![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
104 Cards in this Set
- Front
- Back
|
The skin is also known as the integument, whereas the integumentary system consists of the skin and its accessory organs--the hair, nails, and cutaneous glands. |
True |
|
|
What is the scientific study and medical treatment of the integumentary system called? |
dermatology |
|
|
The skin is the body's largest and heaviest organ. In adults, it covers an area of 1.5 to 2.0 m2 and accounts for about 15% of the body weight. |
true |
|
|
What are the two layers of skin? |
a stratified squamous epithelium called the epidermis.
a deeper connective tissue layer called the dermis.
below the dermis is another connective tissue layer, the hypodermis, which is not part of the skin but is studied in conjunction with it. |
|
|
most of the skin is 1 to 2 mm thick, but it ranges from less than 0.5 mm on the eyelids to 6mm between the shoulder blades. The difference is due mainly to variation in thickness of the dermis, although skin is classified as thick or thin based on the relative thickness of the epidermis alone. |
true |
|
|
describe thick skin |
it covers the palms, soles, and corresponding surfaces of the fingers and toes. Its epidermis alone is about 0.5mm thick, due to a very thick surface layer of dead cells called the stratum corneum. It has sweat glands but no hair follicles or sebaceous (oil) glands. |
|
|
Describe thin skin |
has an epidermis about 0.1mm thick, with a thin stratum corneum. It possesses hair follicles, sebaceous glands, and sweat glands. |
|
|
what are stratum corneum? |
very thick surface layer of dead skin cells. |
|
|
What are the functions of skin? |
-Resistance to trauma and infection -Other barrier functions (water, ultraviolet rays, chemicals etc) -Vitamin D synthesis -Sensation -Thermoregulation -Nonverbal communication |
|
|
What is the acid mantle of the skin? |
The acid mantle is a protective acidic film on the skin. Bacteria and fungi colonize the skin's surface, but their numbers are kept in check by its relative dryness, its slight acidity (pH 4-6), and certain defensive antimicrobial peptides called dermcidin and defensins.
|
|
|
The skin carries out the first step in the synthesis of vitamin D, which is needed for bone development and maintenance. Where is the process completed? |
in the liver and kidneys |
|
|
What are thermoreceptors? |
Cutaneous nerve endings that monitor the body surface temperature. |
|
|
describe the epidermis |
a keratinized stratified squamous epithelium. That is the surface consist of dead cells packed with the tough protein keratin. Like other epithelia, the epidermis lacks blood vessels and depends on the diffusion of nutrients from the underlying connective tissue (hypodermis or subcutaneous fat). |
|
|
epi
derm |
epi = above, upon
derm = skin |
|
|
integument
dermat
logy |
integument = covering
dermat = skin; logy = study of
|
|
|
Cells of the epidermis |
Stem Cells
Keratinocytes
Melanocytes
Tactile cells
Dendrite cells |
|
|
stem cells |
undifferentiated cells that divide and give rise to the keratinocytes. They are found only in the deepest layer of the epidermis, called the stratum basale. |
|
|
keratinocytes |
the great majority of epidermal cells. They are named for their role in synthesizing keratin. |
|
|
Melanocytes |
These are also found only in the stratum basale. They synthesize the brown to black pigment melanin. |
|
|
Tactile cells |
receptors for touch. Also found in the basal layer. The tactile cell and its nerve fiber are collectively called tactile disc. |
|
|
Dendritic cells |
found in two layers of the epidermis called the stratum spinosum and stratum granulosum. They are immune cells that originate int eh bone marrow but migrate to the epidermis and epithelia of the oral cavity, esophagus, and vagina. They stand guard against toxins, microbes, and other pathogens that penetrate into the skin. If detected, they alert the immune system. |
|
|
What are the layers of the epidermis? |
Stratum corneum
stratum lucidum
stratum granulosum
stratum spinosum
stratum basale
|
|
|
In most skin, which stratum is the thickest? |
Stratum spinosum |
|
|
dendr |
dendr = tree, branch |
|
|
lucid |
lucid = light, clear |
|
|
what four important developments occur in the stratum granulosum? |
1. Keratohyalin granules release a protein called filaggrin that binds the cytoskeletal keratin filaments together into coarse, tough bundles. 2. The cells produce a tough layer of envelope proteins just beneath the plasma membrane, resulting in a nearly indestructible protein sac around the keratin bundles. 3. Membrane-coating vesicles release a lipid mixture that spreads out over the cell surface and waterproofs it. 4. Finally, as these barriers cut thekeratinocytes off from the supply of nutrients fro below, their organelles degenerate and the cells die, leaving just the tough waterproof sac enclosing coarse bundle of keratin. |
