![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
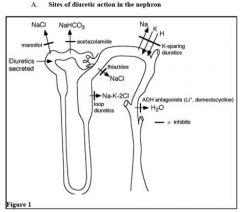
Diuretics increase urine formation. The degree to which solute and water excretion is increased depends on the site and mechanism of action. The strongest diuretics, ____________, act in a segment where a large % of filtered Na+ would be reabsorbed. Conversely, the weakest diuretics, ___________, act in a segment where a small % of filtered sodium is reabsorbed.
|
strongest diuretics: loop diuretics,
weakest diuretics: K-sparing diuretics |
|
|
List the sites of diuretic action in the nephron. (6)
|
|
|
|
Which three are weak acids and are secreted by the organic acid secretory mechansim which is inhibited by probenecid?
A. Acetazolamide B. Amiloride C. Loop diuretics D. Thiazide diuretics E. Triamterene |
A. Acetazolamide
C. Loop diuretics D. Thiazide diuretics are all weak acids, secreted by organic acid secretory mechanism and inhibited by probenecid |
|
|
Acetazolamide, loop diuretics, and thiazide diuretics are all weak acids, secreted by organic acid secretory mechanism and inhibited by _________.
|
Probenecid
|
|
|
_________ does NOT act on the luminal membrane of epitelial cells. Rather, it is a steroid which enters the distal tubule cells and interferes with translocation of aldosterone to the nucleus.
|
Spironolactone
|
|
|
Mannitol
1. What type of diuretic? 2. Where is its site of action? 3. What is its bottom line? 4. What is its clinical usage? 5. What is it NOT used for since it increases blood osmolarity and would expand ECFvolume? |
Mannitol
1. Osmotic diuretic 2. Proximal tubule 3. it is filtered but not reabsorbed; to maintain the principle of isosmotic reabsorption some other solute must be reabsorbed in excess to make up for it - that solute is sodium! As a result, tubular fluid [sodium] decreases, which establishes a sodium gradient from blood to lumen. Then sodium backfluxes into the lumen and water follows. Bottom line - mannitol causes increased excretion of both sodium and water! 4. used to reduce intracranial or intraocular pressure 5. not used for edema |
|
|
Which does this describe:
it is filtered but not reabsorbed; to maintain the principle of isosmotic reabsorption some other solute must be reabsorbed in excess to make up for it - that solute is sodium! As a result, tubular fluid [sodium] decreases, which establishes a sodium gradient from blood to lumen. Then sodium backfluxes into the lumen and water follows. Bottom line - causes increased excretion of both sodium and water! A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
K. Mannitol
|
|
|
Used to reduce intracranial or intraocular pressure. Not used for edema
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
K. Mannitol
*USED TO REDUCE INTRACRANIAL OR INTRAOCULAR PRESSURE (hypertonic solutions of mannitol draw water out of brain cells by osmosis thereby reducing intracranial pressure) * NOT used for edema (b/c increases blood osmolarity which would expand ECF more |
|
|
* inhibits reabsorption of filtered bicarbonate by inhibiting carbonic anhydrase in both the brush border of poximal tubule and in the cells
* b/c the enzyme is essential for reabsorption of filtered bicarb (and accompanying Na), the excretion of BICARB, sodium and water is increased. A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
|
|
|
Used to treat glaucoma and alkalinize the urine.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
also used to treat high altitude sickness * treatment of glaucoma * alkalinization of the urine (to increae solubility of certain substances, like cystine, uric acid and MTX in the urine; to treat drug OD like phenobarbital and salicylate). Note, though you must administer bocarbonate simultaneously to keep up the alkalinization. * high altitude sickness - is accompanied by respiratory alkalosis. Acetazolamide treatment compensates by producing mild metabolic acidosis, thus offsetting it. |
|
|
Toxicity includes hyperchloremic metabolic acidosis with normal anion gap (Type II RTA) can occur, as well as hypokalemia.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
* hyperchloremic metabolic acidosis with normal anion gap (Type II RTA) can occur. *hypokalemia - any diuretic that increases flow rate thru distal tubules produces increased K+ secretion and hypkalemia DO NOT USE IN HEPATIC CIRRHOSIS! (shifts equilibrium of ammonia and ammonium towards ammonia, which goes to blood rather than gets excreted) |
|
|
Toxicity includes hyperchloremic metabolic acidosis with normal anion gap (Type II RTA) can occur, as well as hypokalemia.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
* hyperchloremic metabolic acidosis with normal anion gap (Type II RTA) can occur. *hypokalemia - any diuretic that increases flow rate thru distal tubules produces increased K+ secretion and hypkalemia DO NOT USE IN HEPATIC CIRRHOSIS! (shifts equilibrium of ammonia and ammonium towards ammonia, which goes to blood rather than gets excreted) |
|
|
Do NOT use in hepatic cirrhosis (shifts equilibrium of ammonia and ammonium towards ammonia, which goes to blood rather than gets excreted).
