![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
122 Cards in this Set
- Front
- Back
|
"Dirtier" blood travels in through the (a) ____________________ and "Cleaner" blood travels out through the (b) _______________________. The waste leaves through the (c) _____________________ from the kidneys in the (d) _____________________. |
(a) Renal Artery (b) Renal Vein (c) Ureter (d) Urine |
|
|
Kidneys are (a) _____% of our body weight. Kidneys also take (b) _____% in O2 consumption. The cardiac output of the kidneys is (c) _____-_____%. |
(a) 0.5 (b) 6 (c) 20-25 |
|
|
What does the structure of the Nephron consist of? |
Bowman's capsule and Glomerulus |
|
|
___________________ is a network of porous capillaries having large pores in endothelial cells and large gaps between endothelial cells. |
Glomerulus |
|
|
_______________________________ is the beginning of the renal tubular system, consisting of epithelial cells with foot-like processes (podocytes) separated by large gaps. |
Bowman's capsule |
|
|
_____________________________ in the glomerular capillaries drives rapid filtration of protein-free fluid from glomerular capillary into the Bowman's capsule. |
Blood pressure |
|
|
A juxtamedullary nephron has a long loop of Henle that extends into the (a) ______________________, whereas a cortical nephron has a short loop of Henle that is situated mostly in the (b) ________________________. |
(a) renal medulla (b) renal cortex |
|
|
The primary function of the loop of Henle is: |
production of an osmotic gradient in the renal interstitium from approximately 300 mOsM in the renal cortex to approximately 1,200 mOsM in the renal medulla. |
|
|
Known as the major diluting segment of the nephron because they are capable of lowering tubular fluid osmolarity to lower than 100 mOsM by reabsorbing Na+ from the tubular fluid to peritubular capillaries. |
Distal convoluted tubule |
|
|
The last segment of the nephron; it is important for producing concentrated urine during dehydration by allowing fluid in the collecting duct to equilibrate with the high osmolarity in renal medulla. |
Medullary collecting duct |
|
|
Name the two capillary networks and their functions. |
Glomerular Capillary for Glomerular Filtration. Peritubular Capillary for Reabsorption and Secretion. |
|
|
Name the three fundamental processes in a Nephron. |
Glomerular filtration, tubular reabsorption, and tubular secretion. |
|
|
What is the equation for Net Hydrostatic Pressure for Glomerular Filtration? |
Net Hydrostatic Pressure for Glomerular Filtration = PGC - PBC PGC = Glomerular capillary blood pressure PBC = Bowman's capsule fluid pressure |
|
|
What is the equation for Net Protein Osmotic Pressure Against Glomerular Filtration? |
Net Protein Osmotic Pressure Against Glomerular Filtration = πGC - πBC πGC = Protein osmotic pressure in glomerular capillary blood πBC = Bowman's capsule fluid |
|
|
What is/What is the equation for Glomerular filtration pressure? |
Glomerular filtration pressure = PGC - PBC - πGC + πBC PGC = Glomerular capillary blood pressure PBC = Bowman's capsule fluid pressure πGC = Protein osmotic pressure in glomerular capillary blood πBC = Bowman's capsule fluid |
|
|
What are glomerular capillary blood pressure and glomerular filtration rate dependent on and why? |
Glomerular capillary blood pressure and glomerular filtration rate are dependent upon vascular resistances of afferent and efferent arterioles, because glomerular capillary is situated between afferent and efferent arterioles. |
|
|
____________________________ controls the blood pressure drop from the renal artery to the glomerular capillary. |
Afferent arteriole |
|
|
_____________________________ controls the blood pressure drop from the glomerular capillary to the peritubular capillaries. |
Efferent arteriole |
|
|
Afferent arteriolar vasoconstriction (a) __________________ glomerular filtration pressure and glomerular filtration rate. A(n) (b) __________________ in afferent arteriolar resistance (c) ________________ the blood pressure drop from the renal artery to the glomerular capillary. |
