![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Soft Tissue Calcifications
types and what they look like |
Soft Tissue Calcifications
Soft tissue calcifications pop up all of the time, and it behooves the radiologist to say something intelligent about them. Fortunately the differential diagnosis for this finding is not too difficult. Soft tissue calcifications are usually caused by one of the following six entities. These are listed below in order of prevalence. Differential Diagnosis of Soft Tissue Calcifications Cause Typical Appearance Prevalence Dystrophic small to large amorphous Ca++ in the damaged tissue -- may progress to ossification (formation of cortex and medullary space are then seen) 95 - 98 % CPPD chondrocalcinosis; occasionally associated with calcifications in the soft tissues of the spine 1 - 2 % Metastatic calcification finely speckled Ca++ throughout soft tissues 1 - 2 % Tumoral calcinosis big globs of Ca++, usually near a joint << 1 % Metastatic osteosarcoma amorphous, fluffy, confluent collection of Ca++ <<< 1 % Primary soft tissue osteosarcoma amorphous, fluffy, confluent collection of Ca++ <<<< 1 % |
|

Name:
Common causes : |
ileus
Do supine and upright views. seeing dilated sm bowel i ntra ab causes: post op , post trauma psot inflamm : panc, enteritis, colitits pain related : renal colic, epidural dz Extra ab causes: septicemuia metabolic: hyperkal, uremia meds esp narcs prolonged bedrest post |
|

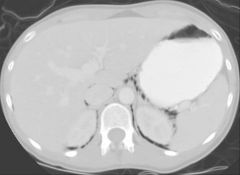
Fifty five year old female in the medical intensive care unit with severe congestive heart failure and acute abdominal pain and extension.
|
MS AB 10: Acute Intestinal Infarction with Pneumatosis and Portal Venous Gas
What films were obtained and in what position was the patient when they were taken? What are the major radiographic abnormalities? What is the likely cause of these abnormalities? loop by liver area that is darker is portal vein gas Discussion: Film #1 is an AP supine view of the abdomen. Films #2 and 3 are left lateral decubitus views of the abdomen taken in the AP projection with the patient lying on her left side. There are several abnormalities. The colon is markedly distended with air fluid levels. On film #1 and 3 one can see linear lucency's of gas density within the bowel wall representing pneumatosis intestinalis. All three films demonstrate linear branching structures of air density in the right upper quadrant representing gas within the portal vein of the liver. There are many possible causes for pneumatosis and portal vein gas, with the most serious being acute intestinal infarction with mucosal necrosis. |
|
dysphgia
|
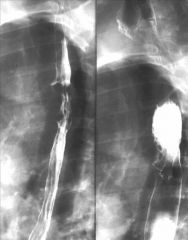
fixed narrowing
What type of study is this? What is the major radiographic abnormality and most likely diagnostic consideration? Discussion: These are multiple films from an air contrast barium esophagram. The patient has swallowed effervescent crystals followed by thick barium to distend the esophagus that pacify the lumen. The major finding is a fixed narrowing at the junction of the proximal and middle 3rd of the esophagus with marked mucosal irregularity and destruction. The morphology suggests a mucosal/mural mass lesion with the mucosal destruction favoring a malignant process. This is the typical radiographic appearance of esophageal carcinoma. Diagnosis: Esophageal carcinoma. |
|

25 year old male who suffered a stab wound to the right flank.
|
This is a CT scan of the abdomen performed with oral and intravenous contrast.
The major abnormality involves the right kidney, which has a large laceration in its posterior aspect (hallf-3/4 moon hole). The right kidney is surrounded by tissue of mixed density. This represents an acute perirenal hematoma (grey area). On the middle row of images, one can see high-density material (white spot) within the hematoma, which represents extravasated intravascular contrast indicating active acute hemorrhage. This was treated with angiographic embolization. A secondary finding is mixed density fluid in the right chest indicating a hemothorax with secondary partial collapse with the right lung. |
|

41 year old female with pelvic pain.
|
giant soft tissue beachball fills pelvis and into abdomen.
The plain radiograph shows a large ovoid soft tissue mass in the pelvis displacing large and small bowel into the upper abdomen. This is a non-specific finding which could be due to a pelvic mass of ovarian, uterine or other origins, or a distended urinary bladder. Film #2 is a pelvic ultrasound, the most widely used test to access female pelvic pathology. On the upper left frame, a longitudinal midline view, one can see the uterus posteriorly marked by cross hairs. The dark areas represent fluid. Inferiorly one can see a relatively collapsed urinary bladder. Above this is a large cystic mass with low level internal echoes and increased through transmission. Based on these findings the mass is almost certainly of ovarian origin. It is too large for a simple cyst. An ovarian neoplasm is the most likely diagnostic consideration. Surgical removal and pathologic evaluation would be needed for definitive diagnosis. Diagnosis: Serous cystadenoma of the ovary. |
|

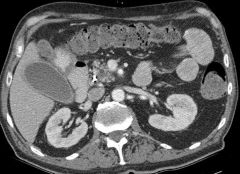
27 year old male with AIDS and progressive hip and back pain.
|
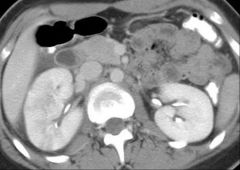
* Lymph adeno by mesenteric? vessels off aorta
* splenomegaly Discussion: This is a CT scan of the abdomen performed with oral and intravenous contrast. The major abnormality is multiple soft tissue density mass lesions surrounding the aorta and inferior vena cava and extending into the iliac region. This represents massive retroperitoneal lymphadenopathy. There is also enlargement of the spleen. Lymphadenopathy can be seen with lymphoma, certain granulomatous infections, and metastatic disease, among other considerations. This pattern of lymphadenopathy in a patient with aids is most likely due to malignant lymphoma. Diagnosis: Malignant lymphoma manifest as retroperitoneal lymphadenopathy and splenomegaly. |
|

