![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
List three indications for intubation. |
Failure to maintain or protect the airway |
|
|
How is the patient’s ability to maintain or protect the airway evaluated? |
- Ability to phonate |
|
|
What are the reported failure rates for intubation in the emergency department (from NEAR studies)? |
Medical intubations: 1% |
|
|
What is estimated incidence of can’t intubate, can’t ventilate situation (in elective anesthesia cases)? |
- 1/5000 to 1/200 000 |
|
|
The difficulty of what three maneuvers should be assessed preintubation? |
1. Difficult intubation |
|
|
What does the pneumonic “LEMON” stand for in the evaluation of the difficult airway? |
Look externally, especially for signs of difficult intubation (by gestalt), difficult bag mask ventilation, and difficult cricothyrotomy Evaluate the ‘3-3-2 rule’ Mallampati Obstruction Neck mobility |
|
|
What does the pneumonic “MOANS” stand for in evaluation for difficult BVM? |
Mask seal Obesity Aged No teeth Stiffness (resistance to ventilation) |
|
|
List conditions which increases stiffness of resistance to ventilation. |
- Asthma/ COPD |
|
|
What is the RODS mnemonic for difficult LMA? |
· Restricted mouth opening, Obstruction, Distorted anatomy, Stiff lungs |
|
|
List predictors of difficult cricothyrotomy. ADD RODS |
- Disturbance of the ability to locate and access the landmarks of the anterior airway via the neck o Obesity 0 N
o Prior surgery
o Subcutaneous emphysema |
|
|
Direct laryngoscopy to visualize the glottis requires the alignment of what three axis? |
1. Oral axis |
|
|
What is required anatomically to align the oral, pharyngeal, and laryngeal axis? |
- Adequate mouth opening |
|
|
Describe the 3-3-2 rule for evaluating difficult laryngoscopy? |
Mouth opening: 3 fingers |
|
|
Describe the Mallampati score. |
Class I: |
|
|
What is the Cormack and Lehane grading scheme for larygoscopic view? |
Grade 1: |
|
|
List methods to confirm endotracheal tube placement. |
Primary:
Secondary: |
|
|
What are some causes of false positive and false negative colorimetric ETCO2 devices? |
· False positive |
|
|
Name false positives and false negatives for the EDD (*note a true positive is considered when the tube is in the esophagus) |
· False positive |
|
|
emergency airway algoritm |

|
|
|
crash airway algorithm |

|
|
|
Define failed airway. |
- Oxygen desaturation below 90% despite good two person BVM |
|
|
DIfficult airway algortim |
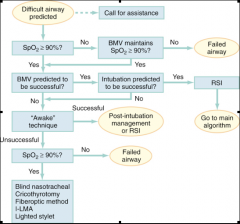
|
|
|
Failed airway algorithm |
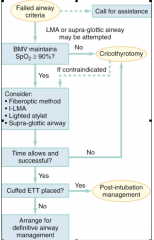
|
|
|
What is “double set-up”? |
|
|
|
What is the desaturation time for fully preoxygenated normal adult, moderately-ill adult, obese adult, and child? |
- Normal adult: 8 min |
|
|
What are the six P’s of RSI? |
1. Preparation 2. Preoxygenation (8 vital capacity breaths or 3 minutes on 100%) 3. Pretreatment 4. Positioning / Protect (Sellick) 5. Paralysis with induction 6. Placement of tube 7.Post-intubation management |
|
|
List risk factors for rapid desaturation during RSI. |
Obese |
|
|
How is optimal preoxgenation achieved? |
- 100% O2 nonrebreather mask for 3 minutes or 8 tidal breath |
|
|
What are the pretreatment agents for RSI? |
· Reactive airways disease: Lidocaine: 1.5 mg/kg IV, to mitigate bronchospasm. Salbutamol 2.5 mg by nebulizer (if time permits and not already given).