(a) decreases (b) increase (c) increase |
|
|
Efferent arteriolar vasoconstriction (a) ____________________ glomerular filtration pressure and glomerular filtration rate, because a(n) (b) __________________ in efferent arteriolar resistance (c) ___________________ the pressure drop from the glomerular capillary to the peritubular capillary. |
(a) increases (b) increase (c) decreases |
|
|
Renal blood flow ____________________ in response to an increase in renal vascular resistance, regardless of the vessel of vasoconstriction. |
decreases |
|
|
______________________________ is the process of transporting a molecule by renal tubular cells from glomerular filtrate in the renal tubular system to peritubular capillaries, thereby decreasing the excretion of a molecule. |
Renal reabsorption |
|
|
______________________________ is the process of transporting a molecule by renal tubular cells from peritubular capillaries into the renal tubular system, thereby increasing the excretion of a molecule. |
Renal secretion |
|
|
What is the equation for excretion? |
Excretion = Filtration - Reabsorption + Secretion |
|
|
The ___________________ Tubule is isoosmotic reabsorption and has high H2O permeability. |
Proximal |
|
|
The (a) _______________________ Limb of Henle and (b) ____________________ Tubule is used for diluting segments of the nephron and uses Na+-pumping activity. |
(a) Ascending (b) Distal |
|
|
It is a major site of renal reabsorption and more than 60% of glomerular filtrate is reabsorbed by it. |
Proximal convolute tubule |
|
|
Transporters on the luminal side of proximal tubular cells are _________________________________________________ for driving reabsorption of molecules against their concentration gradient. |
Na+-coupled transporters |
|
|
Renal tubular reabsorption of (a) ___________________ and (b) ___________________ by distinct transporters occurs in the luminal and basolateral membranes of a proximal tubular cell. |
(a) Phosphate (b) Glucose |
|
|
__________________________________________ is an important criterion for classification of kidney disease. |
Glomerular filtration rate |
|
|
When GFR * [Glucose]plasma < Tmax, glucose is __________________________________ and [Glucose]urine = 0. |
completely reabsorbed |
|
|
When GFR * [Glucose]plasma = Tmax and [Glucose]plasma = Renal threshold, glucose is __________________________________________. [Glucose]urine = 0 |
completely reabsorbed |
|
|
Renal threshold for complete glucose reabsorption is about _______ mM. |
11 |
|
|
When GFR * [Glucose]plasma > Tmax, glucose is __________________________________ and [Glucose]urine > 0. |
not completely reabsorbed |
|
|
What is the equation for urinary glucose excretion? |
Urinary Glucose Excretion = GFR * [Glucose]plasma - Tmax |
|
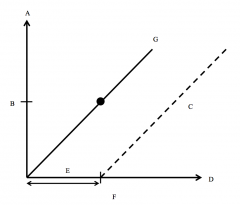
Label this graph of Renal Handling of Glucose. |
A. Rate of Glucose Filtration or Glucose Excretion B. Transport Maximum (Tmax) C. Glucose Excretion = GFR * [Glucose]plasma - Tmax D. [Glucose]plasma E. Complete Glucose Reabsorption F. Renal Threshold G. Glucose Filtration = GFR * [Glucose]plasma |
|
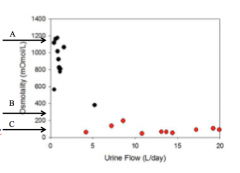
Label the arrows in this graph of Regulation of Extracellular Fluid Osmolarity by Regulating Urine Osmolarity. |
A. Concentrated Urine Osmolarity B. Plasma Osmolarity (280 mOsM) C. Dilute Urine Osmolarity |
|
|
___________________ increases water permeability of collecting duct to enhance the diffusion of water from collecting duct to the renal interstitium. |
ADH |
|
|
Fluid reabsorption by the proximal tubule is known as ___________________________________. |
Isoosmotic reabsorption |
|
|
What is a major function of the loop of Henle? |
A major function of the loop of Henle is the generation of an osmotic gradient in the renal interstitium by countercurrent multiplication. |
|
|
What does "countercurrent" refer to? |
"Countercurrent" refers to the opposite direction of fluid flow in the descending and ascending limbs of the loop of Henel. |
|
|
What does "multiplication" refer to? |