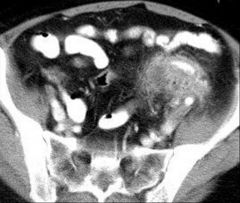
45 year old female with a pelvic mass.
|
Discussion:
This is a CT scan of the pelvis performed with oral and intravenous contrast. The major abnormality is a mass lesion in the mid right pelvis, which sits to the right and anterior to the uterus. Centrally, the mass is predominately of fat density(big black ball).The mass has a smooth soft tissue rim (grey)which contain several small foci of calcification (white specks). Posteriorly in the mass is a large nodule that contains both soft tissue and fat density. This represents an ovarian mass lesion, which contain calcium, fat, and soft tissue density material. This appearance is diagnostic of an ovarian teratoma. Diagnosis: Right ovarian cystic teratoma. |
|

50 year old male with left flank pain.
|
What type of radiographic examination is this? What is the major radiographic abnormality? What are some likely diagnostic considerations?
Discussion: The study is an AP radiograph of the abdomen performed following retrograde injection of contrast material into the left ureter via a cystoscope (retrograde ureterogram). The distal ureter appears normal. In the proximal ureter there is an ovoid filling defect, which causes partial obstruction to retrograde passage of contrast. There is faint opacification of some of the infrarenal collecting system that appears mildly dilated. A partially obstructing lesion with this morphology is almost always a renal calculus, which is passed into the ureter. A polypoid ureteral mass or tumor is an alternate consideration. Diagnosis: Partially obstructing left ureteral calculus on retrograde ureterogram. |
|

20 year old female with blunt trauma in a motor vehicle collision.
|
Discussion:
This is a CT scan of the abdomen with oral and intravenous contrast, the most common test performed for evaluation of blunt abdominal trauma. The spleen is the most abnormal organ. The spleen appears normal on the upper two images. The inferior aspect of the spleen appears very heterogenous. It is separated into numerous fragments by multiple low-density clefts representing splenic lacerations and fractures. There is an irregular focus of very high density in the center of the spleen which is similar in attenuation to the aorta. This represents active extravasation of blood in the fractured splenic hilum. This can be treated with transarterial embolization or surgery, depending on the patient's clinical status. around liver/on right : hemoperitoneum. Diagnosis: Grade IV splenic rupture with active extravasation. |
|
|
46 year old male with abdominal pain and abnormal liver function test.
|
What are the major radiographic abnormalities seen on the chest x-ray (Film #1)? pulm edema.
What type of study is depicted on Film #2? What are the hypoechoic (dark) branching structures in the upper left image of the liver? : top L hep, M hep, R hep. On other view IVC and hep vein. What do the other three images represent? What diagnostic considerations does this suggest that would explain the patient's symptoms? Discussion: Film #1 is a chest x-ray showing enlargement of the heart with vascular congestion and pulmonary edema. The patient has a Swan-Ganz catheter and a pacemaker/defibrilator indicating chronic heart disease. Film #2-5 is an ultrasound of the liver with doppler evaluation of the hepatic vessels. Image #2 shows dilated hepatic veins within the liver and #3 dilated IVC. The other images show a doppler waveform evaluation of the left hepatic vein (#4) inferior vena cava (#5). On the hepatic vein and vena cava wave forms there is flow both above and below the line, indicating two and fro flow. This abnormal flow in the abdominal veins is related to elevated right heart pressure from congestive heart failure. This can manifest as hepatomegaly and liver function test abnormalities and abdominal pain. Diagnosis: Passive hepatic congestion due to right heart failure. |
|

60 year old male with acute right flank pain.
|
* film has hydronephrosis : right side large circle at hilum.
* 2nd film see stone. The study is a CT scan of the abdomen and pelvis performed without contrast administration. The major abnormality is in the right kidney, which is enlarged compared to the left and has ill-defined perinephric stranding. The right renal collecting system is dilated, manifest as tubular and circular water density structures within the renal hilum. This is hydronephrosis. The dilated fluid filled ureter can be followed distally to the level of the bladder. In the expected position of the right ureterovesical junction (lower left images) there is a bright calcification located within the distal ureter. This represents an obstructing distal right ureteral calculus. Non-contrast CT has become the preferred method for evaluation of possible renal stone disease in the setting of flank pain and hematuria. Diagnosis: Obstructing distal right ureteral calculus. |
|

|
What tubes are visible on this radiograph? What is the location of these tubes? What complications can occur in this setting?
Discussion: Evaluation of this radiograph is limited by under penetration and multiple overlying monitor leads, a common occurrence. A nasogastric tube can be faintly identified coursing inferiorly over the left aspect of the spine with the tip in the left upper quadrant where the two leads cross. This is a nasogastric tube and appears to be in the stomach. A second tube is looped over the left lower chest with the tip not visible. This is a feeding tube which has been inadvertently directed into the trachea and left lower lobe airways. By its position it must have penetrated the pleura and is looped in the pleural space. Pneumothorax, empyema, and pneumonia can complicate this malposition catheter. |
|

66 year old female with chronic renal insufficiency.
|
Discussion:
Film 1 and 2 is an ultrasound of the kidneys, a study often performed with renal insufficiency to access for renal size and hydronephrosis. The primary abnormality is an incidentally discovered mass projecting off the lower pole of the left kidney. It has internal echoes and no increased through transmission, indicating a solid mass. Film 3-5 is from a CT scan performed with intravenous and oral contrast. The mass arising from the lower pole of the left kidney is well seen. It is of mixed attenuation, predominately in the soft tissue range, indicating a solid heterogenous mass. 95% of solid renal masses represent renal cell carcinoma. The treatment of choice is surgical removal. Diagnosis: Stage II left renal cell carcinoma. |
|

