, rumen contents - feed samples if suspect monensin toxicity 5. response to treatment - confirms diagnosis |
|
|
name 2 ways in which lambs can get polyarthritis |
1. bacteria in umbilicus soon after birth 2. bacteria entering a wound i.e. at marking or mulesing and then get bacteraemia to joints |
|
|
the most common cause of arthritis in sheep in Aus is? |
Erysipelothrix rhusiopathae |
|
|
why is scrapie seen in adult sheep and not in younger sheep? |
long incubation period |
|
|
sheep being fed silage that are sick and have nervous signs. What is the first thing you should think of? |
listeriosis |
|
|
what causes a rocking horse gait? |
rye grass toxicity |
|
|
etiological agent responsible for bottle jaw? |
Haemonchus |
|
|
what is the most common cause of opisthotonus in sheep? |
PEM (polioencephalomalacia) |
|
|
what is the first thing you should do if suspect ARGT? |
notifiable disease = notify ag dept
also warn farmer ewes may abort |
|
|
describe pathogenesis of ARGT |
occurs in Nov/Dec or from ryegrass hay any time of the yr annual ryegrass (Lolium rigidum) becomes infected with a bacterium (Rathayibacter toxic us) which is transported to the plant by a nematode (Anguina funesta) and the bacterium produces corynetoxin (slimy seed heads) responsible for clinical signs |
|
|
what are the clinical signs of ARGT? |
- affected sheep may appear normal until driven - rocking horse gait - collapse, convulsions (precipitated by exercise and hot weather) - death from respiratory failure - pregnant ewes may abort |
|
|
what is the best option for eradicating ARGT? |
twist fungus (Dilophosphora alopecuri) |
|
|
list differentials for sudden death in sheep |
- anthrax - black disease (infectious necrotic hepatitis) - black leg - botulism - enterotoxaemia - colibacilosis (lambs) - listeriosis - malignant oedema - lamb dysentery - tetanus - salmonellosis - peracute mastitis - pneumonia
- Rift Valley fever virus - bluetongue virus
- coccidiosis - liver fluke - haemonchus
- hypocalcaemia - hypomagnesaemia - lactic acidosis - PEM - red gut (intestinal volvulus) - Se deficiency- cardiac form in lambs
- bloat - choke - casting |
|
|
what causes black disease? |
Fasciola hepatica + Clostridium novyi |
|
|
what are the risk factors for botulism in sheep in Aus? |
- depraved appetite - low nutritive value of pasture - unimproved pasture - drinking water contaminated with decaying carcasses - access to decaying carcasses |
|
|
describe how to prevent botulism |
1. prevent access to carcasses, if an outbreak occurs, move to paddock w.o carcasses 2. vaccinate with specific vaccine- type C/D Cl. botulimum toxoid 3. make sure sheep on good feed to prevent depraved appetite 4. remove carcasses from dams |
|
|
usually the poor doers of the mob are the ones to get enterotoxaemia. True or false? |
false! usually the best in the mob get source: contaminated feed |
|
|
if unable to demonstrate epsilon toxin from SI contents, enterotoxaemia can be ruled out. True or false? |
false |
|
|
what are the lab findings associated with enterotoxaemia? |
- haemoconcentration - glycosuria - hyperglycaemia - elevated pyruvate, lactate and alpha ketoglutarate |
|
|
what are the causes of wool break? |
1. nutritional stress/poor diet - causes thinning of fibres 2. deprived of water/hot water- sheep won't drink 3. break of season 4. diseases that cause inappetance - footrot - mastitis - pregnancy toxaemia - fly strike etc |
|
|
what micro-organism is usually cultured from sheep with fleece rot? |
Pseudomonas aeruginosa |
|
|
treatment of fleece rot? |
cull affected sheep |
|
|
what is the major predisposing factor to body strike in WA? |
Dermatophilus |
|
|
what is the economic importance of Dermatophilus? |
1. reduction in value of fleece and pelt - scabs difficult to remove during processing and don't take up dye - price penalty 2. deaths in young lambs and weaners 3. interference with shearing due to active lesions with scabs at skin surface - shearers can refuse to shear 4. production losses - affected sheep are lighter and grow less wool 5. costs associated with culling - discounts at sale yards and some sheep are not treatable 6. treatment costs and cost associated with jetting for flystike |
|
|
what are the conditions necessary for outbreaks of dermatophilus? |
1. source of infection - infected sheep with ear, nose or fleece lesions - 1 out of 50 infected sheep is enough to spread 2. moisture/wetting event - rainfall, jetting, backlining, dipping - bleeding i.e. ears after ear tagging 3. a way to transfer zoospores to other sheep- close contact - i.e. yarding, trucking, herding etc 4. susceptible sheep - sheep not previously infected and have susceptible skin i.e. skin damage from shearing or ear tagging or prolonged wetting of skin
