![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
562 Cards in this Set
- Front
- Back
|
The hip complex consists of... *** |
- pelvis
- hip joint |
|
|
The pelvis consists of... ***
|
- hip bones
- sacrum - coccyx |
|
|
How much mobility does the pelvis have at the SI joint? At the pubic symphysis? ***
|
very little
|
|
|
Another name for the hip joint ***
|
coxafemoral joint
|
|
|
What is the hip joint? ***
|
the articulation between the acetabulum of the hip bone and the proximal femur
|
|
|
Three bones that make up the os coxa ***
|
- ilium
- ischium - pubis |
|
|
Other names for hip bone ***
|
- os coxa (plural os coxae)
- innominate bone |
|
|
What type of joint is the hip joint? ***
|
- diarthrodial
- ball and socket - 3 degrees of freedom |
|
|
With what does the head of the femur articulate? ***
|
with the acetabulum of the hip bone (os coxa)
|
|
|
Describe the capsule of the hip joint. ***
|
- strong, dense, fibrous
- completely covers hip joint and most of femoral neck - acetabular labrum covers to distal portion of neck |
|
|
How is the capsule of the hip joint reinforced? ***
|
by three ligaments which play a major role in hip stability
|
|
|
What is the common function of the three extracapsular hip ligaments? ***
|
they all prevent excessive hyperextension
|
|
|
Describe the iliofemoral ligament ***
|
- anterior aspect
- a.k.a. “Y” ligament, or ligament of Bigelow - strongest ligament of the three: limits hyperextension |
|
|
Which is the strongest of the three extracapsular hip ligaments? ***
|
iliofemoral ligament
(a.k.a. “Y” ligament, or ligament of Bigelow) |
|
|
Describe the pubofemoral ligament ***
|
- anterior/inferior aspect
- limits hyperextension and internal (medial) rotation |
|
|
Describe the ischiofemoral ligament ***
|
- posterior aspect; spirals around superiorly;
- limits hyperextension and internal (medial) rotation |
|
|
How do the 3 primary extracapsular ligaments of the hip joint react to movement in the sagittal plane? ***
|
- slack during flexion
- become taut with extension - limit hyperextension |
|
|
Describe "resting on the Ys" and explain its importance. ***
|
- while standing, throwing the trunk backward and hyperextending hips in order to “rest on Y ligament” (takes no muscle action to maintain this posture)
- assumed by paraplegics in gait |
|
|
What is the ligamentum teres? ***
|
- attaches in the central portion of acetabulum (non-articulating area)
- goes to the fovea of the femoral head - of little stabilizing significance - contains blood vessel that supplies head of femur |
|
|
What structure contains the blood vessel supplying the head of the femur? ***
|
ligamentum teres
|
|
|
What is the iliotibial (IT) band? ***
|
- long tendinous band (part of the TFL muscle)
- attaches to iliac crest - runs laterally along thigh - attaches to lateral tibia - TFL and gluteus medius fibers attach to it |
|
|
What two muscles attach to the IT band? ***
|
- tensor fascia lata (TFL) |
|
|
What is the trochanteric bursa? ***
|
- fluid-filled sac situated between the gluteus medius and greater trochanter
- irritation causes hip pain |
|
|
What is the iliopsoas bursa? ***
|
- fluid-filled sac between the tendinous insertion of ilipsoas and pubis
- irritation causes groin pain |
|
|
Three bursae in the hip area ***
|
- trochanteric
- iliopsoas - ischial |
|
|
What are the functions of the hip joint? ***
|
- supports weight of HAT (head, arms, and trunk) in static and dynamic postures
- provides pathway for transmission of forces between pelvis and LE |
|
|
The hip joint is designed to operate primarily in a ____ kinematic chain. ***
|
closed
|
|
|
Why is the hip joint designed to operate primarily in a closed kinematic chain? ***
|
because for the majority of functional activities, the feet are fixed on ground and not freely moving in space
|
|
|
What is the close-packed position of the hip joint? ***
|
- hyperextension
(- adduction) - internal rotation (ligaments, capsule are taut but articular surfaces are not in optimal contact) |
|
|
What is the open-packed position of the hip joint? ***
|
- flexion
- abduction - external rotation (FABER) |
|
|
What are the two angulations of the neck of the femur? ***
|
- angle between axes of the neck and shaft (inclination)
- angle between axes of the neck and condyles (torsion) - how it’s twisted (condyles at 0 degrees, neck of femur should be around 12 degrees from them) |
|
|
