![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
99 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is bone tissue composed of? |
Bone cells and extra cellular matrix (osteogenic, osteocytes, osteoblasts, osteoclasts) |
|
|
|
Osteogenic cells |
Stem cells that give rise to other bone cells |
|
|
|
Osteocytes |
Former osteoblasts that become trapped in matrix they deposited |
|
|
|
Lacunae |
Tiny cavities where osteocytes live |
|
|
|
Canaliculi |
Narrow channels that connect the lacunae |
|
|
|
Osteoblasts |
Build bone tissue; synthesize soft organic matter of bone matrix; hardens by mineral deposit |
B for build |
|
|
Osteoclasts |
Bone matrix dissolving cells found on bone surface; release minerals (calcium) into the bloodstream |
C for chew |
|
|
What is the extracellular bone matrix composed of? |
Organic & inorganic matter that surrounds the bone cells |
|
|
|
Dry weight of bone? |
1/3 organic & 2/3 inorganic |
|
|
|
Organic matter |
Synthesized by the osteoblasts; includes collagen fibers and other protein based complexes; stimulates the incorporation of calcium into bone matrix |
|
|
|
Inorganic matter |
85% hydroxyapatite (calcium-phosphate salt); 10% calcium carbonate; 5% random ions |
|
|
|
What is the difference between spongy and compact bone? |
The extra cellular matrix is arranged differently; their names speak for themselves |
|
|
|
Compact bone |
Arranged in structures called osteons |
|
|
|
Osteons |
Contain: central (haversian) canal & concentric rings of calcified matrix called lamellae |
|
|
|
Central (haversian) canal |
Blood vessels and nerves run through; connected together by perforating (volkmann) cells |
|
|
|
Spongy bone |
Arranged in structures called trabeculae; matrix is not concentric circles but a lattice-like network of spikes |
|
|
|
Red bone marrow |
Fills the space in spongy bone; produces the blood cells (hematopoiesis) |
|
|
|
Yellow bone marrow |
Fills the medullary cavity; lipid storage |
|
|
|
What are the main functions of the skeletal system? |
Support, protection, movement, mineral storage, hematopoiesis, triglyceride storage |
|
|
|
What is the skeletal system composed of? |
Bones, cartilage, joints, ligaments |
|
|
|
Ossification or osteogenesis definition? |
Formation of bone via 2 methods: intramembranous ossification & endochondral ossification |
|
|
|
Intramembranous ossification |
Produces the flat bones of the skull & part of the clavicle; compact & spongy bone develop directly from sheets of fibrous connective tissue; no cartilage is needed for this process |
|
|
|
Endochondral ossification |
Involves a cartilage bone template that is converted to bone tissue; most bones develop this way; starts around 6th week of fetal development; an epiphyseal plate is formed |
|
|
|
Epiphyseal plate |
Found in epiphyseal end of long bones; remains “open” during bone growth; allows for longitudinal growth of bone; similar to endochondral ossification |
|
|
|
How does bone grow vertically? |
As older cartilage cells are pushed further from the reserve zone, the cartilage is eventually converted to bone tissue, which then allows bone to grow longitudinally |
|
|
|
At what point in life do the epiphyseal plates “close”, converting cartilage to bone tissue? |
Late adolescence |
|
|
|
Wolff’s law of bone |
Bone will remodel the density of the matrix according to the external stresses placed upon it; occurs primarily within spongy bone; less force/stress= decrease in matrix density; & more force/stress= increase in matrix density |
|
|
|
Which 2 hormones have a direct influence on the density of bone? |
Parathyroid hormone (PTH) & Calcitonin - both hormones maintain blood calcium levels |
|
|
|
PTH |
Secreted by parathyroid gland; increases blood calcium levels; stimulates increase of activity of osteoclasts and decrease activity of osteoblasts; activates increase in production of vitamin D, absorption of calcium within intestinal tract, & decreases loss of calcium through kidneys |
|
|
|
Calcitonin |
Secreted by thyroid hormone; decreases blood calcium levels; stimulates increased activity of osteoblasts and decreases activity of osteoclasts; also deactivates absorption of calcium in intestinal tract & increases secretion of calcium in kidneys |
|
|
|
Bone mineral density (BMD) |
Vital to maintain structural support for the body; as a person ages, BMD decreases and can lead to risk of pathological bone fractures |
|
|
|
Osteopenia |
BMD is lower than normal peak of bone mineral density, but not low enough to be classified as osteoporosis |
|
|
|
Osteoporosis |
Progressive condition where the BMD is very low and there is an increased risk for bone fractures |
|
|
|
What are the different classifications of fractures? |
Simple Compound Greenstick Communited Spiral |
|
|
|
What are the 4 stages of bone repair when a fracture occurs? |
1. Hematoma formation 2. Fibrocartilage callus formation 3. Bony callus formation 4. Bone remodeling |
|
|
|
What are the 5 classifications of bones? |
Long Sesamoid Flat Short Irregular |
|
|
|
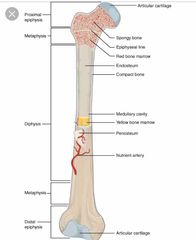
Long bone anatomy |
Back (Definition) |
|
|
|
Spinal regions |

Back (Definition) |
|
|
|
Closed reduction |
Manual manipulation of a broken bone to set it into its natural position without surgery |
|
|
|
Diaphysis |
Tubular shaft that runs between the proximal and distal ends of a long bone |
|
|
|
Diploe |
Layer of spongy bone that is sandwiched between two layers of compact bone found in flat bones |
