![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What are the characteristics of Acute Kidney Injury?
|
- ↓ GFR → Azotemia over days
- D/t renal ischemia or toxins - Reversible |
|
|
What can cause Acute Kidney Injury?
|
- Renal ischemia
- Toxins |
|
|
Is acute kidney injury reversible or irreversible?
|
Reversible
|
|
|
Are there symptoms of uremia in AKI?
|
No chronic uremia (urea in blood) symptoms
|
|
|
How does the size of kidneys change in AKI?
|
Usually kidney size is preserved
|
|
|
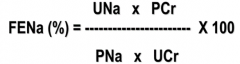
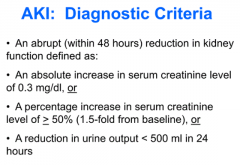
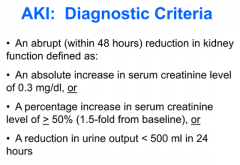
What are the diagnostic criteria of AKI?
|
Abrupt (within 48 hours) reduction in kidney function:
- Absolute ↑ in serum creatinine level of 0.3 mg/dl OR - Percentage ↑ in serum creatinine level of ≥ 50% (1.5 fold from baseline) OR - Urine output < 500 ml in 24 hours |
|
|
Why is AKI important?
|
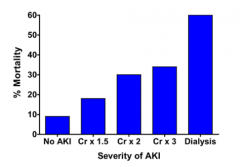
As AKI becomes more severe (↑ serum creatinine), increased % mortality
- No AKI: mortality is 10% - Dialysis d/t AKI: 60% |
|
|
What is Oliguria?
|
Urine output < 400-500 ml/day
|
|
|
What is Azotemia?
|
Elevation of nitrogen waste products related to insufficient filtering of blood by kidneys
|
|
|
What is Uremia?
|
Illness accompanying kidney failure which results from toxic effects of abnormally high concentrations of nitrogenous substances in blood
|
|
|
What do you look for in a Urinalysis, related to AKI?
|
- Casts: caused by trapping of cellular elements in matrix of protein secreted by renal tubule cells
- Granular casts ("muddy brown urine") seen in cases of acute tubular necrosis |
|
|
Over what range of BP are GFR and RBF auto-regulated?
|
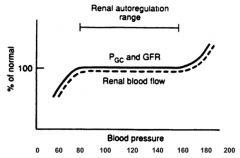
~80-160 mmHg (remains at normal)
- Lower BP leads to lower GFR and RBF - Higher BP leads to higher GFR and RBF |
|
|
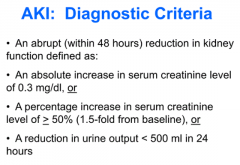
How does auto-regulation control GFR if there is a decreased perfusion pressure?
|
- Increased vasodilatory Prostaglandins dilate afferent arteriole
- Increased Angiotensin II constricts efferent arteriole - Maintains normal GFR |
|
|
What can inhibit prostaglandins? How does this affect ability of kidney to auto-regulate GFR and RBF?
|
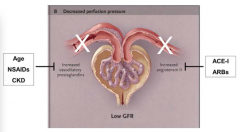
- Increased age, NSAIDs, and CKD all inhibit effects of vasodilatory prostaglandin on afferent arteriole
- Prevents dilation of afferent arteriole - Leads to low GFR |
|
|
What can inhibit Angiotensin II? How does this affect ability of kidney to auto-regulate GFR and RBF?
|
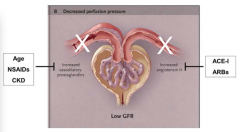
- ACE-I and ARBs inhibit effects of Angiotensin II
- Prevents constriction of efferent arteriole - Leads to low GFR |
|
|
What are the three categories of AKI?
|
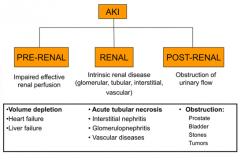
- Pre-renal
- Renal - Post-renal |
|
|
What can cause pre-renal AKI?
|
↓ Effective renal perfusion:
- Volume depletion - Heart failure - Liver failure ↓ GFR w/o ischemic or nephrotoxic injury to tubules |
|
|
What can cause renal AKI?
|
Intrinsic renal disease (glomerular, tubular, interstitial, vascular)
** Acute Tubular Necrosis - Interstitial Nephritis - Glomerulonephritis - Vascular diseases |
|
|
What can cause post-renal AKI?