What is a normal angle of inclination of the femur? ***
|
125 degrees
|
|
|
What angle is considered coxa vara of the femur? ***
|
- 105 degrees
|
|
|
What condition does coxa vara of the femur produce? ***
|
genu valga (knock knees)
|
|
|
What angle is considered coxa valga of the femur? ***
|
140 degrees
|
|
|
What condition does coxa valga of the femur produce? ***
|
genu varum (bowed legs)
|
|
|
Which abnormality in femoral inclination is more likely to result in fracture? ***
|
coxa vara (105 degrees)
(the smaller angle that produces knock knees) |
|
|
What is normal angle of femoral inclination in an elderly person? ***
|
120 degrees
|
|
|
How does femoral inclination contribute to fractures in females? ***
|
coxa vara (smaller angle of inclination), to which females are more predisposed due to their wide pelvises, is more likely to produce fracture
|
|
|
In which plane is angle of femoral inclination measured? ***
|
frontal plane
|
|
|
In which plane is angle of femoral torsion measured? ***
|
transverse plane
(it compares the rotation of the neck of the femur with the rotation of the shaft of the femur, as measured at the condyles) |
|
|
What is a normal angle of femoral torsion in an adult? ***
|
12-15 degrees
|
|
|
How does an increased angle of femoral torsion present? ***
|
- medial rotation of femoral shaft
- toe-in gait |
|
|
What is anteversion? ***
|
- increased angle of femoral torsion
- medial rotation of femoral shaft - toe-in gait |
|
|
How does a decreased angle of femoral torsion present? ***
|
- lateral rotation of femoral shaft
- toe-out gait |
|
|
What is retroversion? ***
|
- decreased angle of femoral torsion
- lateral rotation of shaft of femur - toe-out gait |
|
|
How do the angles of inclination and torsion affect the hip joint? ***
|
angles affect
- fit of the femoral head in the acetabulum and the - distribution of forces on the neck normal angles = optimal balance of bone stresses and muscle alignment |
|
|
What are some effects of abnormal angles of femoral inclination and/or torsion? ***
|
- hip joint instability
- compromise of weight-bearing structures of the hip - altered muscle alignment and force of pull |
|
|
What are trabeculae? ***
|
thin calcified plates laid down in response to stresses placed on bone
|
|
|
The ____ the trabeculae, the stronger the bone. ***
|
denser
|
|
|
Where do trabecular systems form? In response to what? ***
|
- along lines of stress in the bone
- due to weight bearing and/or muscle forces |
|
|
How do trabeculae function in the hip complex? ***
|
provide stability to the pelvis and hip joint by reinforcing those bony regions under great amounts of stress
areas where the systems intersect and are denser are areas of greatest strength |
|
|
What are zones of weakness? ***
|
- areas in the bone without intersection (portion of femoral neck region)
- result in less reinforcement and greater potential for fracture |
|
|
How is open chain motion at the hip carried out? ***
|
- femur moves on fixed pelvis
- convex on concave, thus roll and slide in opposite directions |
|
|
Describe flexion/extension at the hip joint. ***
|
- sagittal plane
- 120-135 degrees flexion with knee flexed - 10-30 degrees hyperextension |
|
|
Describe abduction/adduction at the hip joint. ***
|
- frontal plane
- 30-50 degrees abduction -10-30 degrees adduction |
|
|
Describe internal/external rotation at the hip joint. ***
|
- transverse plane
- 30-45 degrees IR - 45-60 degrees ER |
|
|
How is closed-chain motion at the hip joint carried out? ***
|
- pelvis moves on fixed femur
- convex on concave, thus roll and slide in same direction |
|
|
Name two types of closed-chain motion of the hip joint. ***
|
- anterior pelvic tilt
- posterior pelvic tilt |
|
|
What are the characteristics of an anterior pelvic tilt? ***
|
- sagittal plane
- ASIS moves anteriorly & inferiorly - hip flexion occurs - extension of lumbosacral spine - increased lordotic curve (to keep head over sacrum/COG) |
|
|
Why does the lordotic curve in the lumbosacral spine increase in response to an anterior pelvic tilt? ***
|
to keep the head over the sacrum and maintain the COG
|
|
|
What are the characteristics of a posterior pelvic tilt? ***
|
- sagittal plane
- ASIS moves posteriorly & superiorly - hip extension occurs - flexion of lumbosacral spine - decreased lordotic curve (to keep head over sacrum/COG) |
|
|
Why does the lordotic curve in the lumbosacral spine decrease in response to a posterior pelvic tilt? ***