55 year old with right upper quadrant pain
|
What type of studies are displayed? What is the primary abnormality? What is the most likely diagnosis?
Discussion: Film 1 is a CT scan of the abdomen performed with oral intravenous contrast. Film 2 is an ultrasound of the right upper quadrant. Both studies demonstrate multiple ill-defined mass lesions within the liver. On CT these appear hypodense relative to the liver and ill defined, consistent with necrotic or mucinous neoplasia. On ultrasound the tumors appear predominately hyperechoic relative to the liver. The most common cause of multifocal ill-defined solid liver lesions is metastatic disease. This is a typical appearance for metastatic adenocarcinoma of any origin. Diagnosis: Metastatic adenocarcinoma to the liver from a colorectal primary. |
|
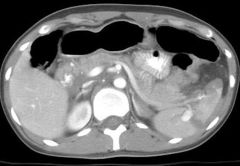
72 year old male with acute back and abdominal pain.
|
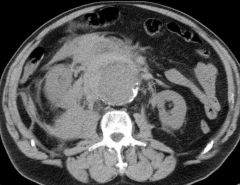
What type of study is this and how is it performed? What is the major abnormal organ? Based on density, what is the nature of the abnormality surrounding this organ. What is your diagnosis and what is the next step in management?
Discussion; The study is a CT scan of the abdomen and pelvis performed without contrast. The abnormal organ is the aorta, which is markedly dilated. This is seen as a tubular low-density mass anterior to the spine with a calcified wall. Surrounding the aorta is ill-defined tissue of intermediate (soft tissue) density. This high-density fluid represents acute hemorrhage in the retroperitoneal tissue planes due to rupture of the aneurysm. This is a life-threatening emergency, the only treatment for which is emergent surgery. Diagnosis: Ruptured abdominal aortic aneurysm. |
|

34 year old with cystic fibrosis and abdominal pain
|
Discussion:
The chest radiograph shows cystic bronchiectasis and heterogenous pulmonary opacities typical for cystic fibrosis. The abdominal radiograph demonstrates dilated small bowel with air fluid levels, out of proportion to the degree of colonic dilation. This suggests a mechanical small bowel obstruction. The CT confirms disproportionate dilation of small bowel. In the pelvis there is a loop of small bowel which has mottled gas and fluid within, reminiscent of stool. This is the typical appearance of a "meconium equalivent" where thick viscous pancreatic and small bowel secretions become inspissated in the small bowel causing obstruction. Incidentally noted is fatty replacement of the pancreatic head seen in the upper left image, a typical finding in cystic fibrosis. The spleen is enlarged. Diagnosis: Mechanical small bowel obstruction due to "meconium equivalent" in a patient with cystic fibrosis. |
|

|
calcified fibroid and displaced bladder.
on other views, grey balls smaller size, other fibroids. Look at the scout radiograph first. What is the major abnormality and what is its density? What is the most likely diagnosis? Now look at the CT scan. Does this confirm this suspicion? Discussion: The scout radiograph from a CT scan shows a large mass in the pelvis, which is very dense indicating calcification. This has been termed "popcorn" calcification (really big popcorn). Calcifications such as this in the pelvis are almost invariably due to degenerated uterine fibroids. The CT scan confirms the presence of multiple mass lesions within the myometrium of the uterus. A pedunculated mass on the inferior aspect of the fundus is densely calcified. Diagnosis: Calcified uterine fibroid. |
|

20 year old with acute left upper quadrant pain.in setting of mono
|
split in spleen
hemoperitoneum Look at the plain radiograph first. Do any organs appear abnormal? Now look at the CT scan. There are two primary abnormalities-can you identify them? What is the diagnosis and what would be some likely underlying causes? Discussion: The abdominal radiograph is relatively gasless rendering an indeterminate pattern. The primary abnormality is a soft tissue density filling the left upper quadrant, with a rounded inferior margin projecting below the ribs. This represents marked enlargement of the spleen. Marked splenomegaly is confirmed on the CT scan. The upper portion of the spleen is heterogenous in attenuation and there is surrounding mixed density fluid representing blood. Blood is also seen in the pelvic peritoneum, the paracolic gutter and the right subphrenic space. There are many potential causes of splenomegaly, and enlarged spleens are at risk for rupture from minor trauma or spontaneous rupture. Common cause for acute splenic enlargement and rupture in young people is mononucleosis. Diagnosis: Mononucleosis with acute rupture of an enlarged spleen. |
|

42 year old on steroids for presumed Crohn's disease who presents with fever.
|
Discussion:
The study is a CT scan of the abdomen performed with IV and oral contrast. The major abnormality is an ill-defined mass in the right lobe of the liver. The mass is predominately of water density with interspersed areas of soft tissue density. This represents a complex cystic mass. Differential considerations include cystic neoplasms and liver abscess. Given the clinical history liver abscess is most likely. The treatment of choice is antibiotic therapy and percutaneous drainage. Note: The patient was subsequently shown to have a subacute ruptured appendix as the cause and did not have Crohn's disease. Diagnosis: Pyogenic liver abscess. |
|

31 year old female with an elevated INR from anticoagulant therapy and abdominal pain.
|
see appy and below stranding and thickening (thickening just above R kidney. App above that.)
What type of study is this and how is it performed? There is one major abnormality on these images. Can you identify it? What is the likely diagnosis and how should this be treated? Discussion: The study is a CT scan of the abdomen performed with both oral and intravenous contrast. The small bowel and right colon are well opacified and distended. The primary abnormality is an ill-defined tubular mass in the right lower quadrant which appears to extend from a thickened thecal wall. No normal appendix is visible. This mass represents an enlarged and inflamed appendix due to acute appendicitis. Treatment is surgical removal. Diagnosis: Acute appendicitis. |
|

