![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
what percentage of cardiac output goes to the kidneys? |
20% - therefore susceptible to blood borne toxins and to ischaemia due to hypotension/hypoxia |
|
|
what components are filtered into the glomerular filtrate? |
urea, water and sodium |
|
|
what hormone does the kidney release? |
erthropoietin |
|
|
what is erthropoetin responsible for? |
stimulation of the bone marrow to produce red blood cells - therefore damage can affect RBC levels |
|
|
urine travels from the kidney to the bladder via the.... |
Ureters |
|
|
urine is voided from the bladder via the... |
urethra |
|
|
diagnostics for renal/urinary disorders |
Bloods – Urea, Creatinine, Phosphorus, Potassium andother electrolytesUrinalysis– methods of collection (free catch, bladder expression, katkor, catherisation, cystocentesis – pros/cons?) |
|
|
define Azotamia |
a rise in urea and creatinine in the blood. further classified as pre-renal(before kidney - dehydration), renal (kidney damage) or post-renal (afterkidney – bladder obstruction) |
|
|
a cause of Pre-renal azotaemia is... |
dehydration |
|
|
a cause of post renal azotaemia is... |
bladder obstructions |
|
|
ingestion of lilies is a cause of... |
renal azotaemia |
|
|
what is the most reliable urine collection method for culture? |
cystocentesis |
|
|
is finding haematuria normal in urine samples? |
no |
|
|
urine SG of 1.003 indicates? |
very dilute urine (weak urine) |
|
|
kidney is better visualised on an x-ray or ultrasound? |
ultrasound |
|
|
upper urinary tract disorders can be caused by |
-circulatory problems |
|
|
ARF? |
Acute renal failure |
|
|
AKI? |
Acute kidney injury can be reversible if diagnosed and treated quickly –Ischaemia–Toxins–Bacterialinfection (pyelonephritis)–Urinaryobstruction Ishaemia –hypotension/hypovolaemia due to shock, anaesthesia, decreased cardiac output/thrombosisToxins– NSAIDs, Ethylene glycol, lilies |
|
|
ARF signs |
•Suddenonset•Lethargy•Inappetance•Vomitting/Diarrhoea•Dehydration•Oliguria/Anuria(polyuria in later stages)•Enlarged,painful kidneys•Bradycardia(if hyperkaleamic)•Tachycardia(if hypovolaemic)•Pyrexia(pyelonephritis) |
|
|
ARF treatment and nursing |
antibiotics if bacterial involvement IVFT to correct dehydration and for ongoing losses monitor BP In dogs a possible cause is leptospirosis – consider isolationand barrier nursing for AKI which no history of toxin ingestion and poor vacchistory. |
|
|
CRF? |
chronic renal failure |
|
|
CRF |
•Slowonset and progression••Bodyis able to adapt and compensate••Clinicalsigns not apparent until >70% of renal function is lost••Couldbe caused by toxins/ischaemic damage/infections or idiopathic |
|
|
CRF signs |
Pu/pd – kidneys no longer able to concentrateurine and Pd inresponse to excessive urinationUlcers – nitrogenous waste products inblood lead to ulceration causing nausea and anorexiaWeight loss – poor appetite, musclewastage and protein loss from kidneys
Rubber jaw (not common) or secondaryrenal hyperparathyroidism (high phosphate levels from reduced excretion resultin the body producing extra parathyroid hormone and this in turn withdrawscalcium from bones, leading to soft and rubbery bones (especially of the jaw). |
|
|
CRF diagnosis |
•Increasedblood urea, creatinine and phosphorus• Anaemia(non-regenerative)••Mayhave hypokalaemia• Urinalysis–Lowurine SG–Mayhave proteinuria–Sendfor culture to check for infection Anaemia – erythopoeitin production is affectedHypokalaemia – due to PU, can cause neuromuscularsigns, ventroflexion of neck |
|
|
CRF treatment and nursing |
Encourage fluid intake – water fountains,flavoured water
Renal diet – Phosphate restriction (prevent 2ndaryhyperparathyroidism which can be fatal), protein restriction and highbiological value (reduce waste for kidneys to deal with), potassium and vit Bsupplemented as excess loss with PU, palatable and calorie dense (encourageweight gain as most CRF cats are underweight), reduced sodium (to minimisehypertension) Medication likely euthanasia |
|
|
Nephrotic syndrome (NS) |
presence of proteinuria, hypoalbuminemia, hyperlipidaemic and interstitial fluid accumulation. •Dueto damage to glomerulus (glomerulonephropathy) •Proteinleaks into urine and leads to fluid moving out of the vasculature.• Compensatorymechanisms worsen condition |
|
|
NS signs |
•Oedema•Ascites•Lethargy•Weightloss•PD/PU•Proteinuria•Hypoalbuminaemia•Hypernatraemia andhypertension (compensatory mechanisms) |
|
|
NS treatment |
Treatment – underlying cause ?corticosteroids/anabolic steroids/antibiotics – to treat underlying cause ofnephropathy. |
|
|
Polycystic Kidney Disease (PKD) |
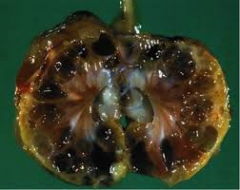
•diseasewhich causes large fluid-filled cysts to form within the kidney. •Congenitalabnormality (Persians) •Screeningprogramme for owners and breeders (ultrasound/DNA test) |
|
|
