![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
|
What amount of the population is affected by asthma?
|
5%
|
|
|
How has the prevalence, hospitalizations, and fatal asthma attacks changed over the past 20 years?
|
All have increased
|
|
|
How does the treatment of asthma and COPD compare?
|
Asthma treatment involves many of the same agents used in COPD
|
|
|
What are the categories of treatments for asthma?
|
- Bronchodilators
- Respiratory Anti-Inflammatory Agents |
|
|
What are the types of bronchodilators for asthma?
|
- β2 agonists: albuterol and salmeterol
- Phosphodiesterase inhibitors: theophylline - Anticholinergics: ipratropium bromide |
|
|
What are the types of respiratory anti-inflammatory agents for asthma?
|
- Mast cell inhibitors: cromolyn sodium and omalizumab
- Glucocorticosteroids: beclomethasone - Leukotriene modifiers: zafirlukast and zileuton |
|
|
What is asthma?
|
Bronchoconstriction d/t hyperresponsiveness of airways to physical, chemical, and/or pharmacological stimuli
|
|
|
What are the symptoms of asthma?
|
- Wheezing
- Cough - Shortness of breath - Tightness in chest |
|
|
What can cause asthma?
|
- Allergy
- Cold air - Exercise - Stress - Respiratory infection |
|
|
What is the pathology in asthma?
|
- Decreased airway caliber
- Bronchiolar edema - Increased airway smooth muscle contractility - Increased bronchial mucosal secretion - Airway epithelial damage - Increased resistance to airflow: limited expiratory rates on forced expiration * Airway inflammation |
|
|
What happens to FEV1/FVC/ratio in asthma?
|
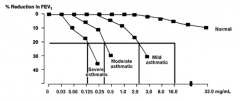
- Reduced FEV1/FVC ratio and reduced FEV1
- The more severe the asthma, the greater the reduction in FEV1 |
|
|
What do you classify asthma based on?
|
- Severity: intensity of disease
- Control: degree to which therapy goals are met |
|
|
What determines the initial treatment for asthma?
|
Severity / intensity of disease
|
|
|
How do you assess the control of asthma treatment?
|
- Ability to maintain level of activity
- Lung function - Prevention of exacerbations |
|
|
What controls airway smooth muscle tone?
|
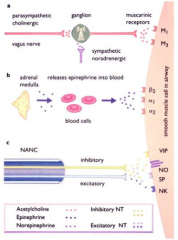
- PNS: action of ACh released from vagus on muscarinic receptors → contraction
- SNS: action of Epi released from adrenal medulla on smooth muscle adrenoreceptors (β2) → relaxation |
|
|
What causes airway inflammation and hyperconstriction response in asthma?
|
- Mast cell degranulation
- Mediator release from various other inflammatory cells (eosinophils) - Bronchoconstriction - Inflammation → hyperconstrictor response of airway smooth muscle to repeated exposure to allergen or other stimuli |
|
|
What antibody is involved in the response to antigen in asthma? Implications?
|
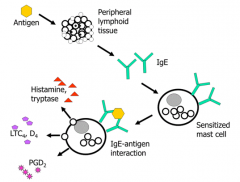
IgE - stimulates mast cells to release histamine, tryptase, LTC4, LTD4, and PGD2 when Ag binds
|
|
|
What happens when mast cells are activated by IgE binding to antigen in asthma?
|
- Degranulation within minutes: histamine, leukotrienes, cytokines, proteases
- Secretion within hours: cytokines and chemokines |
|
|
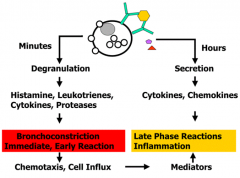
What is the impact of mast cell degranulation in asthma?
|
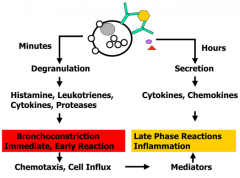
- Histamines, leukotrienes, cytokines, proteases
- Leads to bronchoconstriction (immediate, early reaction) - Causes chemotaxis and cell influx → mediators that also contribute to late phase inflammation reaction |
|
|
What is the impact of mast cell secretion in asthma?
|
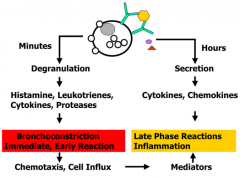
- Cytokines and chemokines
- Leads to inflammation (late phase reaction) |
|
|
What are the consequences of mast cell activation?