|
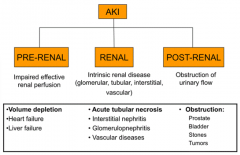
Obstruction of urinary flow from both kidneys
- Prostate - Bladder outlet obstruction - Ureteral obsturction - Stones - Tumors |
|
|
How does the kidney try to compensate for pre-renal AKI?
|
Decreased effective renal perfusion →
- Leads to increased AngII and Vasopressin → - Increased reabsorption of Na+ (at PT) and H2O → - Conc. urine → - Oliguria (appropriate) |
|
|
What are the characteristics of pre-renal AKI?
|
- Increased reabsorption of urea → elevation of BUN out of proportion to creatinine (>20:1)
- Usually reversible within 3-4 days if underlying cause is treated |
|
|
How does BUN compare to creatinine in pre-renal AKI?
|
Increased reabsorption of urea → elevation of BUN out of proportion to creatinine (>20:1)
|
|
|
How do you reverse pre-renal AKI? How soon?
|
Usually reversible within 3-4 days if underlying cause is treated
|
|
|
What are the histological features of Pre-Renal AKI?
|
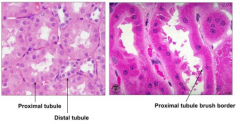
Normal tubular epithelium
|
|
|
What is the most common cause of Renal AKI?
|
Acute Tubular Necrosis (ATN): ischemic, toxic, or both
|
|
|
How does ischemia to kidneys cause reduced GFR and oliguria?
|
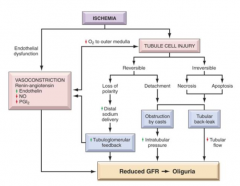
Ischemia →
- Vasoconstriction → - Tubule Cell Injury → Obstruction by casts or Tubular back-leak → Both: ↓ GFR → ↓ Oliguria |
|
|
What are the mechanisms of acute tubular necrosis?
|
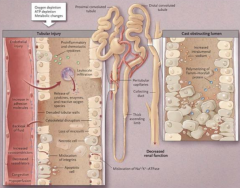
Causes of tubular injury:
- O2 depletion - ATP depletion - Metabolic changes Leads to: - Cast obstructing lumen - Decreased renal function |
|
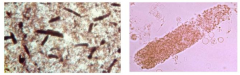
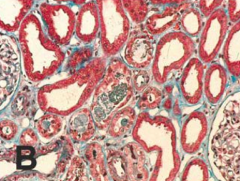
What does this image show?
|
Tubular obstruction in Acute Tubular Necrosis (Renal AKI)
|
|
|
What are the morphological features of Acute Tubular Necrosis (Renal AKI)?
|
- Tubular dilatation
- Attenuation (thinning) of tubular epithelium - Loss of epithelial cell brush border - Granular cast material in tubular lumen - Mitotic figures (regenerative change) |
|
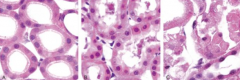
What do these images show?
|
Progression:
- Normal → - Early ATN (loss of tubular epithelial cells and debris in lumen) → - Necrotic tubules (necrosis and flattening of tubular epithelium) |
|
|
Following Acute Tubular Necrosis (Renal AKI), what happens?
|
- Tubular regeneration in coordinated fashion
- Sublethally injured tubular epithelial cells repopulate the tubules |
|
|
How do sub-lethally injured tubular epithelial cells repopulate the tubules in Acute Tubular Necrosis (Renal AKI)?
|
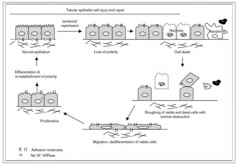
- De-differentiation →
- Proliferation → - Migration → - Re-establishing cell polarity |
|
|
Do stem cells help re-populate the tubular epithelial cells in Acute Tubular Necrosis (Renal AKI)?
|
No convincing evidence for direct re-population of tubules by intra-renal or extra-renal stem cells
|
|
|
What needs to be ruled out in all patients w/ oliguria?
|
Obstructive Uropathy (post-renal AKI)
|
|
|
Is post-renal AKI reversible? How?
|
Yes with relief of the obstruction
|
|
|
What happens if there is post-renal AKI?
|
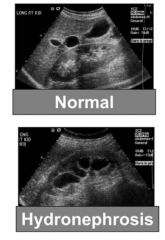
Hydronephrosis - distension and dilation of renal pelvis calyces
|
|
|
What are the most common causes of Acute Renal Failure / AKI?