"Multiplication" refers to amplification of the Na+ pumping effect of each segment of the loop to generate a large overall osmotic gradient in the renal interstitium. |
|
|
The overall osmotic gradient in the renal interstitium ranges from (a) ______ mOsM in the renal cortex to (b) _______ mOsM in the renal medulla. |
(a) 300 (b) 1,200 |
|
(a)______________________ in the hypothalamus detect the increase in the plasma osmolarity and in response stimulate the release of (b) __________ from posterior pituitary. |
(a) Osmoreceptors (b) ADH/VP |
|
An increase in plasma concentration of ADH/VP causes the (a) ___________________ in renal water reabsorption and (b) ___________________ in urine osmolarity. |
(a) increase (b) increase |
|
|
__________ increases water reabsorption by increasing water permeability of collecting duct for the production of concentrated urine. |
ADH |
|
|
ADH increases water permeability of cells of (a) _____________________________________ and (b) _____________________________________ by inserting (c) __________________ channels onto the cell membrane. |
(a) collecting tubule (b) collecting duct (c) aquaporin |
|
|
In presence of _______________________, water channels (aquaporin channels) insert onto collecting duct membrane and permit osmotic equilibrium between collecting duct fluid and medullary interstitial fluid, thereby producing concentrated urine. |
vasopressin |
|
|
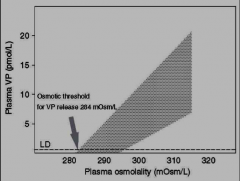
Draw the effect of antidiuretic hormone (vasopressin, VP) on urine osmolarity. |
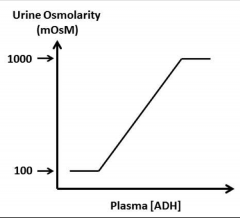
|
|
|
__________________________________ can be caused by genetic deficiencies in vasopressin receptor and aquaporin. |
Diabetes insipidus |
|
|
In absence of (a) ____________________________, water channels (aquaporin channels) are (b) _________________ from collecting duct membrane, causing tubular fluid to remain (c) _________________ as it passes through collecting duct. |
(a) vasopressin (b) removed (c) hypoosmotic |
|
|
Regulation of extracellular fluid volume by renin-angiotensin-aldosterone system causes these three things. |
(a) Sympathetic activity (b) Tubular Na+ & Cl- reabsorption, K+ excretion, H2O retention (c) Aldosterone secretion |
|
|
High ECF Osmolarity --> ______ Plasma ADH/VP --> ______ Renal Reabsorption of Water |
Increases Increases |
|
|
_________________________________________ are sensors of Na+ delivery through distal tubule. In response to low Na+ delivery through the distal tubule, these signal juxtaglomerular cells to release renin. |
Macula densa cells |
|
|
Macula densa signal (a) __________________________ cells to release (b) ________________ when they sense low Na+ delivery through distal tubule. |
(a) juxtaglomerular (b) renin |
|
|
Angiotensin II stimulates ________________________ secretion by adrenal cortex. |
Aldosterone |
|
|
Aldosterone (a) ________________________ Na+ reabsorption in the (b) _______________________ limb of Henle, (c) _____________________ tubule, and (d) ____________________ tubule. |
(a) increases (b) ascending (c) distal (d) collecting |
|
|
Aldosterone increases __________________________________________________ by increasing Na+ reabsorption. |
extracellular fluid volume |
|
|
How is the kidney involved in hypertension? |
From the kidney, angiotensin II-induced vasoconstriction and aldosterone-induced Na+ and water retention causes high blood pressure (hypertension). |
|
|
How is the sympathetic nervous system involved in hypertension? |
The sympathetic nervous system causes sympathetic stimulation of vasoconstriction, which causes high blood pressure (hypertension). |
|
|
What interactions between the sympathetic nervous system and kidney cause hypertension? |
The sympathetic nervous system causes the sympathetic nerves to stimulate renin release by the kidney. The kidney produces angiotensin II, which stimulates activity of the sympathetic nervous system. These result in vasoconstriction and the increase in blood pressure (hypertension). |
|
|
Vitamin D is hydroxylated in the _________________ and ____________________. |