|
- Bronchoconstriction
- Chronic inflammation - Mucus secretion |
|
|
What are the components of inflammation after mast cell activation?
|
- Leukocyte and eosinophil infiltration
- Proliferation / activation of inflammatory cells - Increased vascular permeability - Nerve stimulation (e.g., cough) |
|
|
How does the peak expiratory flow rate change during an asthma attack?
|
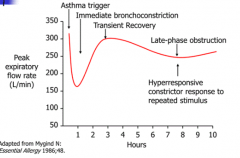
- Immediate bronchoconstriction: causes severe drop in FEV1
- Transient recovery - Late phase obstruction d/t inflammatory response / hyper-responsiveness to repeated stimulus |
|
|
What is the effect of bronchodilators on asthma?
|
Treat the primary symptom of asthma: bronchoconstriction
|
|
|
What is the effect of anti-inflammatory agents on asthma?
|
Reduce airway inflammation that causes smooth muscle hyper-responsiveness to stimuli (treats underlying pathophysiology of disease)
|
|
|
What asthma drug acts by stabilizing mast cells?
|
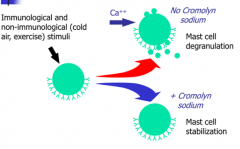
Cromolyn Sodium
|
|
|
What is the mechanism of Cromolyn Sodium?
|
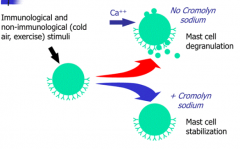
- Prevents bronchoconstriction and inflammation d/t mast cell activation
- Prevents transmembrane influx of Ca2+ into mast cells required for degranulation - May bind to a plasma membrane Ca2+ channel, inhibiting its activity |
|
|
What is necessary for Cromolyn Sodium to be effective?
|
- Must be used immediately before exposure to a known stimulant of asthma attack (eg, cold air, exercise, allergen, etc)
- Treatment is restricted to patients w/ known asthma and fore-knowledge of exposure |
|
|
What is the mechanism of Omalizumab?
|

- Monospecific anti-IgE antibody
- Neutralizes IgE, which prevents it from binding to mast cells - prevents mast cell degranulation |
|
|
What are the β2-adrenoreceptor agonists? Main difference?
|
- Albuterol: short-acting
- Salmeterol: long-acting |
|
|
What are the most widely prescribed and effective agents for treating bronchoconstriction?
|
β2-adrenoreceptor agonists:
- Albuterol (short acting) - Salmeterol (long acting) |
|
|
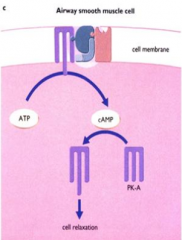
What is the action of Albuterol and Salmeterol?
|
- Bind β2-adrenoreceptors → activates G protein coupled AC → ↑cAMP →
- Increases conductance of large Ca2+ sensitive K+ channels → - Relaxes airway smooth muscle - Stimulates mucociliary transport |
|
|
How quickly does Albuterol work? For how long?
|
Works in 1-5 minutes, lasts 4-6 hours
|
|
|
How do albuterol and salmeterol affect FEV1 in asthma?
|
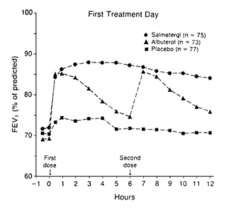
- Both have quick increase in FEV1
- Effect of Albuterol declines after a couple of hours - Effect of Salmeterol is maintained for longer period |
|
|
What kind of toxicity is associated w/ the β-agonists, albuterol and salmeterol?
|
- Direct cardiac toxicity (arrhythmias)
- HTN can't be treated w/ β-antagonists - Overreliance on these drugs may delay seeking adequate medical care |
|
|
What rules should be followed for use of long-acting β-agonists (Salmeterol)?
|
- Don't use as sole initial treatment
- Do not stop using abruptly - Do not use to treat wheezing that is getting worse - Do not try to use to relieve sudden wheezing (always use a short acting bronchodilator) |
|
|
What asthma drug is an anti-cholinergic?
|
Ipratropium Bromide
|
|
|
What is the action of Ipratropium Bromide?
|
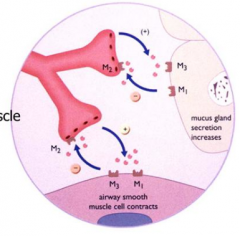
- Anti-cholinergic
- Relaxes airway smooth muscle - Decreases mucus secretion |
|
|
How do anti-cholinergics (ipratropium bromide) compare to β2-agonists?