40 year old with diabetic ketoacidosis and abdominal pain.
|
in front of and back of panc is low density areas. not normally there.
Discussion: This is a CT scan of the abdomen performed with both intravenous and oral contrast. The most striking abnormality is abnormal low-density tissue infiltrating the fat planes of the mesentery and retroperitoneum. This infiltrative process surrounds the pancreas, which appears slightly enlarged but otherwise enhances normally. This represents peripancreatic fat necrosis, inflammation, and fluid accumulation due to acute pancreatitis. One would expect the amylase and lipase to be elevated. CT is the procedure of choice for evaluating the local pathologic changes complicating pancreatitis. Fluid collections which can evolve into pseudocysts, parenchymal necrosis manifest as absent pancreatic enhancement, vascular occlusion, and infection are all complications that may ensue. Diagnosis: Acute pancreatitis complicated by retroperitoneal fat necrosis and fluid accumulation. |
|
17 year old female with fever and right lower quadrant pain.
|
R kidney has paler zones going to borders. These are "striated zones of dec enhancement".
These are CT scans of the abdomen performed after oral and intravenous contrast administration. Can you tell any differences between film #1-3 and film #4-6? Look carefully at the kidneys and blood vessels. Do you see any imaging abnormalities? What diagnosis would you entertain? Discussion: Film #1-3 reveals a CT performed during bullous intravenous contrast administration. The blood vessels are bright and the kidneys still demonstrate cortical medullary differentiation. Film #4-6 is a delayed CT performed during the nephrographic/excretory phases of renal enhancement. The left kidney is normal and demonstrates uniform enhancement and excretion. The right kidney is slightly enlarged. There are striated zones of decreased enhancement in multifocal locations throughout the right kidney. These are more conspicuous on the nephrographic images than they are on the cortical medullary phase images. This pattern of striated hypodensity is almost pathoanatomic for acute pyelonephritis. Most cases of pyelonephritis are clinically diagnosed and do not require imaging for confirmation. Occasionally patients are imaged for fever/or pain in which the diagnosis was not suspected. Imaging is also performed in patients who do not respond to antibiotic therapy, to look for complications such as abscess or obstruction. Diagnosis: Acute uncomplicated right pyelonephritis. |
|

42 year old with a history of hepatitis and abnormal liver function tests.
|
bright spot by midline : varix, has another in front of 2 diaph crux
LIver is nodular sufrace along surface by belly. spleen is enlarged. Discussion: The liver is abnormal in morphology. The left lobe is small and the caudate lobe is enlarged. The liver has a very nodular contour. The morphologic changes suggest advanced fibrosis. There is a large enhancing venous structure extending inferiorly from the portahepatis and falciform ligament toward the umbilicus. This represents a large umbilical varix. The spleen is enlarged. These findings are indicative of portal hypertension. The diagnosis of cirrhosis is usually based on a combination of clinical findings and biopsy. Imaging is performed to look for complications such as hepatocellular carcinoma. With the widespread use of CT, cirrhosis is occasionally first diagnosed based on findings at cross sectional imaging. THIS image shows lg caudate in front of right kidney, and varix again. Diagnosis: Advanced hepatic cirrhosis with portal hypertension. |
|
Elderly with hypertension
|
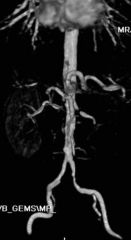
See spot of RAStenosis, black spot.
Discussion: These are contrast enhanced MR angiograms. This is performed with a breath hold 3D volumetric acquisition following the IV administration of a bolus of Gadolinium. The study takes approximately 20 to 30 seconds. The Gadolinium shortens the T1 relaxation time in the blood causing vessels to appear bright. There are multiple different methods for analyzing the 3D data set. For Film 37A film #3 demonstrates multiple different views from a volume rendered 3D reconstruction of the data. Film #4-6 shows a MIP (maximum intensity projection) reconstruction. Film #1-2 shows axial and coronal 2D reformations from the data set. Patient 37 A has high-grade stenoses of both renal arteries and the superior mesenteric artery(SMA not here) |
|

start of scan for elderly man HTN, name vessels:
|
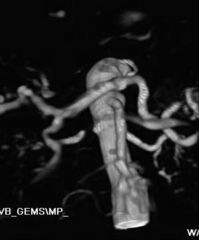
PRior: coming over top celiac axis,
coming off going down is SMA. This image: RAS. |
|
60-year-old female with left lower quadrant pain and leukocytosis.
|
Discussion:
The study is a CT scan of the pelvis with intravenous and oral contrast. The oral contrast has opacified the colon, which could also be opacified retrograde by an enema. The abnormal organ is the sigmoid colon, which demonstrates diffuse mural thickening with soft tissue stranding and small foci of fluid in the pericolonic fat. Inflammation and neoplasia are the most common causes of colon thickening. The most common inflammatory condition is diverticulitis. Pseudomembranous colitis and ischemic colitis can also produce this appearance. CT of the pelvis with enteric contrast is the procedure with choice for identifying and staging colon inflammation, including diverticulitis. Possible complications include abscess formation, fistulas, and bowel obstruction. Diagnosis: Acute sigmoid diverticulitis. |
|