|
to keep the head over the sacrum and maintain the COG
|
|
|
Describe a lateral pelvic tilt. ***
|
- hip hiking or pelvic drop (of the OPPOSITE hip)
- results in either abduction or adduction of hip joint (abduction hikes, adduction drops) |
|
|
Describe pelvic rotation. ***
|
- forward and backward rotation of pelvis on femurs
- results in either IR or ER of hip joint |
|
|
Which muscles are hip flexors? ***
|
- iliopsoas (strongest)
- rectus femoris - sartorius - tensor fascia lata |
|
|
Which is the strongest/primary hip flexor? ***
|
iliopsoas
|
|
|
Tightness of the iliopsoas leads to what? ***
|
increased lordosis in lumbar spine
(in addition to excessive hip flexion which may produce contractures) |
|
|
Function of rectus femoris ***
|
- flexes hip
- extends knee - part of quadriceps group - passive/active insufficiency positions |
|
|
Function of sartorius ***
|
- longest muscle in the body
- hip flexion, abduction, and external rotation (FABER) - knee flexion and internal rotation of the flexed knee - muscle used for “Indian sitting” or tailor’s muscle |
|
|
Function of tensor fascia lata ***
|
- short muscle with long tendinous attachment (IT band)
- crosses hip joint laterally and slightly anteriorly - combined hip abduction/flexion - assists with knee extension |
|
|
Other muscles that assist at the hip ***
|
- adductor group (magnus, longus, and brevis)
- pectineus - flexion of femur on fixed pelvis, or - anterior pelvic tilt with femur fixed |
|
|
Name the muscles comprising the force couple for anterior pelvic tilt. ***
|
- trunk extensors (erector spinae)
- hip flexors (iliopsoas, rectus femoris, sartorius, TFL) |
|
|
List the hip extensor muscles ***
|
- gluteus maximus
- hamstrings (semitendinosus, semimembranosus, and long head of biceps femoris) |
|
|
Name the strongest hip extensor. ***
|
gluteus maximus
|
|
|
Function of gluteus maximus ***
|
- hip extensor (strongest one)
- external rotator |
|
|
List muscles of the hamstrings ***
|
- biceps femoris
- semitendinosus - semimembranosus |
|
|
Function of hamstrings ***
|
- hip extension
- knee fleion - passive/active insufficiency positions (as they cross two joints--except short head of biceps femoris) |
|
|
Action of hip extensors ***
|
- extension of femur on fixed pelvis
- posterior pelvic tilt with femur fixed |
|
|
Name the muscles comprising the force couple for posterior pelvic tilt. ***
|
- trunk flexors (rectus abdominis)
- hip extensors (gluteus maximus and hamstrings) |
|
|
List the hip adductors. ***
|
- pectineus
- adductors (longus, brevis, magnus) - gracilis |
|
|
Function of pectineus ***
|
- hip flexion
- hip adduction |
|
|
Function of gracilis ***
|
- 2 joint muscle
- hip adduction - knee flexion/internal rotation |
|
|
List the hip abductors. ***
|
- gluteus medius
- gluteus minimus - TFL |
|
|
Action of the hip abductors ***
|
- abduct femur on fixed pelvis
or - stabilize pelvis during unilateral stance to prevent pelvic drop on opposite side |
|
|
List the external rotators of the hip. ***
|
- "deep six"
- piriformis - gemellus superior/inferior - obturator internus/externus - quadratus femoris - gluteus maximus - gluteus medius (posterior fibers) - sartorius |
|
|
Location of "deep six" ***
|
- deep rotators:
- six small deep muscles - span hip joint posteriorly & horizontally - originate from ischium/sacrum and - insert greater trochanter |
|
|
Function of "deep six" ***
|
- due to horizontal line of pull, tend to behave similar to rotator cuff muscles in shoulder
- serve as a stabilizer of the joint |
|
|
To which muscle group do the external rotators of the hip operate similarly? ***
|
the rotator cuff muscles of the shoulder
- horizontal line of pull - stabilizers - as they have a near-horizontal line of pull, they help compress the femoral head firmly into the acetabulum (as the rotator cuff muscles do at the GH joint) |
|
|
What other muscle can work as an external rotator of the hip? ***
|
gluteus maximus
(But the gluteus medius also has posterior fibers that externally rotate the hip....) |
|
|
List the internal rotators of the hip. ***
|
- gluteus medius (anterior fibers)
- gluteus minimus - TFL - adductor muscle group |
|
|
Primary internal rotator of the hip ***
|
gluteus minimus
|
|
|
List the common pathologies of the hip (the ones we covered, anyway). ***
|
- osteoarthritis
- bony abnormalities - fractures - muscle weakness |