|
They are not as effective in many patients
|
|
|
Which asthma drug inhibits phosphodiesterase?
|
Theophylline
|
|
|
What is the mechanism of Theophylline?
|
- Prolonges cAMP action
- Acts as a competitive inhibitor at adenosine receptor - Promotes relaxation of airway smooth muscle - Anti-inflammatory effects |
|
|
Why is Theophylline not used as much?
|
- Narrow therapeutic window
- CNS stimulant |
|
|
What is Theophylline used for?
|
Wean or limit oral steroids in asthma treatment
|
|
|
What glucocorticosteroid is used for asthma?
|
Beclomethasone
|
|
|
What is the most effective and most often prescribed anti-inflammatory drug for treating chronic inflammation underlying asthma?
|
Beclomethasone - Glucocorticosteroid
|
|
|
What drug is often used as the first drug in newly diagnosed asthma?
|
Beclomethasone - Glucocorticosteroid
|
|
|
What is the mechanism of Beclomethasone?
|
- Chronic use of inhaled steroid reduces airway smooth muscle hyper-reactivity caused by inflammation
- Decreases transcription of inflammatory mediators (cytokines, prostaglandins, etc) - Increases β2 receptor protein, Lipocortin 1 (aka Annexin - inhibits activity of phospholipase A2) |
|
|
How does Beclomethasone interact with Salmeterol?
|
- Permissive effect of Beclomethasone on response to β-agonists
- Salmeterol also has a permissive effect on steroids |
|
|
What is an example of a Phosphodiesterase-4 Inhibitor?
|
Roflumilast
|
|
|
What is the action of Roflumilast? Use?
|
- Phosphodiesterase-4 Inhibitor
- Controversial in asthma - Used more predominantly in COPD |
|
|
What side effects are caused by Roflumilast? How can you avoid these side effects?
|
- Nausea, headache, abdominal pain
- Avoid by using more specific inhibitor of enzyme subtype: PDE-4β |
|
|
What do you need to consider when using a steroid for asthma?
|
- Inhaled steroids are NOT effective in an acute attack
- Must be used over an extended period - May exert certain effects as soon as 4 hours after treatment |
|
|
What drugs can be used for acute attacks?
|
Cromolyn Sodium and Bronchodilators
|
|
|
What are the potential adverse effects of inhaled glucocorticosteroids (Beclomethasone)?
|
- HPA axis suppression
- Bone resorption - Carbohydrate and lipid metabolism - Skin thinning - Dysphonia - Candidiasis |
|
|
What drugs can modify leukotrienes? How?
|
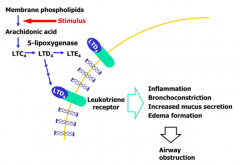
- Zafirlukast: leukotriene receptor antagonist
- Zileuton: 5-lipoxygenase inhibitor |
|
|
What is the mechanism of Zafirlukast?
|
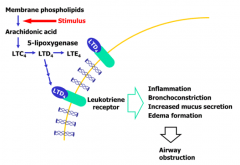
- Leukotriene receptor antagonist
- Blocks bronchoconstriction and inflammation caused by leukotrienes |
|
|
What is the mechanism of Zileuton?
|
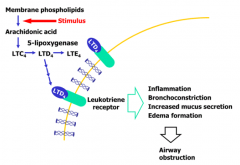
- 5-lipoxygenase inhibitor
- Blocks bronchoconstriction and inflammation caused by leukotrienes |
|
|
When are leukotriene modifiers useful?
|
- Not effective in all asthmatics
- Particularly effective in aspirin induced asthma |
|
|
What kind of toxicity is associated with leukotriene modifiers?
|
Liver toxicity in some patients
|
|
|
How does Zafirlukast affect β2-agonists?
|
Can have synergistic effect, which means the patient requires less β2-agonist because they are on a long-term control drug
|
|
|
What drug interactions occur with leukotriene modifiers?
|
- Zafirlukast and Zileuton interact w/ warfarin and increase prothrombin times
- Zileuton decreases steady state theophylline clearance |
|
|
What kind of treatment should be used for mild, intermittent asthma?
|
- No daily meds
- Short acting β-agonist as needed |
|
|
What kind of treatment should be used for mild, persistent asthma?
|
- Inhaled steroid / long-acting β-agonist combination
- Leukotriene modifiers - Short-acting β-agonist as needed |
|
|
What kind of treatment should be used for exercise-induced asthma?