|
|
What is Dandruff? |
Dead keratinocyes exfoliate (flake off) from the epidermal surface as specks called dander. Dandruff is composed of clips of dander stuck together by sebum (oil). |
|
|
dermato
phag |
Dermato = skin; phag = eat |
|
|
Pap
illa |
pap = nipple; illa = little |
|
|
dermal papille |
the upward waves that are fingerlike extensions of the dermis. |
|
|
epidermal ridges |
the downward waves that are extensions of the epidermis |
|
|
reti
cul |
reti = network; cil = little |
|
|
hypo
derm |
hypo = below; derm = skin |
|
|
two ZONES of the dermis |
papillary layer
reticular layer |
|
|
papillary layer |
a thin zone of areolar tissue in and near the dermal papillae. This loosely organized tissue allows for mobility of leukocytes and other defenses against organisms introduced through breaks in the epidermis. This layer is especially rich in small blood vessels. |
|
|
recticular layer |
The reticular layer of the dermis is deeper and much thicker. It consists of dense irregular connective tissue. The boundary between the papillary and reticular layers is often vague. |
|
|
hypodermis or subcutaneous layer |
a layer beneath the skin that generally has more areolar and adipose tissue. It pads the body and binds the skin to the underlying tissues. |
|
|
Subcutaneous fat |
hypodermis composed predominantly of adipose tissue. It serves as an energy reservoir and thermal insulation. It is not uniformly distributed; for example, it is virtually absent from the scalp but relatively abundant in the breasts, abdomen, hips, and thighs. The subcutaneous fat averages about 8% thicker in women than in men, and varies with age. |
|
|
Epidermis |
Keratinized stratified squamous epithelium |
|
|
stratum corneum |
Dead, keratinized cells of the skin surface |
|
|
stratum lucidum |
Clear, featureless, narrow zone seen only in thick skin |
|
|
stratum granulosum |
Two to five layers of cells with dark-staining keratohyalin granules; scanty in the skin. |
|
|
stratum spinosum |
Many layers of keratinocytes, typically shrunken in fixed tissues but attached to each other by desmosomes, which give them a spiny look; progressively flattened the farther they are from the dermis. Dendritic cells are abundant here but are not distinguishable in routinely stained preparations. |
|
|
stratum basale |
Single layer of cuboidal to columnar cells resting on basement membrane; site of most mitosis; consists of stem cells, keratinocytes, melanocytes, and tactile cells, but these are difficult to distinguish with routine stains. Melanin is conspicuous in keratinocytes of this layer in black to brown skin. |
|
|
dermis |
Fibrous connective tissue, richly endowed with blood vessels and nerve endings. Sweat glands and hair follicles originate here and in hypodermis. |
|
|
Papillary layer |
Superficial one-fifth of dermis; composed of areolar tissue; often extends upward as dermal papillae. |
|
|
Reticular layer |
Deeper four-fifths of dermis; dense irregular connective tissue. |
|
|
Hypodermis |
Areolar or adipose tissue between skin and muscle. |
|
|
two forms of melanin |
a brownish black eumelanin
a reddish yellow sulfur-containing pigment, pheomelanin |
|
|
explain dark skin color |
People of different skin colors have essentially the same number of melanocytes, but in dark skin, the melanocytes produce greater quantities of melanin, the melanin granules in the keratinocytes are more spread out than tightly clumped, and the melanin breaks down more slowly. Thus, melanized cells may be seen throu |
|
|
Hair is divisible into three zones along its length: |
(1) the bulb, a swelling at the base where the hair originates in the dermis or hypodermis; (2) the root, which is the remainder of the hair within the follicle; and (3) the shaft, which is the portion above the skin surface. |
|
|
lan
vellus |
lan = down, wool
vellus = fleece |
|
|
dermal papilla |
a bud of vascular connective tissue that provides the hair with its sole source of nutrition. The hair bud grows around the dermal papilla. |
|
|
hair matrix |
a region of mitotically active cells immediately above the papilla which is the hair's growth center. |
|
|
in a cross section the hair reveals up to three layers: |
medulla
cortex
cuticle |
|
|
The medulla |
a core of loosely arranged cells and air spaces. It is most prominent in thick hairs such as those of the eyebrows, but narrower in hairs of medium thickness and absent from the thinnest hairs of the scalp and elsewhere. |
|
|