|
|
|
Endosteum |
Delicate membranous lining of a bones medullary cavity |
|
|
|
Epiphysis |
Wide section at each end of long bone; filled with spongy bone and red marrow |
|
|
|
External callus |
Collar of hyaline cartilage and bone that forms around the outside of a fracture |
|
|
|
Internal callus |
Finbrocartilaginous matrix, in the endosteal region between the 2 ends of a broken bone |
|
|
|
Modeling |
Process during bone growth by which bone is resorbed on one surface of a bone and deposited on another |
|
|
|
Open reduction |
Surgical exposure of a bone to reset a fracture |
|
|
|
Osteoid |
Uncalcified bone matrix secreted by osteoblasts |
|
|
|
Perichondrium |
Membrane that covers cartilage |
|
|
|
Periosteum |
Fibrous membrane covering the outer surface of bone and continuous with ligaments |
|
|
|
Projection |
Bone markings where part of the surface sticks out above the rest of the surface where tendons and ligaments attach |
|
|
|
Proliferative zone |
Region of the epiphyseal plate that makes new chondrocytes to replace those that die at the diaphyseal end of plate and contributes to longitudinal growth of epiphyseal plate |
|
|
|
Remodeling |
Process by which osteoclasts resorb old or damaged bone at the same time as and on the same surface where osteoblasts form new bone to replace that which is resorbed |
|
|
|
Reserve zone |
Region of epiphyseal plate that anchors the plate to Osseous tissue of the epiphysis |
|
|
|
Secondary ossification center |
Region of bone development in the epiphyses |
|
|
|
Zone of calcified matrix |
Region of epiphyseal plate closest to diaphyseal plate; functions to connect the epiphyseal plate to the diaphysis |
|
|
|
Zone of maturation and hypertrophy |
Region of epiphyseal plate where chondrocytes from proliferative zone grow and mature and contribute to longitudinal growth of growth plate |
|
|
|
Vitamin K |
Supports bone mineralization and may have synergistic role with vitamin D |
|
|
|
Normal blood calcium level? |
10mg/dL is critical for normal body functions |
|
|
|
Hormones that affect the skeletal system? |
Growth hormone Thyroxine Sex hormones Calcitriol Parathyroid hormone Calcitonin |
|
|
|
Growth hormone |
Increases length of long bones, enhances mineralization, and improves bone density |
|
|
|
Thyroxine |
Stimulates bone growth and promotes synthesis of bone matrix |
|
|
|
Sex hormones |
Promote osteoblastic activity and production of bone matrix; responsible for adolescent growth spurt; promote conversion of epiphyseal plate to epiphyseal line |
|
|
|
Calcitriol |
Stimulates absorption of calcium and phosphate from digestive tract |
|
|
|
Parathyroid hormone |
Stimulates osteoclast proliferation and resorption of bone by osteoclasts; promotes reabsorption of calcium by kidney tubules; indirectly increases calcium absorption by small intestine |
|
|
|
Calcitonin |
Inhibits osteoclast activity and stimulates calcium uptake by bones |
|
|
|
Calcium |
Needed to make calcium phosphate and calcium carbonate which form hydroxyapatite crystals that give bones their hardness |
|
|
|
Calcium |
Needed to make calcium phosphate and calcium carbonate which form hydroxyapatite crystals that give bones their hardness |
|
|
|
Vitamin D |
Needed for calcium absorption |
|
|
|
Magenesium |
Structural component of bone |
|
|
|
Fluoride |
Structural component of bone |
|
|
|
Omega 3 fatty acids |
Reduces inflammation that may interfere with osteoblast function |
|
|
|
Transverse fracture |
Occurs straight across the long axis of the bone |
|
|
|
Oblique fracture |
Occurs at an angle that is not 90 degrees |
|
|
|
Oblique fracture |
Occurs at an angle that is not 90 degrees |
|
|
|
Spiral fracture |
Bone segments are pulled a part as a result of twisting motion |
|
|
|
Comminuted fracture |
Several breaks may result in many small pieces between two large segments |
|
|
|
Comminuted fracture |
Several breaks may result in many small pieces between two large segments |
|
|
|
Impacted fracture |
One fragment is driven into the other usually as a result of compression |
|
|
|
Greenstick fracture |
Partial fracture where only one side of the bone is broken |
|
|
|
Compound or open fracture |
At least one end of the broken bone tears through the skin |
|
|
|
Compound or open fracture |
At least one end of the broken bone tears through the skin |
|
|
|
Closed or simple fracture |
Fracture in which skin remains intact |
|
|
|
Pagets disease |
Leg bones are porous and curved |
|
|
|
Long bones function? |
Leverage |
|
|
|
Long bones function? |
Leverage |
|
|
|
Short bones function? |
Provide stability, support, allows some motion |
|
|
|
Long bones function? |
Leverage |
|
|
|
Short bones function? |
Provide stability, support, allows some motion |
|
|
|
Flat bone function? |
Points of attachment for muscles; protectors of internal organs |
|
|
|
Long bones function? |
Leverage |
|
|
|
Short bones function? |
Provide stability, support, allows some motion |
|
|
|
Flat bone function? |
Points of attachment for muscles; protectors of internal organs |
|
|
|
Irregular bone function? |
Protect internal organs |
|
|
|
Long bones function? |
Leverage |
|
|
|
Short bones function? |
Provide stability, support, allows some motion |
|
|
|
Flat bone function? |
Points of attachment for muscles; protectors of internal organs |
|
|
|
Irregular bone function? |
Protect internal organs |
|
|
|
Sesamoid bones function? |
Protect tendons from compressive forces |
|