Ownerscomment during a nursing consult that their elderly cat has lost a lot ofweight, is drinking more and is having accidents in the house. This could be asign of acute or chronic RF? |
chronic |
|
|
Adog presents with sudden onset of lethargy, inappetence and reduced urination which is mostlikely? acute or chronic? |
acute |
|
|
hypoxia during anaesthesia could put a patient at risk of ... |
ARF |
|
|
hyperkalaemia is a sign of ... |
ARF |
|
|
patient with palpably enlarged kidneys is more likely to have... |
ARF |
|
|
complete recovery is possible in ... |
ARF |
|
|
Lower urinary tract disorders involve the ... |
bladder and urethra |
|
|
what are lower urinary tract disorders caused by... |
–Bacterialinfections–Urinarystones–Anatomicaldefects–Neurologicaldeficits–Stress |
|
|
cystitis is the.... |
inflammation of the lining of the bladder - caused by ascending bacteria –Traumacaused by uroliths(stones)–Retentionof urine–Concurrentillness e.g. diabetes mellitus–Indwellingurinary catheter |
|
|
clinical signs of lower UTI |
Dysuria – difficulty passing urine |
|
|
lower UTI diagnosis |
•Cultureand sensitivity prior to antibiotic treatment - sample collected via cystocentesis••Inpractice for first occurrence, simple cases this may not be undertaken ,however essential for recurrent cases |
|
|
lower UTI treatment |
antibiotics, encourage urination, encourage fluid intake, prevent urine scalding |
|
|
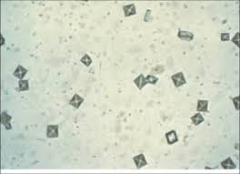
Urolithiasis(urinary stones/calculi) is the... |
•Formationof stones within the urinary tract••Causedby a combination of factors that allow for the precipitation of solutes and thegrowth of crystals••Factorsinclude:–Saturationof the urine–pHof urine–Presenceof UTIs–Breed–Diet |
|

|
struvite (alkaline pH) |
|
|
calcium oxalate (acidic pH) |
|

|
urate (found in Dalmatians) |
|
|
Lower UTI diagnosis |
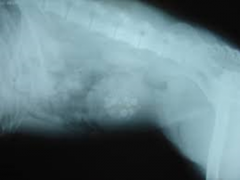
•Radiography/ultrasound - Contrast study•Urinalysisand pH measurement•Completediagnosis should include stone analysis where appropriate |
|
|
lower UTI treatment |
Short term•Surgicalremoval of stone•Dietto dissolve (struvite)•Antibioticsto treat any UTI•Nursingcare and monitoring post op Long term•Dietto prevent reoccurrence•Encouragewater intake•Regularurinalysis/urine sediment exam to monitor Diets – promote solubility and volume ofurine, wet diet is better for increases water intake. Alter pH and dietary components. Aim for pH6.7-7 to prevent both struvite and calcium oxalate |
|
|
FLUTD |
Feline Lower Urinary Tract Disease |
|
|
Feline lower urinary tract disease |
involve bacterial infection or uroliths feline idiopathic cystitis (FIC) Stress– environmental factors including multicat households where there is conflictpresent may reduce water intake and urine elimination. |
|
|
FLUTD signs |
•Clinicalsigns are cystitis like signs – haematuria, dysuria, pollakiuria••Mayhave obstruction (blocked bladder) which could result in renal failure orbladder rupture–Clinicalsigns in these cases are urinary tenesmus and vocalisation–Anuria–Large,painful bladder•EMERGENCYCASES! - A cat showing signs of obstruction should be seen immediately |
|
|
'blocked cat' treatment |
•Assessmentof cardiovascular system (hyperkalaemia caused by blockage can have markedaffect on CV system)•Relieveobstruction (retrograde hydropulsion)•Catheterisebladder and flush urethra and bladder to remove any crystals/debris If hyperkalaemia is symptomatic then stabilisation(fluids/meds) is required prior to any sedation/GAIf can not relieve obstruction (or need to stabilise first)bladder size may be reduced in the short termvia cystocentesis (carries risk of rupture) while nextstep is considered such as urethrostomy/cytostomy tube. |
|
|
FLUTD long term management |
•Diet(wet diet/specific prescription diet)•Increasewater intake•Considerhome environment –availabilityof resources–environmentalenrichment–pheromonetherapy•Medications•Monitorfor signs of relapse/blockage |
|
|
what is non neurogenic incontinence? |
associatedwith anatomical/functional disorders of the urinary tract - ectopic ureter, urethal sphincter mechanism incompetence (USMI) |
|
|
what is neurogenic incontinence? |
involvessacral spinal cord and likely to be combined with other neurological signs - spinal cord injury/disease |
|
|
incontinence signs |
•‘Wetpatch’ on bed•Urinationwhilst walking•Urinescalding |
|
|
incontinence treatment |
•Preventscalding with barrier creams•Frequentopportunity to urinate•Surgeryfor anatomical defectsMedicationfor USMI |
|
|
urine retention |
•Possibleafter spinal injury/RTA (neurogenic)•Mayshow signs of incontinence (over-flow)•Unproductivestraining (dysuria/stranguria)Treatment- medications to relax/contract muscles - Timing of medications is important toensure co-ordinated contraction and relaxation |
|
|
dysuria means... |
difficulty urinating |
|
|
Pollakiuria means... |
protein in the urine |
|
|
stone to form in alkaline urine is... |
struvite |