The cortex |
constitutes most of the bulk of a hair. It consists of several layers of elongated keratinized cells that appear cuboidal to flattened in the cross section. |
|
|
The cuticle |
composed of multiple layers of very thin, scaly cells that overlap each other like roof shingles with their free edges directed upward. |
|
|
The follicle is a diagonal tube that dips deeply into the dermis and sometimes extends as far as the hypodermic. It has two principal layers: |
epithelial root sheath
connective tissue root sheath |
|
|
The bulge of the epithelial root sheath |
a source of stem cells for follicle growth |
|
|
Hair receptors |
Nerve fibers which entwine each follicle and respond to hair movements. |
|
|
pilorector muscle (pilomotor muscle or arrector pili)
pili = of hair |
a bundle of smooth muscle cells extending from dermal collagen fibers to the connective tissue root sheath of the follicle. |
|
|
A given hair goes through a hair cycle consisting of three developmental stages: |
anagen
catagen
telogen |
|
|
anagen |
at any given time about 90% of the scalp follicles are in the anagen stage. In this stage, stem cells from the bulge in the follicle multipy and travel downward, pushing the dermal papilla deeper into the skin and forming the epithelial root sheath. Root sheath cells directly above the dermal papilla form the hair matrix. Here, sheath cells directly above the dermal papilla form the hair matrix. Here, sheath cells transform into hair cells, which synthesize keratin and then die as they are pushed upward away from the papilla. |
|
|
catagen stage |
Mitosis in the hair matrix ceases and sheath cells below the bulge die. The follicle shrinks and the dermal papilla draws up toward the bulge. The base of the hair keratinizes into a hard club and the hair, now known as a club hair, loses its anchorage. |
|
|
telogen |
This is the stage when the papilla reaches the bulge and the hair goes into a resting period. |
|
|
alopecia |
Thinning of the hair, or baldness.
Occurs to some degree in both sexes and may be worsened by disease, poor nutrition, fever, emotional stress, radiation, or chemotherapy. |
|
|
Pattern baldness |
condition in which hair is lost from select regions of he scalp rather than thinning uniformly across the entire scalp. |
|
|
hirsutism |
excessive or undesirable hairiness in areas that are not usually hairy, especially in women and children. |
|
|
ana gen cata telo alopecia hirsut |
ana = up; gen = build, produce cata = down telo = end alopecia = fox mange hirsut = shaggy |
|
|
fingernails and toenails are clear, hard derivatives of the ____________ |
Stratum corneum |
|
|
hyponychium
hypo = below; onych = nail |
the epidermis of the skin underlying the nail plate |
|
|
how fast does the fingernail grow? |
1 mm per week. Toenails are slightly slower. |
|
|
How can the appearance of the fingertips and nails be valuable in medical diagnosis? |
The fingertips become swollen or clubbed in response to long-term hypoxemia -- a deficiency of oxygen in the blood stemming from conditions such as congenital heart defects and emphysema. Dietary deficiencies may be reflected in the appearance of the nails. An iron deficiency, for example, may caue them to become flat or concave (spoon like) rather than convex. |
|
|
lunule
lun = moon; ule = little |
The opaque white crescent at the proximal end of a nail. |
|
|
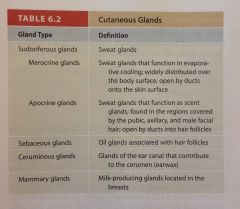
The skin has five kinds of glands: |
merocrine sweat glands
apocrine sweat glands
sebaceous glands
ceruminous glands
mammary glands |
|
|
Sudoriferous (sweat) glands, are of two kinds:
sudor = sweat
fer = carry, bear |
apocrine
merocrine |
|
|
apocrine glands |
Occur in groin, anal region, axilla, and areola, and in mature males, in the beard area. Ducts lead into nearby follicles rather than directly to the skins surface. They do not use apocrine mode of secretion. They use exocytosis. Sweat is thicker and more milky because it has more fatty acids in it. They are scent glands that respond especially to stress and sexual stimulation. They secrete sex pheromones. |
|
|
bromhidrosis |
disagreeable body odor |
|
|
Merocrine (eccrine) sweat glands |
Over entire body, especially abundant on the palms, soles, and forehead. Function to cool the body. Excrete some of the same wastes as the kidneys. There are 3 to 4 million merocrine sweat glands in the adult skin, with a total mass about equal to one kidney. |
|
|
Myoepithelial cells |
Specialized cells found in both apocrine and merocrine sweat glands and found amid the secretory cells at the deep end of the gland. These squeeze the base of the gland, and force perspiration up the duct---particularly under conditions of over heating, nervousness, or arousal. |
