![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
Describe the clinical significance of acute renal failure
|
-Occurs in 5-10% of hospitalized patients
-Occurs in up to 25% of ICU patients -Mortality rate is high especially for severe ARF (20-40%) -Contributes to morbidity of critically ill patients -Correct diagnosis and treatment depend upon knowledge of pathophysiology |
|
|
What are the major causes of hospital acquired acute renal insufficiency?
|
-Decreased renal perfusion
-Medications -Radiographic Contrast Agents -Post-operative -Sepsis |
|
|
How do we measure the severity of acute renal injury?
|
Serum markers BUN and creatinine. These give an indication of GFR. As GFR falls both of these build up in the blood. The higher the serum creatinine the higher the mortality
|
|
|
Define acute renal failure
|
-A rapid deterioration of renal function (GFR) associated with the accumulation of normally excreted nitrogenous and other waste products
-All forms of ARF typically have an elevated blood level of creatinine and BUN |
|
|
Describe the 3 major patterns of acute renal failure
|
-Post-renal azotemia (obstruction)
-Pre-renal azotemia (perfusion problem) -Intrinsic renal failure (acute tubular necrosis, acute interstitial nephritis, acute glomerulonephritis, vascular disease) |
|
|
Describe Post-renal Azotemia
|
-ARF caused by obstruction of the outflow of urine
-Blockage can occur at any level from the urethra to the pelvis of the kidneys -Common causes are prostatic enlargement due to beining hypertrophy or cancer, gynecologic malignancies, kidney stones -Anuria (<100cc/day) suggests obstruction |
|
|
What are the 3 rules of post-renal azotemia?
|
-Exclude obstruction in every case of ARF
-Radiologic tests (IVP, CT scan, etc) can show there is no blockage In most cases use ultrasonogrram -Unilateral obstruction does not cuase progressive severe ARF |
|
|
Describe pre-renal azotemia
|
-An oliguric condition, associated with decreased GFR and retention of nitrogenous wastes, caused by decreased perfusion of the kidney
-Occurs in states of volume depletion and volume overload -Potentially rapidly reversible if underlying cause is fixed |
|
|
Describe how pre-renal azotemia can develop into acute tubular necrosis and how to distinguish the two
|
-If you have enough fluid loss, your BP drops, the kidney swings over from pre-renal azotemia and develops acute tubular necrosis.
-Severe decreases in BP can cause ATN. -Mild and moderate only cause pre-renal azotemia. -If you treat and it rapidly reverses it was just pre-renal azotemia. You can also look at the findings based on the pathophysiology. |
|
|
Describe the urinary findings in pre-renal azotemia
|
-Low urinary Na+ concentration (<20 mEq/L) and low FeNa+ (<1%)
-Large increase in BUN High BUN/Pcreatinine ratio (>20:1) -Increased urine osmolality (>400 mOsm/L) and urinary specific gravity |
|
|
Why is there a high BUN/Pcreatinine ratio in pre-renal azotemia?
|
-Creatinine is filtered and not reabsorbed at all, urea is partially filtered and then some is reabsorbed.
-In pre-renal azotemia with a low flow state there is a fair amount of back reabsorption of urea. -This BUN/Pcreatinine is high. Both are elevated, but the BUN is much higher. -In pre-renal azotemia the tubules work fine. |
|
|
Describe reabsorption in pre-renal azotemia
|
-In any decreased renal perfusion state the amount of glomerular filtration per unit renal blood flow increases
-Filtration fraction goes up which causes forces that lead to Na reabsorption in the proximal tubule -The RAS axis is turned on leading to increased Na reabsorption in the distal tubule -If you reabsorb your Na proximally and distally then the fractional excretion of Na excretion if low and the concentration in low. |
|
|
Describe acute tubular necrosis
|
-Most common pattern of intrinsic ARF
-Physiologic syndrome not morphologic -Two etiologies: Ischemic and Nephrotoxins -Has classic oliguric and diuretic phases -There is a non-oliguric ATN |
|
|
What is oliguria?
|
Urine output below 400ml/day
|
|
|
What is anuria?
|
Urine output below 100 ml/day
|
|
|
What is the common cause of non-Oliguric ATN?
|
Nephrotoxins
|
|
|
Describe the urinary findings in acute tubular necrosi-High urinary Na+ concentration (>40 mEq/L) and high FeNa+ (>1%)
|
-Unchanged BUN/plasma creatinine ratio in blood (10-15/1)
-Fixed urine osmolality (300mOsm/L) and urinary specific gravity (1.010) |
|
|
Describe Non-Oliguric Acute Tubular Necrosis
|
-Increasing in incidence