|
|
|
when are the most common times that Dermatophilus is spread? |
- jetting in long wool - yarding of wet sheep - dipping |
|
|
Dermatophilus is highly pruritic. True or false? |
false usually no pruritus |
|
|
describe treatment and prevention of dermatophilus |
treatment: - most cases recover spontaneously - only treat the sheep which cannot be shorn/ poorly shorn: 1. LA oxytetracycline IM 20mg/kg (WHP 42d) 2. shear 6-8wks later to lift scabies
prevention 1. trace transmission event measure position of top of scab in wool staple - how much wool di have when became infected wool grows 1cm/month 2. avoid close contact wetting events - minimise contact < 30 mins (zoospores come out in 30-45mins) 3. reduce prevalance - cull - treat sheep with active lesions that cannot be shorn 4. avoid routine dipping of weaner sheep in flocks where dermatophilus is a problem - use pour ons - avoid sheep to sheep contact after dipping |
|
|
growth rate of wool? |
about 1cm/month important because use wool break when trying to determine time occurred |
|
|
what is the incubation period of scabby mouth virus? |
1-1.5 days |
|
|
how long does recovery from scabby mouth take and what should you advise farmer to do in this time? |
takes 3-4 wks would be ideal to separate affected and non-affected sheep but in outbreak situation this is not feasible so keep sheep in paddock they are in until scabs drop off |
|
|
how can scabby mouth be prevented? |
1. vaccination = mainstay of prevention vaccinate lambs between 3wks -6 months before leaving farm (live export) old or at marking (6-7wks) - do not vaccinate within 5 wks of shearing - do not vaccinate ewes within 6 wks of lambing- lamb can get affected when suckles |
|
|
how can you confirm scabigard vaccination has worked? |
2 wks after vaccination take 20 lambs and look for a 'take' = small line of pustules where the scrape was applied (live virus vaccine) |
|
|
when should sheep be vaccinated for scabby mouth? |
- annually - vaccinate lambs at marking or if destined for live export 3wks to 6 months after - if lambs going to feedlot should be vaccinated soon after entering - ewes should be vaccinated 6-8wks before lambing starts - do not vaccinate sheep within 5wks of shearing |
|
|
how long does it take to have immunity after scabigard vaccination? |
2 wks will see a 'take' |
|
|
what is the main manifestation of FMD in sheep? |
sudden onset of lameness |
|
|
what is the main clinical sign of Scrapie (TSE) ? |
Pruritis |
|
|
list 2 important ectoparasites for sheep in Australia |
1. Lucilia cuprina (blow fly) 2. Bovicola ovis |
|
|
Lucila cuprina breeds in carcasses and manure. True or false? |
false, Only breeds in moist areas of live sheep |
|
|
how long does it take for Lucilia maggots to complete lifecycle? |
72h |
|
|
what are the clinical signs of cutaneous miasis? |
- abnormal behaviour: wiggle tail, lower head, attempts to bite at area - pyrexia, tachycardia, tachypnoea - toxaemia (death) - wet areas where struck, tender wool, wool break - foul odour - visualise maggots, flies |
|
|
list 2 parasiticides that are recommended for fly control and 2 parasiticides that are not recommended for fly control |
recommended: 1. spinosad 2. cyromazine (IGR) NOT recommended: 1. organophosphates i.e. diazinon 2. synthetic pyrethroids i.e. deltamethrin (Clout) |
|
|
what drugs can be used to treat nasal bot |
- closantel - moxidectin - ivermectin - nitroxynil - rafoxanide
|
|
|
how long can Bovicola ovis survive off the sheep? |
4 wks at 25oC |
|
|
list differentials for lice infestation |
1. itch mite 2. grass seeds 3. sheep scab (exotic to Aus) 4. scrapie (exotic) 5. dermatophilus 6. fleece rot 7. fly strike 8. allergic dermatitis |
|
|
why is it important to know when lambing is due if treating ewes for lice? |
because can't treat lambs < 6 wks and so if treat ewe with lamb at foot then the lice will jump onto lamb |
|
|
how do you treat lice? |
short wool (< 6 months since shorn) 1. IGR i.e. cryomazine long wool (> 6 months since shorn) 1. shear (will lose money) 2. spinosad and then use product to eradicate lice at next shear 3. if whole flock affected use spinosad |
|
|
name 5 mites that can affect sheep and goats |
1. Psorobia ovis - itch mite (sheep only) 2. Chorioptes bovis - scrotal mange (rams and bucks mainly) 3. Psoroptes ovis- sheep scab (exotic) 4. Sarcoptes 5. Demodex |
|
|
list treatment options for itch mite |
- oral ivermectin or moxidectin - amitraz - fipronil - cull (slow spread) |
|
|
what is the preferred test for diagnosing cobalt deficiency? |