Liver and kidney |
|
|
Vitamin D is _______________________ in the liver and kidney. |
hydroxylated |
|
|
________________________________ and ________________________________ enhance renal Ca2+-reabsorption by stimulating protein expression of Ca2+ transporters in renal tubular epithelial cells. |
Parathyroid hormone and vitamin D |
|
|
Parathyroid hormone and vitamin D enhance (a) __________________________________________________ by stimulating protein expression of (b) _________________________________ in renal tubular epithelial cells. |
(a) renal Ca2+-reabsorption (b) Ca2+ transporters |
|
|
Ca2+ enters the (a) _____________________ side of a tubular cell through (b) _____________________ channels, and leaves the (c) _____________________ side through (d) ____________________________ and (e) ___________________________. |
(a) luminal (b) calcium (c) basolateral (d) Na+/Ca2+ exchange (e) Ca2+-ATPase |
|
|
What is the CO2/bicarbonate buffer system? |
CO2 + H2O <--> H2CO3 <--> H+ + HCO3- |
|
|
What is the equation of the chemical equilibrium of the CO2/bicarbonate buffer system? |
K = [H+] * [HCO3-] / [H2CO3] |
|
|
What is the Henderson-Hasselbalch equation? |
pH = pK + log{[HCO3-]/αPCO2} |
|
|
Extracellular pH is dependent on the ___________________ ratio. |
[HCO3-]/PCO2 |
|
|
What causes an increase and decrease in CO2? |
Increase: (Hypoventilation) Respiratory acidosis Decrease: (Hyperventilation) Respiratory Alkalosis |
|
|
What causes the increase and decrease in HCO3-? |
Increase: (acid production) Metabolic acidosis Decrease: (bicarbonate production) Metabolic alkalosis |
|
|
If there is an increase in CO2, there is a(n) __________________________ in HCO3-. |
decrease |
|
|
If there is a decrease in CO2, there is a(n) __________________________ in HCO3-. |
increase |
|
|
List the three ways the kidneys regulate acid-base. |
1. Tubular reabsorption of HCO3- 2. Tubular secretion of H+ as titratable acid 3. Tubular excretion of NH4+ |
|
|
Bicarbonate is filtered from the plasma into the renal tubular system by glomerular filtration but is completely reabsorbed back to the circulation by _______________________________________. |
renal tubular cells |
|
|
Inside a tubular cell, ____________________________ catalyzes the conversion of CO2 to H2O to H2CO3. |
carbonic anhydrase |
|
|
H2CO3 dissociates into _______ and _______. |
H+ and HCO-. |
|
|
H+ is transported from a tubular cell into tubular lumen by (a) _____________ exchange and (b) __________________ at the luminal membrane for neutralization of (c) ___________ to form (d) ___________. |
(a) Na+/H+ (b) H+-ATPase (c) luminal HCO3- (d) H2CO3 |
|
|
Carbonic anhydrase converts H2CO3 to ___________ and __________. |
CO2 and H2O |
|
|
K+ is reabsorbed in the nephron through (a) ___________ exchange channels and (b) ___________ channels. |
(a) Na+/K+ (b) Na+/Cl-/K+ |
|
|
In the CNT or principal cell of the nephron, K+ is secreted through ___________ channels and ____________. |
K+ K+-ATPase |
|
|
In the intercalated cell (α) in the nephron, K+ is secreted through (a) _________ channels and (b) _____________. (c) ______________ exchange channels and (d) ____________ channels are used in the secretion of K+ as well. |
(a) Na+/K+ (b) K+-ATPase (c) HCO3-/Cl- (d) Cl--ATPase |
|
|
During tubular secretion, H+ is transported actively from a (a) _______________________ into (b) _______________________ by H+-ATPase at the (c) ______________________________ and HCO3- is transported to the circulation via (d) ______________________________ at the (e) ______________________________. |
(a) tubular cell (b) luminal fluid (c) luminal membrane (d) HCO3-/Cl- exchange (e) basolateral membrane |
|
|
During tubular secretion, H+ in tubular fluid is buffered mostly by (a) __________________ resulting in a modest (b) ___________________ in pH. |
(a) phosphate (b) decrease |
|
|
What is a "titratable acid" and why? |
The amount of H+ captured by buffer in the urine is known as "titratable acid," because it can be determined by titrating the pH of urine back to 7.4. |
|
|