|
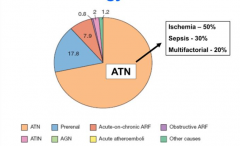
- ~ 70% ATN: 50% ischemia, 30% sepsis, 20% multifactorial
- 17.8% pre-renal |
|
|
How can you determine which type of AKI is causing the oliguria/AKI?
|
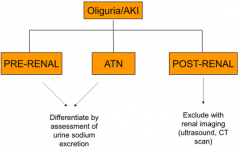
- Pre-renal: FENa < 1%
- Renal: FENa >2% - Post-renal: renal imaging (ultrasound, CT) FENa = fractional excretion of Na |
|
|
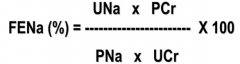
What is FENa?
|
Fractional Excretion of Na+ (FENa)
- Expressed as amount of Na+ excreted over amount of Na+ filtered by glomeruli |
|
|
What is the FENa (fractional excretion of Na) normally?
|
~1% (99% of Na+ reabsorbed)
|
|
|
How should FENa be affected by volume depletion (pre-renal AKI)?
|
Urine Na reabsorption should be increased in PT → FENa < 1%
|
|
|
How should FENa be affected by injury to proximal tubules (renal AKI)?
|
Na+ reabsorption will be impaired → FENa > 2%
|
|
|
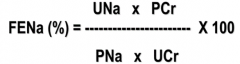
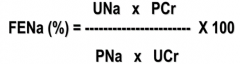
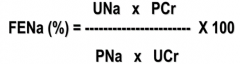
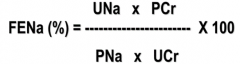
How do you calculate FENa?
|
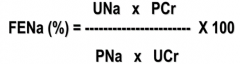
|
|
|
What is the purpose of calculating FENa?
|
To differentiate between pre-renal azotemia and ATN (both common causes of oliguric acute renal failure)
|
|
|
Case 1:
60 yo male w/ 10y hx of HTN and CKD admitted w/ uncontrolled HTN. He is on HCTZ & metoprolol. BP was 190/120 mmHg. Serum creatinine of 1.5 mg/dl and BUN of 15 mg/dl. Started on Lisinopril and Amlodipine. Improved BP on day 2 of 150/90 mmHg and day 3 of 138/84 mmHg. Urine output of 1.8-2 L/day. Day 2 serum creatinine of 1.8 mg/dl and BUN of 26 mg/dl. Day 3 serum creatinine of 2.9 mg/dl and BUN of 38 mg/dl. Unremarkable urinalysis. Does this patient have AKI? |
Yes, change in serum creatinine over 48 hours is consistent w/ AKI
|
|
|
Case 1:
60 yo male w/ 10y hx of HTN and CKD admitted w/ uncontrolled HTN. He is on HCTZ & metoprolol. BP was 190/120 mmHg. Serum creatinine of 1.5 mg/dl and BUN of 15 mg/dl. Started on Lisinopril and Amlodipine. Improved BP on day 2 of 150/90 mmHg and day 3 of 138/84 mmHg. Urine output of 1.8-2 L/day. Day 2 serum creatinine of 1.8 mg/dl and BUN of 26 mg/dl. Day 3 serum creatinine of 2.9 mg/dl and BUN of 38 mg/dl. Unremarkable urinalysis. Does he have hematuria? Uremia? Oliguria? Polyuria? Azotemia? |
Azotemia
(Elevation of nitrogen waste products, BUN, related to insufficient filtering of blood by kidneys) |
|
|
Case 1:
60 yo male w/ 10y hx of HTN and CKD admitted w/ uncontrolled HTN. He is on HCTZ & metoprolol. BP was 190/120 mmHg. Serum creatinine of 1.5 mg/dl and BUN of 15 mg/dl. Started on Lisinopril and Amlodipine. Improved BP on day 2 of 150/90 mmHg and day 3 of 138/84 mmHg. Urine output of 1.8-2 L/day. Day 2 serum creatinine of 1.8 mg/dl and BUN of 26 mg/dl. Day 3 serum creatinine of 2.9 mg/dl and BUN of 38 mg/dl. Unremarkable urinalysis. What is the most likely cause for the change in serum creatinine? |
Impaired GFR auto-regulatory response to decrease in BP (d/t being on ACE-I and CKD)
|
|
|
Case 1:
60 yo male w/ 10y hx of HTN and CKD admitted w/ uncontrolled HTN. He is on HCTZ & metoprolol. BP was 190/120 mmHg. Serum creatinine of 1.5 mg/dl and BUN of 15 mg/dl. Started on Lisinopril and Amlodipine. Improved BP on day 2 of 150/90 mmHg and day 3 of 138/84 mmHg. Urine output of 1.8-2 L/day. Day 2 serum creatinine of 1.8 mg/dl and BUN of 26 mg/dl. Day 3 serum creatinine of 2.9 mg/dl and BUN of 38 mg/dl. Unremarkable urinalysis. What pain medication should this patient avoid when treating his chronic knee pain? |
NSAIDs can cause further derangement of auto-regulation of GFR
|
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. Does this patient have AKI? Why? |
