![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
Differential of Cough
|
• Infection
– Bacterial, fungal, viral • Respiratory diseases – Asthma, COPD, chronic sinusitis • GI – Acid reflux • Medication side effect |
|
|
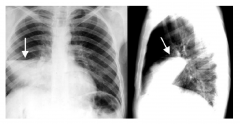
TB X-ray Pattern
|

• Miliary pattern for TB
• Named after “millet seeds” • “Lymphangitic spread” • Other illnesses can cause similar appearance |
|
|
Lobar Pneumonia X-Ray Pattern
|
• “Lobar pneumonia”
• Usually “typical bacteria” |
|
|
Atypical Pneumonia X-Ray Pattern
|

• “Atypical pneumonia”
pattern • “Ground glass” • Atypical bacteria • e.g.mycoplasma • e.g.PJP (PCP) |
|
|
Normal X-Ray Pattern
|

|
|
|
MTB Risk Factors
|
• Immunosuppression
– HIV, alcoholism, diabetes, chronic kidney disease • Endemic areas – Mexico, India, Philippines, China, Vietnam • Poverty • Malnutrition |
|
|
MTB
|
• Transmitted human-to-human via
aerosol droplets containing bacteria • Acid-fast aerobic rod (unique staining) • Infects and survives within alveolar macrophages for years-decades • Host response includes formation of granulomas to control infection • 2 billion individuals latently infected, 8 million active infections and 2 million deaths due to MTB annually |
|
|
MTB causes what types of infections?
|
Active or Latent Infections
|
|
|
Active cases of TB
|
Due to "Reactivation" from latent infections
|
|
|
Suppression of immune systems does what to TB?
|
Greatly increases incidence of active or reactivation disease
|
|
|
Characteristics of Active TB
|
• Active replication of bacteria within granuloma
• Granuloma becomes “liquified” due to exaggerated immune response to control infection • Cavitation can lead to expulsion of bacteria from lungs into sputum • Those with active disease infectious to transmit organism |
|
|
What type of individual has the most risk factors for MTB?
|
35 yo migrant worker from Mexico with diabetes, HIV seen in the ED for chronic cough with hemoptysis
|
|
|
Diagnosing TB: Sputum Smear
|
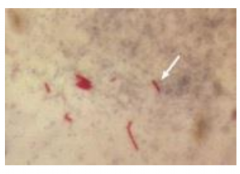
• AFB (Acid fast Bacillus)
• Requires ~ 5,000 bacilli per ml sputum for positive ID • However, HIV-infected individuals often test sputum smear negative |
|
|
Diagnostic Tests for TB
|
• Tuberculin skin test
• Interferon gamma release assay • AFB smear and culture • Nucleic acid amplification |
|
|
TST (Tuberculin Skin Test)
|
• TST > 5 mm (induration!)- HIV, recent
contacts active MTB,immunosuppressed (TX pts.), CXR c/w prior TB • TST> 10 mm- < 5 years from endemic area, IVDA, residents of jails, LTCF • TST > 15 mm- all others • Comment on anergy! |
|
|
TB: Interferon Gamma
|
• < .35 IU/ml- negative
• > .35 IU/ml- positive |
|
|
NAAT
|
DNA Amplification
Equipment reads intensity of fluorescent labeled probes Can also test for rifampin resistance |
|
|
Which one of these lab test results is
diagnostic of active MTB? |
Sputum smear negative for acid fast bacillus, but culture positive for growth and nucleic acid amplification (NAA) test positive for MTB
|
|
|
Treatment for TB
|
Isoniazid, Rifampin, Pyrazinamide and Ethambutol
|
|
|
How long is the initial phase of TB treatment?
|
2 months
|
|
|
How long is the continuation phase of treatment?
|
4-7 months
|
|
|
How does isoniazid exert its anti-tuberculous effect by inhibiting
|
mycolic acid synthesis
|
|
|
Why would you have a multiple drug cocktail and extended drug therapy duration for TB?
|
• Antibiotics targeting different molecules
• MTB grows very slowly, difficult to kill all of the bacteria • Antibiotics most effective on “actively” growing bacteria…not effective on latent or dormant bacilli • Minimize chance of developing antibiotic resistant variants |
|
|
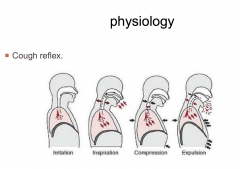
Cough Reflex
|
|
|
|
Acute Cough
|
Less than 3 weeks
|
|
|
Chronic Cough
|
More than 3 weeks
|
|
|
Common causes of acute cough
|
Common cold 60%
Acute Bronchitis 20% Asthma 10% COPD 4% Environmental irritants 2% Influenza 2% |
|
|
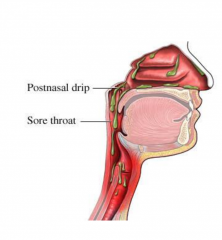
Common cause of Chronic Cough
|
Rhinitis
|
|
|
Clues that the cough is due to rhinitis
|
“ I cough when I have a runny nose.”
“I can feel something drip in the back of my throat.” “I have to constantly clear my throat.” “I cough more when I lay down.” |
|
|
Tonsils with a cobblestone pattern
|