Two separate patients, both elderly males with jaundice.
|
Discussion:
Laboratory assessment is the first step in distinguishing intrahepatic cholestasis from extrahepatic obstructive jaundice. Ultrasound is often the first test for suspected obstructive jaundice to look for dilated bile ducts. When present, CT scanning is the procedure of choice to determine the level and cause of obstruction. Endoscopic retrograde cholangiography may be diagnostic and therapeutic and MRI can be used in problem cases. The abnormalities on Film #1 include marked intra and extrahepatic biliary dilation, distension of the gallbladder, and a heterogenous mass enlarging the pancreatic head. A dense stent can be seen within the distal common bile duct, placed endoscopically for drainage. The pancreatic duct is dilated as well. This represents the "double duct" sign, with biliary and pancreatic dilation upstream from a mass. Film #2 demonstrates less marked biliary dilation and a stent in the distal common bile duct. The gallbladder is distended. The pancreatic body and tail are atrophic with ductal dilation. There is a subtle fullness to the pancreatic head suggesting a small mass. |
|
eld man jaundice contd
|
Discussion:
Laboratory assessment is the first step in distinguishing intrahepatic cholestasis from extrahepatic obstructive jaundice. Ultrasound is often the first test for suspected obstructive jaundice to look for dilated bile ducts. When present, CT scanning is the procedure of choice to determine the level and cause of obstruction. Endoscopic retrograde cholangiography may be diagnostic and therapeutic and MRI can be used in problem cases. The abnormalities on Film #1 include marked intra and extrahepatic biliary dilation, distension of the gallbladder, and a heterogenous mass enlarging the pancreatic head. A dense stent can be seen within the distal common bile duct, placed endoscopically for drainage. The pancreatic duct is dilated as well. This represents the "double duct" sign, with biliary and pancreatic dilation upstream from a mass. ** Film #2 demonstrates less marked biliary dilation and a stent in the distal common bile duct. The gallbladder is distended. The pancreatic body and tail are atrophic with ductal dilation. There is a subtle fullness to the pancreatic head suggesting a small mass. |
|

58 year old male with know pancreatic carcinoma presenting with pain, fever, and leukocytosis following endoscopic biliary stent placement.
|
prior: air/blk in biliary tree in liver.
This: abscess lying up to pabncreas CASE shows stent ERCP and then needle to drain abscess. Look at Film #1 first and identify how the exam was performed. What major imaging abnormalities do you see? What is the likely cause for the patient's symptoms? What is the appropriate treatment for this condition? Now look at Film #2 and identify what has happened in the interval. The upper left image is from the same day as the prior CT with the other three images representing a two-week follow up CT. Discussion: Film #1 is a CT of the abdomen performed with intravenous contrast. There is a biliary stent in place as well as air throughout the biliary tree from ERCP. The primary abnormality is a mass behind the pancreas surrounding the celiac axis. This has components of water and gas density and is most consistent with an abscess related to perforation from the ERCP. The primary treatment of choice for loculated intraabdominal abscess is an image guided percutaneous drainage performed by interventional radiology. On Film #2, the first image shows a needle placed in the retroperitoneal abscess from a posterior approach using CT guidance. This access was used to place a pig- tailed drainage catheter. The following three images show the pigtail drainage catheter in place with resolution of the abscess. Diagnosis: Post ERCP pancreatic abscess treated with percutaneous drainage. |
|

43 year old with blunt trauma in a motor vehicle collision.
|
retroper hemm: on right in front of obliques, solid grey density. not colon as not full of air and no walls.
Discussion: The primary abnormality is a large mass in the posterior right abdomen which extends from the perirenal area and para psoas region superiorly down into the right pelvis along the iliopsoas muscle and pelvic vasculature. The mass is retroperitoneal in location, displacing the kidney and colon anteriorly. The mass is of heterogenous density but largely similar to soft tissue, a pattern that is highly suggestive of hemorrhage. Blood has a higher density than water (compare with urinary bladder). The other imaging abnormality is fractures of multiple right lumbar transverse processes. Retroperitoneal hemorrhage in blunt trauma is usually managed conservatively, or with angiography if there is active bleeding. Bleeding into the retroperitoneum tends to tamponade itself and open surgery can cause the loss of tamponade. Diagnosis: Large right retroperitoneal hematoma from blunt trauma. |
|
28-year-old female injured in a fall from a horse
|
Identify the type of study and how it was performed. What major abnormalities do you see? How is this patient likely to be treated?
Discussion: There is mixed attenuation fluid throughout out the abdominal cavity representing hemoperitoneum. In the left upper quadrant the spleen is shattered into multiple pieces. In the center of the spleen is a globular focus of very bright contrast, similar to the aorta. This represents a pseudoaneurysm of the splenic artery from rupture. While endovascular treatment (embolization) is often used to treat splenic injuries, a fracture of this magnitude is most likely to be treated by emergent surgical splenectomy. |
|
27 year old with abdominal pain one day after colonoscopy.MS AB 51
|
Look at films #1 and 2 first (abdominal radiographs) what abnormality do you see? Concentrate on the gas pattern. Where do you think the gas is located? Now look at film #3 for correlation. What is your diagnosis and how is this condition usually managed?
Discussion: Abdominal radiographs show gas within parts of the large and small bowel, which are not dilated. There are also multiple linear foci of gas best seen along the flanks and marginating the psoas muscles and right kidney. These are not intraluminal. This distribution of gas indicates an extraperitoneal location. Film #3 is a CT of the abdomen and pelvis filmed at lung windows. The bowel is well opacified with contrast. Extensive linear foci of gas within the extraperitoneal spaces is well visualized, extending superiorly into the mediastinum. Extra peritoneal bowel rupture is the most common cause for pneumoretroperitoneum. It was iatrogenic in this case. For iatrogenic extraperitoneal colonic perforation most patients are treated conservatively with antibiotics and pain control. For gastroduodenal perforation surgery is more often necessary. Diagnosis: Pneumoretroperitoneum from iatrogenic colon perforation. |
|

organs outlined >
|
air outlines kidney of right
spleen on left |
|

what ?
|
penumonmediastinum
ms ab 51 |
|

75 year old with abdominal pain and fever.
|
Discussion:
The primary abnormalities involve the liver. The liver is lobular in contour with enlargement of the left lobe suggestive of cirrhosis. There is a large volume of ascites and the spleen is slightly enlarged. Liver attenuation is heterogenous with an infiltrative mass in the right lobe. A challenging but key observation is the fact that the portal vein is not opacified. It is diffusely replaced with low attenuation material representing tumor thrombus. Hepatocellular carcinoma is the most common neoplasm occurring in cirrhotic livers, and has a propensity for portal vein invasion. This latter aspect renders the tumor unresectable. Diagnosis: Advanced infiltrative hepatocellular carcinoma with portal vein invasion superimposed on hepatic cirrhosis. |
|