During renal excretion of ammonium, renal tubular cells produce __________ and ___________ from glutamine. |
HCO3- and NH4+ |
|
|
During renal excretion of ammonium, renal tubular cells produce HCO3- and NH4+ from _____________________. |
glutamine |
|
|
How is HCO3- transported from a tubular cell to the circulation and where does it occur during renal excretion of ammonium? |
HCO3- is transported from a tubular cell to the circulation via Na+/NH4+ exchange at the luminal membrane. |
|
|
Name the modes of transport in tubular excretion of ammonium. |
Na+/H+ exchange, NH3/NH4+ channels, Na+/HCO3- cotransport |
|
|
What is a measure of the kidney's rate of clearing plasma of a given molecule X by urinary excretion? |
Renal clearance |
|
|
What is renal clearance? |
Renal clearance is a measure of the kidney's rate of clearing plasma of a given molecule X by urinary excretion |
|
|
Quantitatively, renal clearance is the flow of clean plasma cleared of X by what equation? |
Clearance of X = [X]urine * Urine Flow / [X]plasma or Clearance of X = Rate of Urinary Excretion of X / [X]plasma or C = UV/P C = clearance of X U = conc. of X V = urine flow P = plasma conc. of X |
|
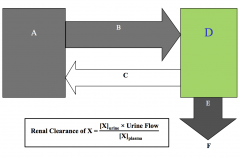
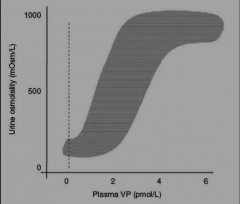
Label this chart. |
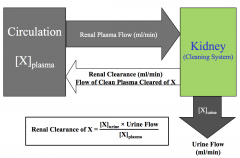
|
|
|
What is the equation for Rate of Creatinine Excretion? |
Rate of Creatinine Excretion = [Creatinine]urine * Urine Flow = [Creatinine]plasma * GFR |
|
|
What is the equation for Clearance of Creatinine? |
Clearance of Creatinine = [Creatinine]plasma * GFR / [Creatinine]plasma = GFR |
|
|
Creatinine is handled by _____________________________________ only. |
Glomerular filtration Clearance of Creatinine = Glomerular Filtration Rate |
|
|
When Clearance = GFR, how is the substance handled by the kidney? |
Filtration only |
|
|
When Clearance < GFR, how is the substance handled by the kidney? |
Filtration + Reabsorption |
|
|
When Clearance > GFR, how is the substance handled by the kidney? |
Filtration + Secretion |
|
|
In clearance values, when maximum clearance is reached, what is it equal to and how is it handled by the kidneys? Give an example. |
Maximum clearance = Renal plasma flow It is handled by the kidneys through Glomerular filtration + complete secretion. An examples is Para-aminohippuric acid (PAH) |
|
|
What is an indicator os kidney failure and why? |
High [Creatinine] in plasma [Creatinine]plasma * GFR = Rate of Creatinine Excretion [Creatinine]plasma = Rate of Creatinine Excretion/GFR At constant rate of creatinine excretion, Inc. [Creatinine]plasma reflects Dec. GFR |
|
|
Detrusor muscle of bladder wall (smooth muscle) is stimulated by the (a) ___________________________________ of the (b) ______________________ Nervous System. |
(a) pelvic nerve (b) parasympathetic |
|
|
The __________________________________________________ (smooth muscle) is stimulated by the hypogastric nerve of the sympathetic nervous system. |
Internal Urethral Sphincter |
|
|
The __________________________________________________ (skeletal muscle) is stimulated by pudendal nerve of the somatic nervous system. |
External urethral sphincter |
|
|
The micturition center in the brain stem regulates (a) _________________________ and (b) _____________________________ of the lower urinary tract by regulating (c) ___________________________, (d) __________________________, and (e) ____________________________ in response to mechanosensory input from the urinary bladder wall. |
(a) urine storage (continence) (b) urination (micturition) (c) parasympathetic (d) sympathetic (e) somatic output |
|
|
During the continence phase, when the urinary bladder is (a) ______________________ filled, mechanosensory input to the micturition center is (b) ________________________, because mechanical stretch of the urinary bladder wall is (c) _________________________. |
(a) not fully (b) low (c) low |
|
|
During the continence phase, the micturition center (a) ______________________ parasympathetic output and (b) _____________________ sympathetic and somatic outputs to the lower urinary tract. |
