![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are common changes associated with Aseptic necrosis of the femoral head?
|

Femoral head sub luxated
Femoral head and neck remodelling & areas of lysis (-> lucency) New bone forming at cranio acetabular ridge |
|
|
|
What is a common place for osteophyte formation in the coxofemoral (hip) joint
|
cranial acetabular ridge
|
|
|
|
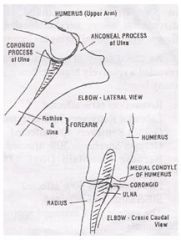
Where is the first place to look for osteophtye formation in the elbow?
|
Non articular edge of proximal anconeal process
|
|
|
|
What are important points for proper technique when imaging for musculoskeletal disease?
|
medium/fine or mammography screen -> good for detail
careful positioning -> GA a minimum of 2 orthogonal views collimation |
|
|
|
What are the types of epiphyseal fractures according to the Salter-Harris fracture classification?
|
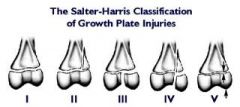
Type 1: physis fracture
Type 2: Physis + metaphysis fracture Type 3: Physis + epiphysis fracture Type 4: Epiphysis to physis fracture Type 5: Crush fracture |
|
|
|
Which are the most important diseases of the immature skeleton?
|
Primarily affecting joints:
- osteochondrosis, OCD - elbow dysplasia - UAP, FMCP, OCD - hip dysplasia - aseptic necrosis of the fremoral head (Legg-Perthes) Primarlily affecting bone: - trauma - panosteits - hypertrophic osteodystrophy - metabolic disorders eg. secondary hyperparathyroidism, dwarfism - metapyseal & epiphyseal dysplasias eg. chondrodysplasia, incomplete ossification, retained cartilage cores |
|
|
|
Where is the first place you would look for osteochondrosis lesions in the elbow?
|
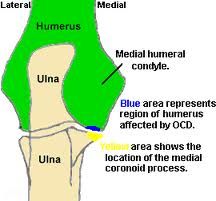
Medial humeral condyle
|
|
|
|
What is the best view to find osteochondral defects in the tarsus?
|
flexed dorsoplantar
|
|
|
|
Which is the primary site for osteochondral lesion in the tarsus
|
medial ridge of the trochlea
|
|
|
|
What are types of elbow dysplasia?
|
United anconeal process UAP
Fragmented medial coronoid process FMCP OCD Incongruity Often the only change seen is secondary -> DJD |
|
|
|
What is the difference between osteophytes and enthesiophytes
|
Osteophyte: new bone formation at periarticular margins
Enthesiophyte: new bone formation from traction at osseous attachments of ligaments or tendons |
|
|
|
What is the best view to asses the anconeal process
|
flexed lateral
also look for osteophytes on lateral epicondylar ridge, sclerosis of the trochlear notch and displaced FPC when assessing elbows |
|
|
|
What is panosteitis?
|

Medullary, diaphyseal sclerosis in young dogs (common GSD males)
painful! self limiting but can predispose for pathological fractures |
|
|
|
What is hypertrophic osteodystrophy & how does it present on x-rays?
|
developmental disorder of the metaphyses in long bones of young, growing dogs, usually of a large or giant breed
radiography reveals metaphyseal bone lucencies and circumferential periosteal bone formation |
|
|
|
What is synovial osteochondroma?
|

rare and benign metaplasia of the synovial membrane resulting in the formation of multiple intra-articular cartilaginous bodies
|
|
|
|
What 6 criteria are important when assessing aggressiveness of a bone lesion?
|
1. Location
primary bone tumours: generally metaphyseal area metastases within diaphysis (nutrient formane enter here) benign: anywhere 2. Bone destruction localised & uniform: probably benign moth eaten: likely malignant permeative: agressive/malignant process 3. Cortical destruction - look at endosteal as well as periosteal surface if none likely to be benign 4.Transition zone abrupt & short: benign, indisdinct/long: aggressive 5. Perisosteal reaction smooth, solid new bone: benign sunburst/spiculated: agressive 6. Rate of change rapid change -> aggressive |
|
|
|
What are some common fracture types
|

|
|
|
|
How does normal bone healing progress?
|
5-10d: fragments lose sharp edge, demineralisation -> fracture widens
10-20d: endosteal & periosteal callus, fracture gap narrows, fragments lose opacity >30d: fracture line disappearing, callus remodeling >90d: callus remodelling, cortical remodelling, etc. |
|
|
|
What are some complications of fracture healing?
|
Malunion: abnormal position
Delayed union: usually due to instability Non-union: atrophic or hypertrophic Osteomyelitis Osteoporosis Joint complications Fracture induced sarcoma |
|
|
|
What radiological changes would you expect to see with atlanto-axial subluxation?
|
Gap between C1 & C2 widens in flexed view -> dens moves dorsally and compresses the spinal cord
|
|
|
|
How can you classify myelographic lesion?
|
extramural
intramural-extramedullary intramedullary |
|
|
|
What defines cervical spondomyelopathy or "wobbler" syndrome?
|
cervical vetebral malformation/malformation syndrome
cervical instability vertebral subluxation vertebral canal stenosis that can be static or dynamic - result of congenital and degenerative changes |
|
|
|
What defines the Cauda equina syndrome?
|
static or dynamic stenosis of vertebral canal or intervertebral foramen causing compression of the nerve roots of the cauda equina
|
|
|
|
What defines Discosponylitis?
|
infection of intervertebral disc and secondarily of the adjecent endplates
L1-S1 most commonle affected most common in large breed male dogs |
|
|
|
What are causes for discosplonylitis?
|
hematogenous spread eg. UTI.. mainly Staph intermedius
direct infection eg. penetrating wound or migrating FB post Sx complication |
|
|
|
What are some radiographic changes associated with discospondylitis?
|
osseus proliferations - can spread along vertebral body
disc space collapse & sclerosis-> irregular intervertebral margins |
|
|
|
Which radiographic view would yo use to asses the nasal cavities & maxillary teeth?
|
DV with intra oral film
|
|
|
|
Which radiographic view would yo use to asses the zygomatic arches, internal & median ear & external ear as well as the TMJ?
|
Dorsoventral
|
|
|
|
Which radiographic view would yo use to asses the mandible?
|
VD with intraoral film
|
|
|
|
Which radiographic view would yo use to asses the TMJ and tympanic bullae?
|
closed mouth lateral oblique 20 degrees
|
|
|
|
Which radiographic view would yo use to asses the frontal sinus?
|
rostrocaudal frontal view
|
|
|
|
What radiographic changes can be seen with internal & median ostitis?
|
opacity in tympanic bullae
bone reaction: thickening of the wall, sclerosis, osteolysis and/or periosteal reaction sclerosis of the petrous bone expansion of the bullae (less common) |
|
|
|
How is US frequency related to resolution and penetration ?
|
High frequency = high resolution but low penetration
Low frequency = low resolution but high penetration |
|