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
|
|
|
Do NOT use in hepatic cirrhosis (shifts equilibrium of ammonia and ammonium towards ammonia, which goes to blood rather than gets excreted).
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
|
|
|
even though acts in the early proximal tubule, it is a weak diuretic because the rest of the nephron operates in a "load dependent" fashion- the more sodium delivered to the rest of the nephron, the more it will reabsorb. So though it inhibits sodium reabsorb in proximal, it delivers more to distal segments which reabsorbs more too.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
A. Acetazolamide
|
|
|
Why is acetazolamide a weak diuretic even though it acts on the proximal tubule?
|
even though acts in the early proximal tubule, it is a weak diuretic because the rest of the nephron operates in a "load dependent" fashion- the more sodium delivered to the rest of the nephron, the more it will reabsorb. So though it inhibits sodium reabsorb in proximal, it delivers more to distal segments which reabsorbs more too.
|
|
|
These are part of the class of the most powerful diuretics.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
LOOP diuretics!
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
Produces diuresis because it inhibits the 3 ion cotransporter. At physiological pH, the loop diuretics are anions which compete for the Cl- binding site on the cotransporter.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
Used for the treatment of edema and hypercalcemia.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
Used for the treatment of edema and hypercalcemia.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
* hypokalemic metabolic alkalosis if treatment with this diuretic causes volume contraction.
* hyponatremia may occur in a patient on this diuretic who is polydipsic. * hypernatremia can occur in a patient on this diuretic who is dehydrated. * ototoxicity * magnesium depletion * hyperuricemia A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
Ototoxicity can occur with this diuretic.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
NaCl must be infused with this diuretic to prevent volume contraction.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Loop diuretics
H. Furosemide B. Bumetanide G. Ethacrynic acid |
|
|
Diuresis is produced b/c of NaCl cotransport inhibition in luminal membrane of early distal tubule cells.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Thiazides
C. Chlorathiazide I. Hydrochlorothiazide |
|
|
* treatment of edema
* treatment of HTN * treatment of idiopathic hypercalciuria * treatment of nephrogenic diabetes insipidus (1. inhibit NaCl reabs and thus dilution in that area, 2.decrease GFR and cause ECF volume contraction and thus increased prox tubule reabs of sodium and water --> decreased water excretion.) A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Thiazides
C. Chlorathiazide I. Hydrochlorothiazide |
|
|
Diuresis: Inhibit sodium reabsorption in late distal tubule and collecting duct by blocking sodium channels in the luminal membrane. Are weak diuretics b/c only a small fraction of filtered sodium is reabsorbed in late distal tubule.
K-Sparing: inhibit K+ secretion in late distal tubule and collecting duct by blocking the K+ secretion process which aldosterone normally stimulates. A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
K-sparing
L. Spironolactone M. Triamterene |
|
|
* combo with thiazide or loop diuretic to offset K+ wasting and prevent hypokalemia
* combo with thiazide or loop diuretic for patients with refractory edema A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
K-sparing
L. Spironolactone M. Triamterene |
|
|
Hyperkalemia is a possible adverse side-effect.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Ksparing diuretics
L. Spironolactone M. Triamterene |
|
|
This is the ONLY diuretic class to decrease K+ secretion. (All others increase K+ secretion.)
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Ksparing diuretics
L. Spironolactone M. Triamterene |
|
|
These diuretics excrete more calcium. (3)
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
A. Osmotic diuretics
B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) Remember: when Na reabs is inhibited, Ca reabs is too in these areas of the Nephron |
|
|
These diuretics excrete more calcium. (3)
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
A. Osmotic diuretics
B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) Remember: when Na reabs is inhibited, Ca reabs is too in these areas of the Nephron |
|
|
This diuretic class is the only one to DECREASE Ca excretion.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
D. Thiazides (chlorothiazide, HCTZ, metolazone)
reabs of Ca in the distal tubule is coupled inversely to Na reabs because of the presence of Ca-Na exchange. When Na reabsorption is inhibited by thiazide diuretics, Calcium reabsorption is stimulated. Thus, overall effect of thiazides is increased Na excretion and decreased Ca excretion (hypocalciuria). seep.347 for diagram |
|
|
This diuretic class is the only one to DECREASE Ca excretion.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
D. Thiazides (chlorothiazide, HCTZ, metolazone)
reabs of Ca in the distal tubule is coupled inversely to Na reabs because of the presence of Ca-Na exchange. When Na reabsorption is inhibited by thiazide diuretics, Calcium reabsorption is stimulated. Thus, overall effect of thiazides is increased Na excretion and decreased Ca excretion (hypocalciuria). seep.347 for diagram |
|
|
Regarding water balance with this diuretic, diluting AND concentrating the urine is messed up so urine tends towards ~isosmotic.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid)
inhibit the 3 ion cotransporter and thus inhibit countercurrent multiplication (decrease in corticopapillary gradient)---> decrease in urine concentraiton AND inhibit the dilution of urine which normally occurs in this gradient ---> increase in urine concnetraiton . |
|
|
Regarding water balance with this diuretic, urine cannot be diluted. (there is no effect on ability to concentrate urine).