|
- Inhaled steroid
- Short acting β-agonist as needed - Cromolyn sodium can be used before exercise if effective |
|
|
What are the benefits of an inhaled steroid / long acting β-agonist combination?
|
- Eliminates need for short-acting β-agonist rescue med
- Adjust anti-inflammatory therapy at times of greatest need while obtaining symptom relief - Improved symptoms and reduced severe exacerbation rate - Prolonged time to exacerbation requiring medical intervention |
|
|
How should an emergency asthma attack be treated?
|
Treated in ED:
- Initially w/ supplementary O2 to achieve SaO2 > 90% - Inhaled short-acting β2-agonist - Systemic corticosteroid |
|
|
What amount of the metered dose inhaler dose is inhaled / swallowed?
|
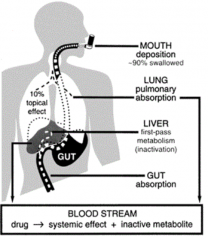
- 90% swallowed
- 10% inhaled into lungs |
|
|
How can you overcome the 90% swallow rate of the drug via inhaler?
|
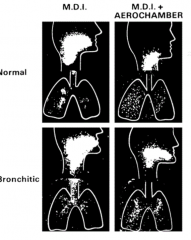
Use aerochamber to get more of the drug into the lungs
|
|
|
What happens in a metered dose inhaler?
|
- Contains propellant in addition to therapeutic agent
- Propellant provides force to generate the aerosol - Propellants (hydrofluroalkanes - HFA) can be >99% of delivered dose |
|
|
What causes COPD?
|
Airflow obstruction d/t chronic bronchitis or emphysema
|
|
|
What are the characteristics of the obstruction in COPD?
|
- Progressive
- Accompanied by airway hyper-reactivity - Generally irreversible |
|
|
How do you diagnose COPD?
|
- History of cigarette smoking
- Chronic cough, dyspnea (in emphysema), and sputum production (in chronic bronchitis) - Airflow obstruction (FEV1/FVC < 0.7) w/ progressively lower FEV1 to classify severity |
|
|
What is the best "treatment" for COPD?
|
- Best intervention: smoking cessation
- Supplemental O2 - Both increase survival (Other pharmacologic agents only treat symptoms) |
|
|
What are the types of drugs used to treat COPD?
|
- Bronchodilators
- Anti-Inflammatory Agents - Antibiotics |
|
|
What Bronchodilators are used for COPD?
|
- β2 agonists: albuterol and salmeterol
- PDE-4 Inhibitor: Roflumilast - Anticholinergics: Ipratropium Bromide and Tiotropium |
|
|
What Antibiotics are used for COPD?
|
Azithromycin
|
|
|
What Anti-inflammatory agents are used for COPD?
|
Glucocorticosteroids
|
|
|
What are the agents of choice in treatment of COPD?
|
Bronchodilators
|
|
|
How do bronchodilators affect patients w/ COPD?
|
- Do NOT alter inexorable decline in lung function
- Improve symptoms and exercise tolerance |
|
|
How do antibiotics affect patients w/ COPD?
|
Prevent and treat acute exacerbations of bronchitis (excessive cough and sputum secretions) that may be accompanied by bacterial infections
|
|
|
What are the treatment recommendations for COPD?
|
- Long-acting inhaled β2-agonists and anticholinergics
- Combined use of long and short acting β2-agonists if needed - PDE4 inhibitor (Roflumilast) for severe or recurrent exacerbations (for those that have failed other therapies) |
|
|
Should short term oral steroids or long term monotherapy steroids be used in COPD?
|
- They can be, but should not be used as sole treatment
- Additionally, long term monotherapy steroids are associated w/ increased risk of pneumonia and fractures |
|
|
What kind of disease is Cystic Fibrosis?
|
- Autosomal recessive disorder
- Mutations in CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) alter Cl- channel |
|
|
How does Cystic Fibrosis affect the lungs?
|
Produce abnormal mucus which depresses lung function
|
|
|
How should Cystic Fibrosis be treated?
|
- Inhaled bronchodilators (see asthma drugs)
- Antibiotics to treat and prevent bacterial infections (azithromycin) - Recombinant Human Deoxyribonuclease (rhDNAase) |
|
|
What is the function of Recombinant Human Deoxyribonuclease (rhDNAase)?
|
Treatment in Cystic Fibrosis:
- Degrades DNA released by infiltrating neutrophils which has a high viscosity (↓ viscosity) - Improves airway clearance of secretions - Decreases frequency and severity of respiratory infections |