|
|
Etiology of osteoarthritis of the hip ***
|
- degenerative joint disease
- deterioration of articular cartilage - associated with trauma to hip joint, misalignment, age, obesity |
|
|
Some causes of osteoarthritis of the hip ***
|
- trauma to hip joint
- misalignments (anteversion, abnormal angulation) - aging - increased weight-height ratio |
|
|
What is the most common painful condition of the hip? What is its prevalence? ***
|
- osteoarthritis
- 10-15% of persons over 55 |
|
|
Possible cause of osteoarthritis ***
|
recent studies reveal that deterioration of articular cartilage may be due to inadequate flow of nutrients and wastes through avascular cartilage due to decreased weightbearing activity
|
|
|
How do abnormal angles of inclination/torsion affect the hip? ***
|
- change the way forces act upon the hip
- can lead to pathologic hip conditions such as OA, femoral neck fractures, and muscular weakness around hip joint due to reduction of biomechanical effectiveness of muscle contraction |
|
|
Pathologies of the hip associated with cox valga ***
|
- decreased hip stability
- predisposes hip dislocation |
|
|
Pathologies of the hip associated with cox vara ***
|
- increases tensile bending forces on femoral neck
- predisposes femoral neck fractures, and slipped capital femoral epiphysis |
|
|
Pathologies of the hip associated with retroversion ***
|
toe-out walking
|
|
|
Pathologies of the hip associated with anteversion ***
|
- toe-in walking
- anterior dislocation of hip - OA |
|
|
Etiology of hip fractures ***
|
- bony failure of the hip joint can result in femoral neck fractures
- most common bony failure fractures occur at the zone of weakness--femoral neck region - most common in elderly population (females > males) - increased incident with osteoporosis, and increased incidence with coxa vara |
|
|
Result of gluteus medius weakness ***
|
- contralateral hip drop during unilateral stance (Trendelenberg)
|
|
|
How does gluteus medius normally perform to prevent contralateral hip drop? ***
|
- gluteus medius and minimus perform a reverse action
- during one leg stand, opposite pelvis has a tendency to drop - to prevent pelvic drop, the gluteus medius on the stance leg does a reverse action contraction (or co-contraction), pulling the pelvic origin toward the insertion and keeping the contralateral pelvis from dropping - gluteus medius keeps hips level (standing leg abduction, support leg gluteus medius gets more of a workout) - this occurs with every step during walking - weakness of the gluteus medius and minimus results in contralateral pelvic drop - this is called a “ Trendelenburg gait" or “Gluteus medius gait” |
|
|
Describe a “Trendelenburg” gait or “Gluteus medius gait.” ***
|
- gluteus medius weakness prevents keeping hips level due to inability to complete reverse action contraction to keep contralateral pelvis from dropping
- this occurs with each step |
|
|
How does gluteus maximus weakness or paralysis affect posture and gait? ***
|
- trunk thrown posteriorly to prevent hip flexion and trunk falling forward during erect posture or gait
- “hang on ligaments” |
|
|
Structure of the knee joint ***
|
two joints in one capsule
- tibiofemoral joint - patellofemoral joint |
|
|
Mobility of knee complex ***
|
- produces shortening/lengthening for LE
- provides mobility for foot in open space (open chain) |
|
|
Stability of knee complex ***
|
works with hip and ankle to support body weight during static and dynamic closed chain activates
|
|
|
What bony stabilizers /limiters does the knee complex have? ***
|
- none
- relies on ligaments, tendons, and muscles for stability |
|
|
Function of knee complex ***
|
- permits a large range of motion
- accommodates forces that can exceed weight of body (2-6 times the body weight) |
|
|
What factors predispose the knee to traumatic injury and degenerative disease? ***
|
- the freedom of motion within the complex
- the extreme forces to which it is subjected, and - the construction of knee complex |
|
|
Structure of tibiofemoral joint ***
|
- synovial, double condyloid joint with 2 degrees of freedom
- flexion/extension (0-130 degrees) - medial/lateral rotation (accompanies flex/ext) - distal convex femur (femoral condyles) articulates with proximal concave tibia (tibial plateaus) - medial condyle articulating surface longer than lateral condyle, medial tibial plateau larger than lateral plateau - asymmetrical, incongruent surfaces - large articular femoral condyles articulate with shallow concavities of tibial plateaus |