Yes - urine output is consistent w/ diagnosis of AKI
(can't say whether she meets criteria for serum creatinine because original value was 2 weeks ago, need to be within 48 hours) |
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. Does she have hematuria? Uremia? Oliguria? Polyuria? Polydipsia? |
Oliguria: Urine output < 400-500 ml/day
|
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. What is the most likely cause of her AKI? |
Pre-renal AKI d/t extracellular fluid volume depletion
|
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. What would you expect her FENa to be? |
FENa < 1% because she has Pre-renal AKI d/t extracellular fluid volume depletion
|
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. Additional labs show: serum Na+ 144 mEq/L, urine Na+ 12 mEq/L, urine creatinine 160 mEq/L. Urine microscopy shows 1-5 WBCs / high power field. Renal ultrasound shows no hydronephrosis. How do you interpret this new information? |
Fractional Excretion of Na+ is consistent w/ pre-renal AKI
|
|
|
Case 2:
80 yo woman admitted w/ 4-day hx of nausea, vomiting, and diarrhea. Fluid intake has been low. Feels light-headed upon standing for last 24 hours. Passed one cup of dark yellow urine in 24 hours. Takes acetaminophen 1-2x/week, HCTZ, and simvastatin. BP 84/60 mmHg and HR 110 bpm. Appears ill w/ poor skin turgor. Serum creatinine of 5.5 mg/dl and BUN of 87 mg/dl. 2 weeks ago her serum creatinine was 1.4 mg/dl. Urine output was 378 ml in one day. Based on diagnosis of Pre-Renal AKI, what is the next best course of action? |
Administer 2L of normal saline
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. Does this patient have AKI? Why? |
Yes, urine output < 500 ml in 24 hours
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. Which of the following is present: hematuria? Uremia? Oliguria? Polyuria? Polydipsia? |
Oliguria: Urine output < 400-500 ml/day
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. What is the most likely cause of AKI? |
Ischemic acute tubular necrosis from septic shock
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. What additional findings would you expect? |
Muddy brown granular casts on urine microscopy d/t ATN
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. Additional testing shows serum Na+ 140 mEq/L, urine Na+ 52 mEq/L, urine creatinine 50 mEq/L. Urine microscopy shows 3-5 muddy brown casts and 1-5 WBCs per high power field. Renal ultrasound showed no hydronephrosis. How do you interpret this data? |
Fractional Excretion of Na+ is consistent w/ acute tubular necrosis (>2%)
|
|
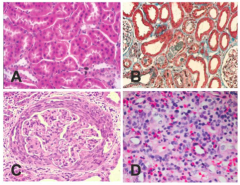
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. Which of these biopsies is most consistent with his type of AKI? |
|
|
|
Case 3:
52yo male w/ hx of liver transplant 2 yrs ago, hospitalized w/ 10-day fever, cough, and progressive lethargy. Oral intake has been poor for 3 days. Took acetaminophen before coming. Two days after admission he developed worsening HypoTN and increased respiratory distress. Intubated and mechanically ventilated. Received 20L of IV fluids for 2 days to treat shock. No NSAIDs or ACE-I. Temp is 103.9, BP 70/44 mmHg, HR 122 bpm. Decreased breath sounds in R midlung. Serum creatinine is 3.8 mg/dl and BUN is 54 mg/dl. Liver function is normal. Serum creatinine was 1.1 mg/dl last month. Urine output was 280 ml in first 24 hours. Transplant team is considering changing his immunosuppressant. They would like to start him on Rapamycin (anti-proliferative). Nephrologist suggests to wait until patient's renal function improves. Why? |
Rapamycin may impair renal tubular regeneration
|