Inflamed pharyngeal mucosa/adenoid glands
|
|
|
Allergic Rhinitis
|
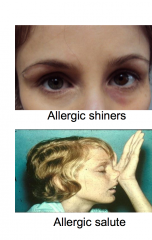
Related to Eczema , Asthma.
Have an itchy nose. Positive skin test and RAST test. Clear discharge |
|
|
Immunology of Allergy
|

|
|
|
Gustatory Rhinitis
|
Triggered by eating
|
|
|
Inflammatory Rhinitis - but no elevated IgE in serum
|
Local tissues may show elevated IgE
|
|
|
Treatment of nasal steroids
|
Beclomethasone, Fluticasone
Binds to intracellular receptors, reduce inflammatory mediators |
|
|
Oral antihistamines
|
Benadryl, Loratidine
Down regulates H1 receptors, decrease inflammatory mediators |
|
|
Cromolyn Sodium
|
Mast cell stabilizer
|
|
|
Nasal Ipratropium
|
Reduces Substance P
|
|
|
Leukotriene Inhibitors
|
Montelukast
|
|
|
GERD
|
In 30% of chronic cough
Esophageal-tracheobronchial cough reflex. ( Chemo receptors in the lower esophagus) Direct laryngeal irritation. ( Chemo/mechanical receptors receptors) Aspiration of gastric acid. ( Chemo/mechanical receptors receptors) |
|
|
GERD Treatment
|
Weight loss , elevation of head of bed , Avoiding certain foods.
Antacids: calcium carbonate H1 blockers: Famotidine Proton pump inhibitors: Omeprazole Surgical : Nissen fundoplication, Vagotomy , Gastric bypass |
|
|
How do ACE-I cause cough?
|
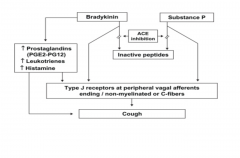
|
|
|
An 80-year-old female with past history of
Mycobacteria tuberculosis infection develops a productive cough that is blood tinged. The patient has a temperature of 39.4° C. A chest radiograph was performed and was significant for bilateral interstitial infiltrates. Sputum is collected to determine if there has been a reactivation of her past Mycobacteria tuberculosis infection. What stain should be performed because of its increased sensitivity in this case? Which stain should you use? |
Auramine-rhodamine stain
|
|
|
A 20-year-old white man presents to the
hospital complaining of a 1-month history of tingling sensations in his legs. He is on treatment for pulmonary tuberculosis with isoniazid. On examination you note a greasy yellow scale over his scalp and eyebrows. Laboratory investigations reveal a hemoglobin of 9 g/dl. What is the most likely diagnosis? |
Pyridoxine Deficiency
|
|
|
A 45-year-old man suffering from viral hepatitis
requires being started on antitubercular therapy for pulmonary tuberculosis. He has icterus with hepatomegaly, and his liver function tests are moderately deranged. What antitubercular drug combination is safest for this patient? |
Isoniazid + Streptomycin
|
|
|
A 36-year-old man is admitted to isolation for
treatment of pulmonary tuberculosis, detected at a routine checkup the day before. He works at a construction site and has not been in contact with any farm animals. Besides treatment, he needs to be aware of the most common way to transmit the disease. What contamination is usually responsible for spread of the disease? |
Aerosol droplets
|
|
|
An outbreak of respiratory illness occurred in
a day-care center involving children who had not completed the primary vaccination series. The illness was characterized by catarrhal symptoms followed by paroxysmal cough. The etiological agent of the outbreak was a small Gram-negative coccobacillus that was isolated from the nasopharyngeal aspirates of children in the early phase of the illness. Bordet Gengou medium was the selective medium used for isolating the bacterial agent. What is a characteristic of this bacterial species that caused the outbreak? |
Can produce a symptomatic infection in adults
|
|
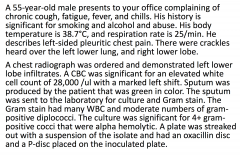
These results indicate that the organism
causing the pulmonary infection in this patient is what? |
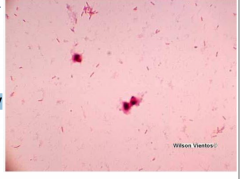
Streptococcus pneumoniae
|
|
|
A 45-year-old individual with a 20 pack-year history of
smoking presents because of a chronic cough. The cough has been worsening for the past 3 months. The patient does not have a primary care physician and usually visits the ER for exacerbations of his cough. What type of epithelium would be anticipated lining the larynx in this individual? |
Stratified squamous
|
|
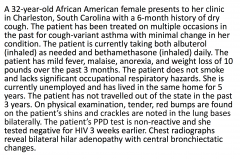
Most likely diagnosis?
|
Sarcoidosis
|
|
|
A 28-year-old woman presents with an itchy throat,
prolonged sneezing episodes, watery red eyes, and inflamed nasal membranes. Her temperature is normal and a throat culture is negative. She is most likely suffering from allergic rhinitis. Her physician will most likely prescribe diphenhydramine. To what class of compounds does the drug of choice belong? |
Antihistamine (H1)
|
|
|
A 28-year-old woman visits her doctor's office
complaining of an itchy throat, prolonged sneezing episodes, watery red eyes, and inflamed nasal membranes. Her temperature is normal and a throat culture is negative. She is most likely suffering from allergic rhinitis. Her physician will most likely prescribe which of the following? |
Diphenhydramine
|
|
|
A 45-year-old individual with a 20 pack-year history
of smoking presents because of a chronic cough. The cough has been worsening for the past 3 months. The patient does not have a primary care physician and usually visits the ER for exacerbations of his cough. What type of epithelium would be anticipated lining the larynx in this individual? |
Stratified Squamous
|