|
|
Perspiration is about 99% water and has a pH ranging from 4 to 6, contributing the acid mantle that inhibits bacterial growth on the skin. |
True |
|
|
insensible perspiration |
the fact that perspiration evaporates about as fast as it is produced, so it is no notice. |
|
|
diaphoresis
dia = through; phoresis = carrying |
Under such conditions as heat, exercise, and circulatory shock, more copious sweat is produced and noticeably wets the skin. |
|
|
Sebaceous glands
seb = fat, tallow; aceous = possessing |
produce an oily secretion called sebum. They are flask-shaped, with short ducts that usually open directly onto the skin surface. These are holocrine glands with little visible lumen. Sebum keeps the skin and hair from becoming dry, brittle, and cracked. |
|
|
Ceruminous glands
cer = wax |
found only in the external ear canal, where their secretion combines with sebum and dead epidermal cells to form earwax, or cerumen. |
|
|
Mammary glands |
modified apocrine sweat glands that produce a richer secretion and channel it through ducts to a nipple for more efficient conveyance to the offspring. |
|
|
Cutaneous Glands |
|
|
|
Skin Cancer |
Befalls one out of five people in the US. UV radiation from the sun damages DNA and disables protective tumor suppressor genes in the epidermal cells. One of the most common cancers, but one of the easiest to treat. |
|
|
There are three types of skin cancer named for the epidermal cells in which they originate:
These three type are also distinguished from each other by the appearance of their lesions (zones of tissue injury) |
basal cell carcinoma
squamous cell carcinoma
melanoma |
|
|
Basal cell carcinoma |
Most common type. Least deadly because it seldom metastasizes, but if neglected, it can severely disfigure the face. The lesion first appears as a small, shiny bump. As the bump enlarges, it often develops a central depression and a beaded "pearly" edge. |
|
|
Squamous cell carcinoma |
Arises from keratinocytes of the stratum spinosum. Lesions usually appear on the scalp, ears, lower lip, or back of the hand. They have a raised, reddened, scaly appearance, later forming a concave ulcer with raised edges. If untreated, tends to metastasize to the lymph nodes and can be lethal. |
|
|
Melanoma |
A skin cancer that arises from the melanocytes. It accounts for no more than 5% of skin cancers, but it is extremely aggressive and drug-resistant. Can be treated surgically if caught early, but if it metastasizes--which it does quickly--it is unresponsive to chemotherapy and is usually fatal. The average person with metastatic melanoma lives only 6 months from diagnosis, and only 5% to 14% of patients survive with it for 5 years. |
|
|
lesio
carcin
oma |
lesio = injure
carcin = cancer; oma = tumor |
|
|
Cancer Society suggest an "ABCD rule" for recognizing melanoma: |
"A" for asymmetry (one side different)
"B" for border irregularity (contour is not uniform but wavy or scalloped)
"C" for color (mixture of brown, black, tan and sometimes red and blue)
"D" for diameter (greater than 6mm) |
|
|
Burns |
The leading cause of accidental death. Burn deaths result primarily from fluid loss, infection, and the toxic effects of eschar--the burned, dead tissue. |
|
|
Burns are classified according to the depth of tissue involvement: |
First-degree
Second-degree
Third-degree |
|
|
First-degree burns |
involve only the epidermis and are marked by redness, slight edema, and pain. (sunburns)
known as partial-thickness burns |
|
|
Second-degree burns |
involve the epidermis and part of the dermis but leave at least some of the dermis intact. Known as partial-thickness burns. Severe sunburns and many scalds are second-degree burns. |
|
|
Third-degree burns (full-thickness burns) |
The epidermis and all of the dermis, and often some deeper tissues (muscle and bone) are destroyed. These are sometimes called fourth-degree burns. The skin can only regenerate from the edges because no dermis remains. |
|
|
The two most urgent considerations in treating a burn patient are: |
fluid replacement
infection control |
|
|
A patient may lose up to 75% of the blood plasma within a few hours, potentially leading to circulatory shock and cardiac arrest--the principal cause of death in burn patients. |
TRUE |
|
|
Eschar |
a slough or piece of dead tissue that is cast off from the surface of the skin, particularly after a burn injury, but also seen in gangrene, ulcer, fungal infections, necrotizing spider bite wounds, and exposure to cutaneous anthrax. |
|
|
debridement
de = un; bride = bridle |
medical removal of dead, damaged, or infected tissue to improve the healing potential of the remaining healthy tissue. |