|
|
|
RSI protocol |
0-10 Preparation 0-5 Preoxygenation 0-3 Pretreatment
|
|
|
What is the algorithm for laryngospasm? |
Try each step in successive order if the one before fails: |
|
|
What is the difference between depolarizing and nondepalarizing NMBAs? |
|
|
|
What is the chemical composition of succinylcholine? |
- Two molecules of ACh |
|
|
What is responsible for the breakdown of succinylcholine |
- Plasma pseudocholinesterase (not present at the motor endplate) |
|
|
List conditions and drugs that reduce the activity of pseudocholinesterase and therefore increase the quantity of succinylcholine being effective at the motor endplate? |
THINK of things that can damage the liver or inhibit it’s pseudocholinesterase production |
|
|
What conditions are associated with hyperkalemia after succinylcholine administration? |
Burns >10% BSA>5 days until healed
Crush injury>5 days until healed
Denervation (stroke, spinal cord injury)>5 days until 6 mo
Neuromuscular disease (ALS, MS)Indefinitely
Intra-abdominal sepsis>5 days until resolutio
Anesthesia lit says after 24 hrs do not use succ, ron walls says 3 days. Rosen’s is 5 days. |
|
|
What is the emergent treatment of malignant hyperthermia? |
- Stop offending agent and initiate active cooling |
|
|
List examples of the two classes of competitive NMBAs. |
Aminosteroid agents
Benzylisoquinolines |
|
|
Provide a rapid sequence protocol using etomidate and rocuronium. |
0-10 Preparation |
|
|
How is vecuronium dosed? |
- 0.3mg/kg IVP, or |
|
|
What medications and doses are good for post intubation maintenance of sedation? |
- Midazolam 0.1mg/kg |
|
|
Provide an RSI protocol for status asthmaticus. |
Prepare |
|
|
What medications blunt the sympathetic stimulation to laryngoscopy and intubation? |
- Fentanyl |
|
|
Outline an RSI protocol for intubation in a patient with elevated ICP. |
0-10 Preparation |
|
|
What is the incidence of cricothyrotomy in ED intubations? |
- ~1% |
|
|
List relative contraindictions to cricothyrotomy. |
- Distorted neck anatomy |
|
|
What are approximate size ETT tubes use for most adult males and females? |
- Males: 8.0-8.5 |
|
|
What is the name of the second hole at the end of the ETT tube that permits flow if the tip is occluded? |
- Murphy eye |
|
|
What are the functional differences between the Miller and Macintosh larygoscopes? |
|
|
|
What does “BURP” stand for? |
- Backwards, upwards, rightwards pressure |
|
|
Differentiate between BURP and cricoid pressure. |
- BURP is applied to the trachea and is designed to improve view of the glottis |
|
|
What does correct tube position usually correspond to in cm at the lips? |
- Men: 23cm (corner of mouth) |
|
|
What cuff pressure range should be maintained within the ETT balloon? |
- 20-40cm H2O |
|
|
List causes for absent CO2 detection in the properly intubated patient (false negative). |
- Cardiac arrest with poor chest compressions |
|
|
LIST causes of false positive CO2 detection. |
- Carbonated beverages |
|
|
List traumatic complications of endotracheal intubation. |
- Arytenoids avulsion, displacement |
|
|
How is translaryngeal anesthesia obtained? |
|
|
|
List sedative induction agents, their doses, induction times, durations, benefits and caveats. |
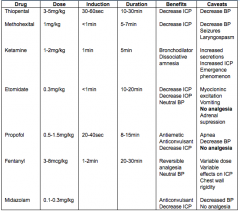
|
|
|
What is “emergence pohenomenon”? |
- Nightmares, visual hallucinations and dissociative sensations experienced by some patients when recovering from ketamine |
|
|
List complications of succinylcholine. |
|
|
|
How much will serum potassium rise during succinylcholine administration? |
- 0.5 mEq/L |
|
|
How does recent cocaine use potentially prolong paralysis with succinylcholine? |
- Cocaine is metabolized by plasma pseudocholinesterase reducing available enzyme for hydrolization of succinylcholine |
|
|
How are nondepolarizing NMBAs reversed? |
- Atropine 0.01mg/kg (prevent muscarinic side effects) |
|
|
Over what range of CPP is CBF normally maintained by cerebral autoregulation? |
- 50mmHg to 150mmHg |
|
|
What is the CPP equation? |
- CPP=MAP-ICP |
|
|
In traumatic brain injury what should the target MAP be? |
- >90mmHg |
|
|
What are potential complications of suctioning the ETT tube? |
- Hypoxia |
|
|
What is reasonable set of initial ventilator settings? |
|
|
|
What is treatment of post extubation larygospasm? |
- 100% O2 and positive pressure, 1/10th dose of succs |
|
|
Define cricothyrotomy. |
- Establishment of a surgical opening in the airway through the cricothyroid membrane and placement of a cuffed tracheostomy tube or ETT. |
|
|
List indications for cricothyrotomy. |
- Primary indication: |
|
|
List contraindication to cricothrotomy. |
- Absolute
|
|
|
What equipment is required for cricothyrotomy? |
- Trousseau dilator |
|
|
What are the basic steps of cricothyrotomy? |
|
|
|
What are important landmarks to identify when performing cicothyrotomy? |
- Laryngeal prominence and thyroid cartilage |
|
|
How far below the laryngeal prominence is the cricothyroid membrane (approximately)? |
|
|
|
How far above the sternal notch is the cricothyroid membrane (approximately)? |
- 4 finger widths |
|
|
How is the larynx immobilized during the procedure? |
- Between the thumb and long (middle) finger of the nondominant hand (L hand), or |
|
|
What direction is the initial incision recommended by The Airway Manual? |
- Vertical (2cm) |
|
|
List tissues cut with the initial vertical incision? |
- Skin |
|
|
How is the actual membrane incised? |
- 1cm horizontal stabbing incision (lower half of membrane) |
|
|
How is the Trousseau dilator used? |
1. Inserted well though the incision with blades directed longitudinally down the airway, or |
|
|
List complications of cricothyrotomy. |
|
|
|
What type and size tube do you want? |
- #4 Shiley (5mm diameter) |
|
|
Describe the location of the cricoithyroid membrane. |
- Between the cricoid and thyroid cartilages |
|
|
What vascular structure is at particular risk during cricothyoidotomy? |
- Thyroid ima artery |
|
|
What are the steps of needle cricothyroidotomy? |
|
|
|
What are some important things to know about intubating the 3rd trimester pregnant patient? |
|
|
|
What are some important things to know about intubating the morbidly obese patient |
? |
|
|
What are some important points in an airway foreign body obstruction? |
|