-Common with Nephrotoxins -Difficult to Recognize -Lower morbidity and mortality |
|
|
Describe the mechanisms of acute tubular necrosis
|
-Ischemic animal models of ATN (renal artery clamping, infuse intraarterial vasoconstrictor)
-Nephrotoxic Animal Models (HgCl2, Uranyl Nitrate, Gentamicin, Cisplatinum, Cyclosporine) -Not all models have the same pathogenesis -More than one mechanisms may be involved in each model of ARF |
|
|
Why is the GFR reduced in acute tubular necrosis?
|
-Vasoconstriction
-Back leak of tubular fluid -Intratubular Obstruction -Altered glomerular permeability |
|
|
Describe the role of Renin-Angiotensin System in ARF
|
-Early studies - JGA hyperplasia (JGA is where renin is secreted)
-Increased plasma Renin and AII levels in ARF -Experiments with blockers of Renin-AII system ameliorate acute renal failure -Tubuloglomerular feedback theory |
|
|
Describe the enzymatic cascade of the renin angiotensin system
|
-Angiotensinogen is made in the liver
-Renin is made in the kidney and converts angiotensinogen to angiotensin I -ACE is made in various tissues and converts Angiotensin I and Angiotensin II -AII acts on the AT1 receptors causing: -Vasoconstriction -Cell growth -Sodium and fluid retention -Sympathetic activation |
|
|
What is the result of increased delivery of Cl- to the macula densa of the distal tubule?
|
-Local vasoconstriction of the afferent arteriole of the same glomerulus by vasoactive local hormones: AII, endothelin, adenosine, NO, prostacyclin
-This shuts down the blood flow to that glomerulus hence the drop in the GFR |
|
|
Describe back leak of tubular fluid
|
Normally you filter inulin, creatinine, and things that are not reabsorbed and they appear in the urine. If you have damage to the tubules (ATN). A lot can back leak through the damaged tubular epithelial cells. They are filtered, but the inulin and creatinine and everything else just go right back into the circulation.
|
|
|
Describe intratubular obstruction
|
Normally there is filtration and low pressure in the tubules. If you have blockage due to a cast the pressure rises. When it equals the filtration pressure you turn off glomerular filtration.
|
|
|
Summarize the pathogenesis of acute tubular necrosis
|
-There is a generation phase of inschemic or nephrotoxic insult
-There is reduced renal blood flow and release of modifying hormone -This is followed by a maintainance phase consisting of vasoconstriction, back-leak, tubular obstruction, and decreased glomerular permeability |
|
|
Describe the biochemical markers of cell injury
|
-Basal and max O2 consumption decrease
-Activation of phospholipases -Increased ROS -Increased permeability to K and Ca resulting in lower cellular K and increased cellular Ca -ATP levels decrease, AMP levels increase |
|
|
Describe the possible mechanisms of tubular cell injury and necrosis
|
-Ischemia or nephrotoxic insult leads to reduction of cell ATP and ADP levels
-There is an inability to regulate intracellular ions (Na and Ca) -There is swelling of cytosol, mitochondrial damage, and activation of enzymes -This leads to organellar damage and increased membrane permeability |
|
|
Describe the targets of treatment in acute renal failure
|
-Offset vasoconstriction
-Limit inflammation -Alter cell outcome with growth factors and survival factors -Change of dialysis prescription -If there is already established ATN you cannot prevent it, you cant readily reverse it. You can prevent it if you hydrate and give saline before the insult, but after the insult there is no way to prevent it. People recover and they recover at the same pace if you give these things or don’t. |
|
|
Describe what occurs with tubular epithelial cell injury and repair
|
-With ischemia or nephrotoxin there is a loss of polarity
-Na-K ATPs is normally along the basolateral and lateral side but it gets shifted to the apical side -There is necrosis and apoptosis/cell death -There is sloughing off of cells -There is a birth of cells along the basement membrane of the tubule, some from viable cells already there and some may be from stem cells -This proliferation goes on and then you get redistribution, redifferentiation, and reestabilishment of the polarity and you are back to where you were. |
|
|
Describe the outcomes of hospital acquired renal insufficiency
|
-Partial recovery of renal function 23%
-Discharged with increased Pcreat 17% -Discharged on chronic hemodialysis 3% -Death 20% |
|
|
What is the biomarker of acute kidney injury?
|
Serum creatinine, although NGAL and KIM-1 are looking promising
|
|

