![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Atresia? Fistula? |
Atresia: closing of lumen Fistula: opening of lumen |
|
|
Esophageal atresia with or without tracheoesophageal fistulas (TEF's) |
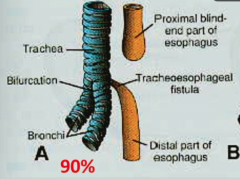
Failure in partitioning esophagus and trachea ~tracheoesophageal septum. Baby looks normal until you feed the baby!! Baby will vomit |
|
|
Polyhydromnios |
Too much fluid in amniotic cavity; detected before birth. Indicates blockage along GI tract which includes esophageal atresia/TEF Baby has to drink this amniotic fluid all the time to stimulate the GI development AND to digest fluid. If there is a blockage like esophageal atresia, baby will not drink the amniotic fluid and we see accumulation in amniotic cavity |
|
|
H type TEF |
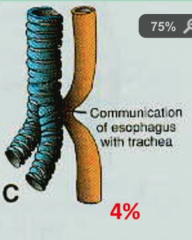
Looks like H Esophagus is continuous with trachea and bronchi |
|
|
VACTERL association |
Vertebral anomalies Anal atresia Cardiac defects Tracheoesophageal fistula (TEF's) Esophageal atresia Renal anomalies Limb defects *3 or more, dx'd with "VACTERL association" |
|
|
Epithelium of internal lining of trachea, bronchi, lungs, and larynx is entirely made of? |
endoderm (foregut origin) |
|
|
Cartilaginous, muscular, and connective tissue components of trachea, bronchi, lungs is derived from? |
splanchnic mesoderm surrounding foregut |
|
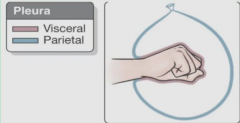
visceral pleura and parietal pleura are derived from? |
visceral pleura - splanchnic mesoderm parietal pleura - somatic mesoderm |
|
|
Pericardioperitoneal canals |
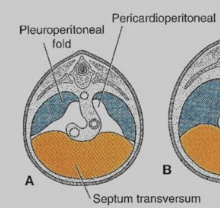
"Lung spaces": Lungs grow caudally in these spaces and then cease from the limit to abdomen Communication between thorax and abdomen |
|
|
Pleuropericardial folds |
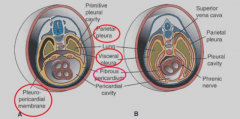
Heart and lung separates when these folds fuse |
|
|
Pleuroperitoneal folds |
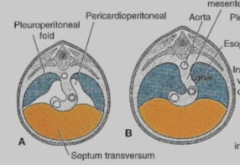
Fuses with septum transversum (primitive diaphragm) to separate thorax from abdomen |
|
|
Congenital Diaphragmatic Hernia |
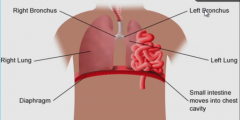
Failure of pleuroperitoneal folds fusing with septum transversum, causing a latch opening in baby's diaphragm due to the absence of a pleuroperitoneal membrane. GI moves upwards into the chest cavity usually on the posterior LEFT side of diaphragm Result: Pulmonary Hypoplasia |
|
|
Pulmonary Hypoplasia |
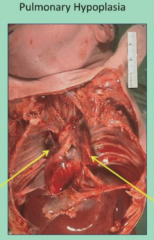
Pressure on lungs and heart leading to underdeveloped lungs baby dies |
|
|
Formation of diaphragm |
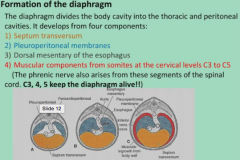
1. septum transversum 2. pleuroperitoneal (fuses with septum transversum) 3. dorsal mesentery of esophagus 4. C3 C4 C5 somites/ voluntary skeletal muscle **phrenic nerves motor diaphragm! |
|
|
1. Pseudoglandular period |
Week 5 to 16 branching continues no bronchioles no alveoli |
|
|
2. Canalicular period |
Week 16 - 26 simple cuboidal epithelia terminal bronchioles dividing into 2 or more, then into 3-6 alveolar ducts |
|
|
3. Terminal sac period |
Week 26 to birth cuboidal bronchioles --> thin flat cells blood/ lymph capillaries enter the terminal sacs creating primitive alveoli respiration possible!! Type 2 pneumocytes secrete surfactant |
|
|
Surfactant |
prevents lungs from collapsing reduces surface tension increases even more 2 weeks prior to birth steroids/ glucocorticoids can stimulate pneumocytes II to produce surfactant |
|
|
4. Alveolar period |
month 8- childhood number of terminal sacs steadily increasing Type 1 pneumocytes becoming thinner to allow capillaries/blood to come into alveolar sacs creating a blood-air barrier between epithelial and endothelial sacs mature alveoli not present before birth lungs are fluid filled |
|
|
post birth of lung maturation |
1. alveoli increase in size in first 10 years 2. bronchioles and alveoli number increasing 3. lung growth 4. majority alveoli formed post-birth 5. continuous formation of primitive alveoli via capillaries into alveolar sacs |
|
|
Respiratory distress syndrome |

Premature babies; 20% deaths among newborns Not enough surfactant Alveoli collapsed; baby cannot breathe Treatment: 1. artificial surfactant 2. glucocorticoid produces surfactant; stimulates pneumocytes 2 to produce it |
|
|
Pulmonary agenesis |
unilateral: absence of ONE lung, or lobe, or bronchi. usually associated with a cardiac defect or other condition 60% chance compatible w life bilateral: baby will die |
|
|
Congenital cysts |
cyst at terminal bronchi cyst- honeycomb appearance develop chronic infection |

