![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Increased peak pressure, normal plateau pressure
|
Kinked tube, bronchospasm
|
|
|
Peak and plateu pressure raised
|
Endobronchial intubation, Pneumothorax, bad lungs
(Overall, poor compliance). |
|
|
Define apneic threshold.
|
Note : this only occurs in anesthetized patients. It is the paco2 below which patients stop breathing. This needs clarification
|
|
|
Do central respiratory centers respond more to co2 or dissolved bicarb?
|
Bicarb - co2 doesn't cross bbb
|
|
|
What do peripheral chemoreceptors (aortic bodies, carotid bodies) react to?
|
Sensitive to changes in PaO2, PaCO2, pH, and arterial perfusion pressure. They interact with central respiratory centers via the glossopharyngeal nerves, producing reflex increases in alveolar ventilation in response to reductions in PaO2, arterial perfusion, or elevations in [H+] and PaCO2.
|
|
|
Which receptors - central or peripheral, react primarily to low o2 and which to high co2?
|
Central : high co2 (in the form of bicarb)
Peripheral : low o2 |
|
|
What is apenic threshold?
|
The co2 below which you stop breathing. For awake ppl, it's like 32 mmhg - you hyperventilate for a while, then you don't have the urge to breathe. In anesthesized folks, that whole curve is shifted to the right - they might have a paco2 of 50 and still not breathe.
|
|
|
What is FRC?
|
Volume at end of normal exhalation. Increased in obesity (less compliance).
|
|
|
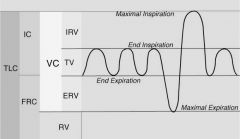
Picture of lung capacities.
|
Add one.
|
|
|
What is closing capacity?
|
VOLUME at which small airways close.
|
|
|
Relationship between FRC and closing capacity?
|
NormallyFRC>>closing capacity. Around age 66, closing capacity >frc so airways close with each exhalation.
|
|
|
What is vital capacity?
|
Max volume of gas that can be exhaled following max. inspiration.
|
|
|
Picture of lung volumes/capacities.
|
|
|
|
Equation relating resistance to length, radius, viscocity.
|
R=(8 *Length *Visc) / (R^4*pi)
So least resistance in short, fat tube with thin stuff Most resistance in long, skinny tube with thick stuff. |
|
|
In Lung Zone 1, how are PA, Pa, and Pv related?
|
PA > Pa > Pv
Alveoli squishing vessels This is like a shunt (ventilated, but not perfused) |
|
|
In Lung Zone 2, how are PA, Pa, and Pv related?
|
Pa>PA>Pv
Good balance |
|
|
In Lung Zone 3, how are PA, Pa, and Pv related?
|
Pa > Pv > PA
This is dead space - blood doesn't actually flow past alveoli |
|
|
Picture of lung zones
|
add one
|
|
|
Examples of obstructive lung dz
|
Asthma, emphysema, chronic bronch, CF
(all have increased resistance to airflow). So Peak pressure would be high, but plateau normal |
|
|
Exampels of restrictive dz
|
ARDS, PNA, fibrosis, sarcoidosis
More like decreased compliance - peak and plateau pressures would be high. |
|
|
Why is o2 therapy bad in co2 retainers?
|
Because they rely on hypoxic drive.
|
|
|
Pulsus Paradoxus - what is it?
|
Normally, pulse gets weaker and BP drops about 10 mm Hg with inspiration. Increased neg. intrathoracic pressure increases venous return, but blood pools in pulm. vasculature, so decreased bp (around 10 mm Hg) and increased hr as a reflex.
This is worse in tamponade, pericarditis, chronic sleep apnea, COPD, asthma. |
|
|
Does pulse increase or decrease during inspiration (in normal pt).
|
It increases. Increased neg. intrathoracic pressure increases venous return, but blood pools in pulm. vasculature, so decreased bp (around 10 mm Hg) and increased hr as a reflex.
|