(a) inhibits (b) stimulates |
|
|
During the continence phase, the inhibition of parasympathetic output to the detrusor smooth muscle cells causes __________________________ of the bladder wall for accommodating continued filling of the urinary bladder with urine. |
relaxation
|
|
|
The stimulation of sympathetic output to smooth muscle cells of the internal urethral sphincter and somatic output to skeletal muscle cells of the external urethral sphincter causes (a) ____________________________ of these two sphincters for (b) __________________________________________________ of urine during the continence phase. |
(a) contraction (b) preventing leakage |
|
|
During the micturition phase, when the urinary bladder is (a) ___________________ filled, mechanosensory input to the micturition center is (b) ___________________, because mechanical stretch of the urinary bladder wall is (c) ___________________. |
(a) fully (b) high (c) high |
|
|
During the micturition phase, the micturition center (a) __________________ parasympathetic output and (b) ___________________ sympathetic and somatic outputs to the lower urinary tract. |
(a) inhibits
(b) stimulates |
|
|
During the micturition phase, the stimulation of the parasympathetic output to detrusor smooth muscle cells causes (a) _____________________ of the bladder wall and (b) ____________________ of pressure inside the urinary bladder. |
(a) contraction
(b) buildup/increase |
|
|
The inhibition of sympathetic output to smooth muscle cells of the internal urethral sphincter and somatic output to skeletal muscle cells of the external urethral sphincter causes ____________________________ of these two sphincters for urinary flow during the micturition phase. |
relaxation |
|
|
Diuretics (a) ___________________ plasma volume by (b) ______________________ Na+ reabsorption. |
(a) lower
(b) inhibiting |
|
|
What is chronic kidney failure characterized by? |
Chronic kidney failure is characterized by a diminished glomerular filtration rate, increased urinary excretion of protein, or both.
|
|
|
What does kidney failure lead to? |
Kidney failure leads to the accumulation of waste products and excess volume in the extracellular fluid, which can lead to failures in multiple organs.
|
|
|
What are the dialysis systems used for?
|
Dialysis systems are used for removing waste products from the extracellular fluid in patients having kidney failure.
|
|
|
During hypoxic stress, what happens to the erythropoietin production levels? Where is erythropoietin produced? |
In hypoxic stress, erythropoietin production may increase a 1000-fold, reaching 10,000 mU/ml of blood. Erythropoietin is produced mainly by peritubular capillary lining cells of the renal cortex, which are highly specialized, epithelial-like cells. It is synthesized by renal peritubular cells in adults, with a small amount being produced in the liver. |
|
|
What is the basic principle of dialysis? |
The basic principle of dialysis is a diffusional exchange of waste products between extracellular fluid and dialysate through a membrane system that is selectively permeable to small molecules but impermeable to proteins and cells. |
|
|
What is the difference between peritoneal dialysis and hemodialysis? |
During peritoneal dialysis, clean dialysate is infused into the abdominal cavity via a catheter. Can be performed at home. During hemodialysis, blood is pumped out of the patient's circulation via an artery into a membrane dialyzer for diffusional exchange with dialysate. Cleansed blood leaving the membrane dialyzer is pumped back into the patient's circulation via a vein. Usually performed at a clinical center. |
|
|
How is kidney transplantation performed? |
The donor's kidney's renal artery and renal vein are typically connected to the recipient's artery and vein in the abdominal cavity. The donor's kidney's ureter is typically connected to the recipient's urinary bladder. The recipient's failed kidneys are usually left in place, unless they cause infection or hypertension in the patient. |