|
This is a normal ultrasound. The black is the cortex of the kidney. The white inside is the medulla of the kidney.
|
|
|
|
-This is a patient with benign prostatic hypertrophy that had a markedly elevated creatinine and BUN.
-The BPH lead to uretereal blockage and backup of urine. -His kidney is compressed into a little rim around this giant kidney. The hollow area is the dilated collecting system. -If this is due to the prostate or a gynecological tumor this will be bilateral because the blockage is low down. |
|

|
-This is a patient with benign prostatic hypertrophy that had a markedly elevated creatinine and BUN.
-The BPH lead to uretereal blockage and backup of urine. -His kidney is compressed into a little rim around this giant kidney. The hollow area is the dilated collecting system. -If this is due to the prostate or a gynecological tumor this will be bilateral because the blockage is low down. |
|

|
US is also good at showing kidney stones. This is a kidney with a kidney stone. There is a sharp cutoff at the stone and a shadow behind it. If you are looking for stones or obstruction, US is great.
|
|

|
-If you see these muddy brown granular casts in the urine sediment it is very suggestive that the patient has acute tubular necrosis.
-Many times you don’t see these. |
|
|
-This is a latex injection of those ARF animals.
-The top left is normal, then 6 hrs, 12 hrs, and 24 hrs. -At the end it is only the deeper nephrons that are being perfused. |
|
|
Here is a kidney glomerulus with the afferent and efferent arteriole.
|
|
|
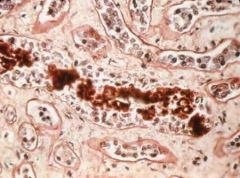
-If you look at biopsies from people who have crush injuries, you see casts of proteinacious material and debris blocking the tubule.
-This may be the same tubule going up and down. You only have to block it at one point. |
|
|
|
-EM of a normal kidney
-If you are sitting in Bowman's space and looking at the capillary loops you can see the visceral epithelial cells sitting on those capillary loops. |
|

|
-EM of a normal kidney
-If you are sitting in Bowman's space and looking at the capillary loops you can see the visceral epithelial cells sitting on those capillary loops. |
|

|
-EM of a nephrotoxic kidney
-This is what the cpaillary loops look like from Bowman's space. -You can sort of see a visceral epithelial cell, but there is marked damage. -The ultrafiltration goes down in these models. |
|
|
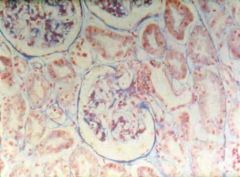
-Biopsy of ATN
-When you look at a biopsy of ATN sometimes you see simplifications of the tubular cells and loss of brush border. -Sometimes you don’t see anything abnormal when you look at it with light microscopy. |
|
|
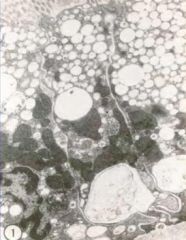
-EM of ATN
-If you look at an early stage at the tubular cells you see vacuolization and rounding up of the mitochondria. |
|

|
-EM of middle stages of ATN
-One cell still has a brush border. The other one has lost the brush border. There are lots of vacuoles, laminated wall type configurations. |
|

|
-EM of later stages of ATN
-Even later you find lot of debris and cells in the tubular lumen. |