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
D. Thiazides (chlorothiazide, HCTZ, metolazone)
nhibits the NaCl reabs in early distal tubule, which is also the cortical diluting segment) . This segment is NOT part of the loop of Henle thus does not participate in countercurrent so the only effect is that the urine cannot be diluted. (there is no effect on ability to concentrate urine). |
|
|
causes metabolic acidosis (Type II RTA) b/c it inhibits the reabs of filtered bicarb, thus increasing its excretion and thus loss of base from body causes blood [H+] to increase.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
B. Carbonic Anhydrase Inhibitors (Acetazolamide)
|
|
|
causes metabolic acidosis (Type II RTA) b/c it inhibits the reabs of filtered bicarb, thus increasing its excretion and thus loss of base from body causes blood [H+] to increase.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
B. Carbonic Anhydrase Inhibitors (Acetazolamide)
|
|
|
These two diuretics can yield volume contraction alkalosis.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid)
D. Thiazides (chlorothiazide, HCTZ, metolazone) |
|
|
These two diuretics can yield volume contraction alkalosis.
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid)
D. Thiazides (chlorothiazide, HCTZ, metolazone) |
|
|
produce metabolic acidosis (Type IV RTA) by blocking aldosterone-stimulated H+ secretion in the distal tubule and collecting ducts
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
E. K-Sparing (spironolactone, tramterene, amiloride)
|
|
|
produce metabolic acidosis (Type IV RTA) by blocking aldosterone-stimulated H+ secretion in the distal tubule and collecting ducts
A. Osmotic diuretics B. Carbonic Anhydrase Inhibitors (Acetazolamide) C. Loop diuretics (Furosemide, Bumetanide, Ethacrynic acid) D. Thiazides (chlorothiazide, HCTZ, metolazone) E. K-Sparing (spironolactone, tramterene, amiloride) |
E. K-Sparing (spironolactone, tramterene, amiloride)
|
|
|
Used for treatment of Central diabetes insipidus.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
D. chloropropamide
E. dDAVP |
|
|
Used for treatment of SIADH.
A. Acetazolamide B. Bumetanide C. Chlorathiazide D. chloropropamide E. dDAVP F. demeclocycline G. Ethacrynic acid H. Furosemide I. Hydrochlorothiazide J. Li+ K. Mannitol L. Spironolactone M. Triamterene |
Blockers of ADH action
J. Li+ F. demeclocycline |
|
|
Name some reasons for resistance to diuretics. (4)
|
1. Decreased secretion of diuretic by proximal tubule (renal insufficiency)
2. Hypoalbuminemia (as in nephrotic syndrome). Decreased plasma protein concentration means more diuretic is distributed in interstitial fluid rather than in plasma, thus there is lsess diuretic in plasma for filtration and secretion. 3. States with hyperaldosteronism- can haave loop ro thiazide resistance because of late distal tubule that reabs extra Na due to high aldo levels (load-dependent reabs). ***Giving Spironolactone additionally can help rectify the resistance.*** 4. Decreased delivery of Na to loop or Henle or distal tubule, as in CHF, or cirrhosis where GFR is decreased and prox tubule reabs is increased due to vasculr volume contraction. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is polydipsic.
|
Hyponatremia
loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is polydipsic.
|
Hyponatremia
loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is dehydrated.
|
Hypernatremia
in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is dehydrated.
|
Hypernatremia
in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is dehydrated.
|
Hypernatremia
in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is dehydrated.
|
Hypernatremia
in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is polydipsic.
|
Hyponatremia
loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine. |
|
|
[ Hypernatremia / Hyponatremia ] can occur in a patient on a loop diuretic who is polydipsic.
|
Hyponatremia
loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine. |
|
|
How is it that loop diuretics can cause both hypernatremia and hyponatremia?
(hint: conditions of water ingestion matters) |
Hyponatremia can occur in a patient on a loop diuretic who is polydipsic. loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine.
Hypernatremia can occur in a patient on a loop diuretic who is dehydrated. in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |
|
|
How is it that loop diuretics can cause both hypernatremia and hyponatremia?
(hint: conditions of water ingestion matters) |
Hyponatremia can occur in a patient on a loop diuretic who is polydipsic. loop diuretics inhibit NaCl reabs in TALH which is normally a diluting segment. Thus, the ability to produce dilute urine is impaired in persons who need to produce dilute urine.
Hypernatremia can occur in a patient on a loop diuretic who is dehydrated. in this case, loop diuretic interferes with production of corticopapillary osmotic gradient and with kidney's ability to make appropriately concentrated urine. In these patients, ADH secretion is stimulated but urine cannot be concentrated due to diminished corticopapillary gradient. Too much water is excreted, resulting in hypernatremia nd hyperosmolarity of blood. |

