![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
Where is the precordium? Where is the apical impulse of the heart found?
|
Area of skin anterior to the heart. Apical impulse is found in the left intercostal space lateral to the sternum.
|
|
|
What is responsible for the sound of S1?
|
The first heart sound (S1) is produced by the closure of the AV valves - tricuspid & mitral.
|
|
|
What is responsible for the sound of S2?
|
The second heart sound (S2) is produced by the closure of the semilunar valves - aortic & pulmonic.
|
|
|
What is the order of valve opening/closing in the cardiac cycle?
|
McTc-PoAo-AcPc-ToMo. (palindrome sequence)
|
|
|
What is an ECG?
|
Electrocardiogram, measures electrical stimulation of the heart.
|
|
|
What does depolarization refer to in the heart?
|
Spread of electrical stimulaton through the heart (heart contracts).
|
|
|
What does repolarization refer to in the heart?
|
Return of stimulated heart cells to resting state (heart relaxes).
|
|
|
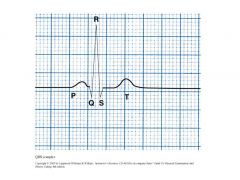
Describe a normal ECG?
|
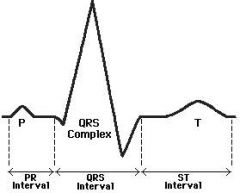
P wave - atrial depolarization (contraction). QRS complex - ventricular depolarization (contraction). ST segment and T wave - ventricular repolarization (recovery).
|
|
|
Where do the heart sounds align on an ECG?
|

S1 beats at about the Q peak. S2 beats at the end of T wave.
|
|
|
What is preload?
|
Volume of blood that stretches the ventricle before contraction (end diastolic volume). Preload is increased by blood volume expasion.
|
|
|
What is afterload?
|
Degree of vascular resistance to ventricular contraction. Resistance is reflected by tone of the arterial walls and volume of blood in the vascular tree.
|
|
|
What is myocardial contractility?
|
Ability of the cardiac muscle to shorten (contract) when given a load.
|
|
|
What is JVP?
|
Jugular venous pressure, reflects central venous pressure (CVP).
|
|
|
What is venous pressure from?
|
Ultimately from LV contraction, but also blood volume and RV contractility.
|
|
|
Which veins are used to estimate JVP?
|
Internal jugular veins.
|
|
|
What is a normal JVP (CVP)?
|
5-9 mm Hg or 0-4 cm cm above the sternal angle.
|
|
|
What is superior vena cava syndrome?
|

Swelling in the face and arms due an obstruction of the superior vena cava. Usually caused by a tumor. Intially veins may be distended, but are covered up after by edema.
|
|
|
Describe the jugular venous pulsations. (a,c,x,v,y)
|
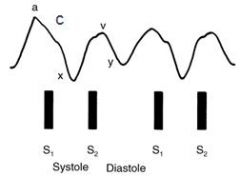
a wave = atrial contraction; c wave = closure of tricuspid valve; x descent = atrial relaxation; v wave = atrial venous filling; y descent = atrial emptying.
|
|
|
Describe arterial pressure wave form.
|
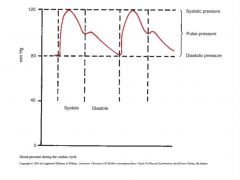
Middle hump is due to the recoil wave generated by the closing of the semilunar (aortic) valves.
|
|
|
What are some differences between the internal jugular vein and carotid artery pulsations?
|
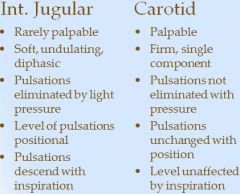
|
|
|
What are thrills?
|
Vibratory pulsation associated with murmurs or bruits felt when doing cardiac palpation.
|
|
|
What are heaves or lifts?
|
Associated with hyper dynamic muscle or hypertrophy
|
|
|
What is PMI? Where is it and how is it found?
|
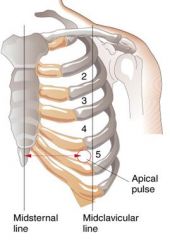
Point of maximal impulse. Hand is placed over the area of the left 5th intercostal space at about the midclavicular line. Once it is felt and located, one finger is placed on it to palpate it.
|
|
|
What and where are the areas of the heart that are palpated?
|
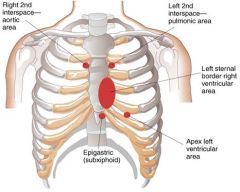
|
|
|
How is the systolic impulse of the right ventricle palpated?
|
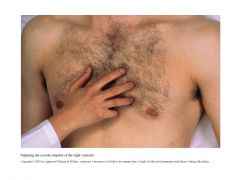
|
|
|
What is measured when palpating the PMI?
|
Diameter (normally 2.5 cm), amplitude (height/strength), duration (normally only 2/3rds of systole).
|
|
|
Describea hyperkinetic apical impulse? Hypokinetic? Sustained?
|

Hyperkinetic - lift; high amplitude. Hypokinetic - low amplitude, long duration. Sustained - long duration, high amplitude.
|