47-year-old female with abdominal pain and fever. The patient had been treated with Ciprofloxin for respiratory infection.
|
Look at film #1 first, what do you think of the bowel gas pattern?
TRANS COLON ABN PATTERN abnormal contour to the transverse colon and, less so, the cecum in the right lower quadrant and sigmoid colon in the left lower quadrant. The normal haustrations are not visible. There is undulating contour ("thumbprinting"), which indicates colon mural thickening. The CT scan (film #2), performed with oral but no IV contrast, confirms the abnormality throughout the entire colon. *** Pan colonic thickening** is most commonly due to an inflammatory colitis. The most common cause is pseudomembranous colitis caused by overgrowth of Clostridium Difficile. Other infections can also cause this appearance, such as e. coli and cytomegalovirus infection. A less common cause is idiopathic inflammatory bowel disease. Diagnosis: Antibiotic induced pseudomembranous colitis. |
|

22 year old with trauma.
|
This is a CT ab pelvis oral and intravenous contrast, the procedure of choice for evaluating the abdomen for blunt traumatic injury. The primary abnormality is a large low attenuation zone transecting the right lobe of the liver. This represents a large hepatic laceration and intrahepatic hematoma. There is a large amount of peritoneal fluid around the liver extending into the pelvis and left abdomen representing acute hemoperitoneum.
Treatment is based on the patient's clinical condition. If the patient is in shock, emergent surgery is generally performed. If the patient is relatively stable and active bleeding is evident, hepatic angiography with embolization is often performed. For stable patients without active bleeding, management is usually conservative. Major complications other than hemorrhage include injury to the bile ducts with biloma formation or secondary abscess formation. Diagnosis: Grade IV hepatic laceration with hemoperitoneum. |
|
|
Film #1, performed on January 20th in a patient with abdominal pain following a total colectomy for ulcerative colitis. The spleen has also been removed. What is the major imaging abnormality? Film #2 was performed 6 months later, in August. What does this demonstrate? What has happened in the interim?
Discussion: All three scan are CT scans of the abdomen performed with intravenous contrast. The major abnormality on Film #1 is abnormal low density filling the entire portal venous system and extending into the splenic vein and superior mesenteric vein. The veins are enlarged. This represents acute portamesenteric venous thrombosis. These patients are most commonly treated with anticoagulation. The major risk is bowel infarction. Film #2, performed 6 months later, shows complete resolution of the acute thrombus with scarring of the involved veins. Extensive collateral flow has developed with the mesenteric circulation entering the liver through numerous portal collaterals, which appear as small tubes and balls in the porta hepatis. This is termed cavernous transformation of the portal vein. Diagnosis: Acute portamesenteric venous thrombosis evolving into cavernous transformation of the portal vein. |

|
|

32-year-old female with abdominal pain and elevated serum lipase.
|
Discussion:
Film #1 is from a contrast enhanced abdominal CT. The primary abnormality is enlargement and ill definition of the pancreas compatible with uncomplicated acute pancreatitis. Alcohol abuse and gallstones are the leading cause of the pancreatitis. The gall bladder wall appears minimally thickened but no stones are evident. Film #2 shows an ultrasound of the right upper quadrant. This reveals gallbladder wall thickening and edema along with multiple echogenic shadowing stones within the gallbladder. The gallbladder was tender. The findings are compatible with acute cholecystitis. CT is the procedure of choice for evaluating patients with suspected complicated pancreatitis. CT is much less sensitive than ultrasound for gallstones. When gallstones or cholecystitis is suspected, ultrasound should be performed. Diagnosis: Acute cholecystitis with gallstone pancreatitis. |
|

25 year old male with abdominal pain and rectal bleeding.
|
The study is a single AP film from an air contrast barium enema, where dense barium and air are instilled into the colon to visualize the colonic wall. The colonic wall is extensively irregular with multiple small ulcerations along the wall. There are also numerous tiny apparent filling defects within the colonic wall. The appearance is that of a diffuse colonic inflammatory process with extensive mucosal ulceration. The most likely diagnostic consideration is inflammatory bowel disease, especially ulcerative colitis.
Diagnosis: Ulcerative colitis on double contrast barium enema. |
|

86 year old female with knee pain following trauma.
|
The study is an AP and lateral view of the knee with the patient supine. The lateral view is performed in a cross table fashion. The primary abnormality is a lucent line traversing the lateral tibial plateau indicative of a fracture. On the lateral view there is a joint effusion with a fat-fluid level in the suprapatellar bursa. This secondary sign indicates a lipohemarthrosis from an intraarticular fracture with bone marrow fat and blood in the joint space.
Diagnosis: Lateral tibial plateau fracture with lipohemarthrosis. |
|

31 year old with right hip pain.
|
The radiographs reveal sclerosis (increase density) in the medullary cavity of the right hip with loss of visualization of the normal trabecula and fine cortical line as compared with the normal left hip. On the lower image there is a pattern of irregular lucency in the lateral femoral head. This pattern of abnormal bone density is most commonly due to avascular necrosis. The MR study is a T1 (top) and T2 (lower) coronal view of the pelvis. These show geographic abnormal signal in the right femoral head compared with the normal left femoral head. MR is probably the most sensitive test for detection and staging of avascular necrosis.
Diagnosis: Stage II-III avascular necrosis of the right femoral head. |
|

44 year old with shoulder pain.
|
The first x-ray is an AP view of the shoulder with the humerus in external rotation. The second image is a "Grashey" view taken with the patient rotated 15 to 20 degrees posteriorly to visualize the glenohumeral joint in tangent. The abnormality is calcific densities superior to the greater tuberosity in the expected position of the insertion of the supraspinatus tendon. There is no donor site or underlying bone abnormality to indicate that this a fracture. Rather, this represents degenerative calcium deposits in the supraspinatus tendon.
Diagnosis: Calcific tendonopathy of the supraspinatus tendon. |
|