MMA (methylmalonic acid) levels in blood |
|
|
when should dairy goats be disbudded? |
< 10 days old |
|
|
what is the most common cause of deaths during winter shearing? |
hypocalcaemia |
|
|
list conditions associated with shearing |
1. hypocalcaemia (fasting) 2. hypomagnesaemia (fasting) 3. preg tox (fasting) 4. poisoning - plants, chemicals 5. cold stress/hypothermia 6. heat stress, sunburn 7. shearing cuts and wounds 8. CLA 9. clostridial diseases 10. fly stike 11. dermatophilosis 12. scabby mouth 13. PEM |
|
|
which sheep are the most susceptible to hypothermia? |
newly shorn sheep < 1 month off shears |
|
|
spread of Corynebacterium pseudo tuberculosis is mostly associated with? |
shearing
probably gains entry soon after shearing via abrasions or can penetrate intact skin of recently shorn sheep |
|
|
what is the most important method of spread of cheesy gland? |
infection sheep with lung lesions coughing bacteria into the environment or onto skin of recently shorn sheep |
|
|
what is meant buy sound wool? |
= when put pressure on it it doesnt break sound = > 30 N/ktex |
|
|
what wool characteristic has the greatest influence on wool ? |
fibre diameter |
|
|
what age group are affected by E.coli? |
lambs and kids < 1 wk olds |
|
|
aetiological agent of lamb dysentery? |
Clostridium perfringens type B
affects lambs < 3 wks old |
|
|
what age group are most commonly affected by coccidiosis? |
4-6 wks |
|
|
what samples should be taken for sheep with diarrhoea? |
1. faeces - 20g/sheep or 10-15 pellets - faecal egg counts - larval culture and identification - examine coccidia and Cryptosporidia - bacterial culture if indicated 2. blood in EDTA - for Hb and PCV - anaemia 3. +/- DRT 4. +/- CBC and biochem 5. +/- necropsy - total worm count - microbiology - histopath |
|
|
describe how to do a drench resistance test? |
the test of choice is faecal egg count reduction test (FECRT) test undrenched lambs about 3-6 months old around weaning time, if they have been recently drenched wait 6-8wks make sure do faecal egg count first - need minimum of 250-300 eggs/g faeces for the test to be viable |
|
|
when should lambs be drenched for the first time? |
at weaning ( ~ 3 months) |
|
|
which drugs does the new DRT kit test? |
- abamectin - moxidectin - levamisole and benzamidazole combination - BZ, levamisole and abamectin combination |
|
|
what is a quarantine drench? |
- when bring new sheep from outside farm should do a quarantine drench - drench new sheep on introduction to farm to exclude all worms - drench with ideally at least 3 groups of anthelmintics - and then put onto wormiest pasture to dilute out the worms that aren't killed by the drench so that don't select for resistant population |
|
|
in Australia Salmonellosis in sheep is mostly associated with |
transportation and feedlots |
|
|
what are the clinical signs of Salmonellosis |
- acute enteritis - many sheep affected - can have outbreaks - pyrexia > 40oC, tachycardia, tachypnoea - green faeces, may contain blood and fibrin - abortion - death in 2-5 days |
|
|
how can Salmonella infection be confirmed ? |
culture faeces |
|
|
etiological agent of weaner colitis? |
Campylobacter |
|
|
the main presenting problem of weaner colitis? |
'failure of drench' |
|
|
list nematodes that cause diarrhoea in sheep |
- Trichostrongylus - Ostertagia - Oesophagostomum - Chabertia - Nematodirus - Trichuris |
|
|
what is the signalment and the clinical signs of coccidiosis? |
- lambs/kids 4-6wks old that have been housed or stressed - especially goat kids because like to sleep in food bin and defecate in - diarrhoea or dysentery - abdominal pain - poor growth rate - anaemia - death |
|
|
how should coccidiosis in lambs/kids be treated? |
toltrazuril 20mg/kg (50mg/ml) 5% suspension- pig product *Nb this is off label use |
|
|
name a product registered for controlling coccidiosis in a) goats b) sheep |
a) goats- monensin but not if producing milk for human consumption b) sheep- lasalocid sodium |
|
|
manifestation of salt poisoning in sheep? |
diarrhoea |
|
|
list 3 causes of bloat in sheep |
1. hypocalcaemia 2. congenital progressive ovine muscular dystrophy (rare) 3. lactic acidosis 4. succulent legume pasture |
|
|
causes of vomiting in sheep |
1. false hellebores 2. lactic acidosis 3. linseed meal 4. nitrate- nitrite poisoning 5. garden plants i.e. azalea 6. rift valley fever |
|
|
discuss bloat in goats |
in goats bloat is a medical emergency** causes: 1. goats grazing succulent legumes i.e. lucerne, clover, lush pasture 2. hypocalcaemia - mild bloat 3. lactic acidosis- frothy bloat 4. secondary to oesophageal choke = gas bloat |