30 year old with trauma in a motor vehicle collision.
|
This is an AP radiograph of the pelvis taken with the patient supine on a backboard. The major abnormality involves the right hip. The femoral head is superimposed over the superior acetabulum indicating that it is dislocated, most likely in a posterior direction from direct impaction of the knee on the dashboard. There is a fragment of bone superior to the femoral head, which represents a displaced fracture of the posterior acetabular wall. Dislocated hips needs to be emergently reduced into the acetabulum to minimize the risk of subsequent avascular necrosis. Large posterior wall fractures need to be surgically repaired.
Diagnosis: Posterior dislocation of the right hip with a posterior acetabular wall fracture. |
|

45 year old with knee pain following a twisting injury.
|
Image #1 and 2 are AP and cross table lateral views of the right knee. Images #3 and 4 are oblique views of the knee. The primary abnormalities are multiple lucency's extending through the mid tibial plateau with cortical disruption, indicating a fracture. These are best visualized on the oblique views, emphasizing the importance of multiple projections to accurately identify fractures. Secondary abnormalities include a small avulsion fracture from the tip of the fibular malleolus at the site of the conjoined tendon insertion and a large effusion distending the suprapatellar bursa.
Diagnosis: Tibial plateau fracture and fibular avulsion fracture at the conjoined tendon insertion. |
|

30 year old with trauma in a motor vehicle collision.
|
This is a lateral cervical spine radiograph performed in the trauma bay. The obvious abnormality is disruption of the normal spinal lines with anterior dislocation of the C4 vertebral body relative to C5. There is no fracture visible. The inferior facets of the C4 vertebra are abnormally locked anterior to the inferior facets of the C5 vertebral body. This pattern of injury has a high rate of cord damage. Emergent spinal traction with relocation is the initial step in management. The tubes evident include a nasoenteric tube extending through the esophagus and an endotracheal tube entering the upper airway.
Diagnosis: C4-5 dislocation with bilat jumped facets. |
|

25 year old with elbow pain following trauma.
|
The primary abnormality is an abnormal piece of bone superimposed over the distal lateral humerus with cortical irregularity of the radial head. This indicates a radial head fracture. LAT view shows elevated fat pad above ?trochlea.
The secondary abnormality is displacement of the anterior and posterior humeral fat pads indicating a hemarthrosis of the elbow joint. Diagnosis: Displaced radial head fracture, intraarticular, with elbow hemarthrosis |
|

A 19 year old with shoulder pain following a snow boarding injury.
|
Both images are AP radiographs of the shoulder with the first image in external rotation and the second image in internal rotation. The abnormality is widening of the acromial clavicular joint with superior displacement of the clavicle.
Acromial clavicular separation ("shoulder separation") is divided into three grades. Grade I injuries is a partial injury to the joint capsule with intact coracoclavicular ligaments. Radiographs are normal. Grade II injuries reflect complete disruption of the acromioclavicular joint with partial tearing of the coracoclavicular ligaments. Grade III is complete disruption of the joint capsule and coracoclavicular ligaments. Imaging with and without weights is performed to access Grade II injuries. Gross displacement such as this is indicative of a Grade III injury. |
|

A 19 year old with shoulder pain following a snow boarding injury.
|
Both images are AP radiographs of the shoulder with the first image in external rotation and the second image in internal rotation. The abnormality is widening of the acromial clavicular joint with superior displacement of the clavicle.
Acromial clavicular separation ("shoulder separation") is divided into three grades. Grade I injuries is a partial injury to the joint capsule with intact coracoclavicular ligaments. Radiographs are normal. Grade II injuries reflect complete disruption of the acromioclavicular joint with partial tearing of the coracoclavicular ligaments. Grade III is complete disruption of the joint capsule and coracoclavicular ligaments. Imaging with and without weights is performed to access Grade II injuries. Gross displacement such as this is indicative of a Grade III injury. |
|

54 year old with ankle pain and inability to bear weight following trauma.
|
The abnormalities are a transverse fracture of the medial malleolus and an oblique fracture of the lateral malleolus, evidenced by cortical disruption and mild displacement. A secondary abnormality is abnormal widening of the ankle mortis, the space between the tibia and talus. The tibia is subluxed medially relative to the talus. The leg has been completely disconnected from the ankle and this is an unstable injury.
This is an eversion injury. When the ankle twists, fractures on the distracting side are transverse in orientation while fractures on the impacting side are oblique in orientation. |
|

31 year old with elbow pain and swelling
|
The lateral radiograph of the elbow shows displacement of the lucent fat pads anterior and posterior to the distal humerus. This finding is indicative of an elbow joint effusion. In the setting of trauma this is most commonly due to a hemarthrosis from an intraarticular fracture. The radial head is the most common bone injured. The AP view shows a subtle lucency traversing the radial head consistent with a non-displaced fracture.
Diagnosis: Non displaced radial head fracture with elbow hemarthrosis |
|

20 year old with shoulder pain following a fall.
|
The radiographics are AP projections of the shoulder with first image in external rotation and the second image in internal rotation. The major finding is a cortical step off on both sides of the greater tuberosity of the humerus indicating a non-displaced greater tuberosity fracture. Tuberosity fractures displaced less than 1cm. are treated conservatively with immobilization followed by physical therapy. External rotation views are very important for diagnosing this condition, but may be difficult to obtain in the acutely injured shoulder.
|
|

69-year-old diabetic with foot pain and swelling.
|
There are AP and oblique views of the forefoot and midfoot. The major abnormality is lytic destruction of the head of the 3rd metatarsal bone and the base of the proximal 3rd phalanx, with concomitant destruction of the metatarsal phalangeal joint. There is irregular periosteal new bone formation on each side of this destructive process. A lytic destructive process on both sides of a joint is most always due to septic arthritis. Diabetics with peripheral neuropathy and impaired circulations are prone to develop soft tissue ulcers, osteomyelitis, and septic arthritis.
Diagnosis: Septic arthritis and osteomyelitis of the left 3rd metatarsal bone and proximal phalanx. |
|

22 year old with foot pain.
|
There is a transverse defect in the base of the 5th metatarsal indicating a non-displaced fracture. This has been termed a "Jones Fracture". These are initially treated conservatively with external cast fixation. They have a relatively high risk of non-union due to traction from the peroneus brevis. This case resulted in non-union and required subsequent screw fixation.
Diagnosis: Non-displaced 5th metatarsal fracture. |
|

21 year old with knee pain following a fall.
|
On the AP view of the knee there are large lucency's extending through the patella with cortical disruption, indicating a comminuted fracture. Subtle areas of cortical disruption are visible on the lateral view. Secondary findings include a large hemarthrosis distending the suprapatellar bursa and marked soft tissue swelling anterior to the patella.
Diagnosis: Patellar fracture with hemarthrosis. |
|

18 years old with knee pain following trauma in a motor vehicle collision.
|
The AP view of the left tibia reveals a subtle linear focus of bone separated from the lateral tibial rim just above the fibular head. This is the site of the lateral capsular ligament attachment and avulsion fracture in this location is called a "Segond" fracture and is highly associated with anterior cruciate ligament tear. On the lateral view there is an irregular bony structure superimposed over the posterior joint space. This is not easy to visualize on the AP view. This also represents an avulsion fracture from the posterior cruciate ligament insertion on the mid posterior tibia.
Avulsion fractures are a clue to soft tissue injury. Their shape and location is frequently predictive of the origin. Further evaluation of the nature of these fractures and the associated soft tissue injuries is most commonly performed with CT and Magnetic Resonance Imaging. Diagnosis: One Segond fracture of the proximal left tibia. Posterior cruciate ligament avulsion fracture from the left tibia. |
|

40 years old with leg pain following trauma.
|
Two oblique views of the right ankle show marked soft tissue swelling medially. There is subtle disruption of the ankle mortis, manifest a slight a widening of the distance between the medial malleolus and talus compared to the distance between the talar dome and tibial plafond. There is no fracture evident. This pattern suggests disruption of the medial supporting structure of the ankle, the deltoid ligament. Right leg views show an oblique non-displaced fracture of the proximal right fibula. This pattern of abnormalities (deltoid ligament and proximal fibular fracture) indicates the patient also has torn the interosseous tibular fibular syndesmosis. The name given to this condition (medial ankle fracture or soft tissue injury and proximal fibular fracture) is a Maisonneuve fracture.
Diagnosis: Maisonneuve fracture of the proximal fibula with disruption of the deltoid ligament and tibial fibular interosseous membrane. |
|

48 year old with trauma in a motor vehicle collision.
|
Film #1 is an AP radiograph of the pelvis, which shows that the femoral heads are not superimposed on the acetabulum, but rather are displaced superiorly. They must also be displaced anteriorly or posteriorly, with the posterior dislocation being by far the most common. This is due to the knee striking the dashboard at the time of impact driving the hip joints out of their sockets. This is commonly associated with acetabular fractures, although none are evident in this case. Film #2 was performed after manual reduction of the bilateral hip dislocation.
|
|

20 year old with foot pain following trauma
|
The primary abnormalities are transverse fractures through the basis of the 2nd, 3rd and 4th metatarsal bones. On the oblique and AP views there is also lateral displacement of the 2nd and 3rd metatarsal bases relative to the middle and medial cuneiform bones, respectively. This indicates subluxation at these joints. Fractures/dislocations of the metatarsal bases and tarsal metatarsal joints are termed the Lisfranc fracture. This injury is named after a general in Napoleon's army who pioneered amputations at the tarsometatarsal joint, now termed the Lisfranc joint.
|
|

33 year old with shoulder pain.
|
What radiographic projections are displayed? What is the major radiographic abnormality? What prior surgery has the patient undergone?
Film #1 demonstrates an AP view of the shoulder in internal rotation, Film #2 a "Grashey" view (AP oblique tangent to glenoid). Film #3 shows a scapular "Y" view to view the relation of the humeral head and glenoid with Film #4 being another AP internal rotation view. The major abnormality is anterior-inferior dislocation of the humeral head relative to the glenoid. This is the most common dislocation of this very mobile joint. There are multiple radiopaque arrows in the anterior margin of the glenoid from prior surgical repair of the torn glenoid labrum and joint capsule (Bankart repair). Diagnosis: Recurrent anterior shoulder dislocation with history of prior capsular labral repair. |
|

20 year old with trauma in a motor vehicle collision.
|
The study is a lateral cervical spine radiograph performed in the initial evaluation of trauma victims. The major abnormality is disruption and separation of the pedicles of the C2 vertebral body from the vertebra itself, with anterior subluxation of C2 on C3. This pattern of spine injury is termed a "hangman's fracture" and is an unstable injury. The patient should be immobilized and placed in halo traction with subsequent evaluation both clinically with CT and MRI for cord injury.
Diagnosis: Hangman’s Fracture |
|
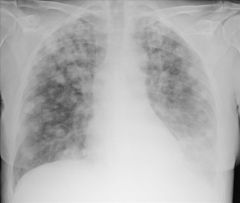
60 year old female with shortness of breath.
|
This single AP view chest radiograph reveals innumerable ill-defined nodular opacities throughout both lungs. These vary in size. The nodules are not calcified. Neoplastic disease and granulomatous disease are the most common causes of nodular opacities in the lung. In a patient of this age, the most likely diagnosis would be metastatic cancer. This patient had a history of endometrial carcinoma.
Diagnosis: Diffuse pulmonary metastases. |