|
|
Describe the menisci of the knee. ***
|
- two: medial and lateral meniscus
- fibrocartilaginous discs - located on tibial condyles (plateaus) - half moon or wedge shaped; deepen the flat joint surface - many attachments to surrounding structures - distort and move anterio-posterior during knee flexion/extension |
|
|
How many menisci are contained within the knee? ***
|
two
|
|
|
Function of the menisci of the knee ***
|
- deepen the flat joint surface to improve articulation/congruency between femur and tibia
- serve as shock absorbers -- absorb 40 to 60% of imposed load on knee - increase the area for distribution of weightbearing forces - spread stresses out over all of articular cartilage region - decrease deterioration of hyaline cartilage by reducing friction |
|
|
Which meniscus is more frequently torn? ***
|
- medial meniscus much more firmly attached than lateral
- more frequently torn (MMT- medial meniscus tear more common) |
|
|
What is the healing potential of the meniscus? ***
|
- cartilage poorly vascularized (especially central 2/3);
- if torn, poor ability to repair in central areas |
|
|
Describe the joint capsule of the knee. ***
|
- large, lax, many attachments to nearby structures
- reinforced by surrounding muscles and ligaments - intricate synovial lining which folds in on itself in certain areas = synovial plicae (which can become irritated or pinched with knee joint movements) |
|
|
Describe the ACL. ***
|
- anterior cruciate ligament (ACL)
- intracapsular (extrasynovial- don’t get nourishment from it) - located between medial/lateral femoral condyles - attaches anterior tibia to posterior/lateral femur - prevents anterior movement of tibia on femur - provides anterior-posterior stability - controls excessive knee rotation |
|
|
Describe the PCL ***
|
- posterior cruciate ligament
- intracapsular (extrasynovial- don’t get nourishment from it) - located between medial/lateral femoral condyles - attaches posterior tibia to anterior/medial femur - provides anterior-posterior stability - prevents posterior movement of tibia on femur - controls excessive knee rotation |
|
|
List the collateral ligaments ***
|
- medial collateral ligament
- lateral collateral ligament - iliotibial band - other extracapsular ligaments |
|
|
Describe the MCL. ***
|
- broad, flat and attaches to medial condyles of femur and tibia and medial meniscus
- (thus MCL damage will probably cause meniscus damage) - provides medial-lateral stability, and becomes taut with extension |
|
|
Describe the LCL. ***
|
- cord-like and attaches lateral femoral condyle to fibular head
- provides medial-lateral stability, and becomes taut with extension |
|
|
Describe the IT band. ***
|
- formed with fibers from gluteus maximus & TFL proximally
- attaches at lateral aspect of proximal tibia, patella - reinforces anterolateral knee - resists or checks excessive motions at knee |
|
|
How many bursae in the knee region? ***
|
13
|
|
|
List the three bursae that communicate with the knee joint capsule. ***
|
- suprapatellar bursa
- subpopliteal bursa - gastrocnemius bursa |
|
|
Location and function of suprapatellar bursa ***
|
- between quadriceps and femur
- reduces extensive friction produced between the many muscles, tendons, ligaments, and bones in knee region |
|
|
Location and function of subpopliteal bursa ***
|
- between popliteus tendon and lateral femoral condyle
- reduce extensive friction produced between the many muscles, tendons, ligaments, and bones in knee region |
|
|
Location and function of gastrocnemius bursa ***
|
- between medial gastrocnemius tendon and medial femoral condyle
- reduce extensive friction produced between the many muscles, tendons, ligaments, and bones in knee region |
|
|
Motions of the tibiofemoral joint ***
|
- sagittal plane, frontal axis
- flexion/extension - 0 to130/160 degrees—must have 0 to walk properly - transverse plane, longitudinal axis - medial-lateral rotation - greatest with knee flexion 90 degrees -also: - anterior-posterior excursion and - abduction/adduction (varus/valgus) movements (neither of these are considered functional movements) |
|
|
Limits on motion of the tibiofemoral joint ***
|
- flexion/extension can be limited with passive insufficiency of multijoint muscles crossing joint
- hip extension/knee flexion (passive insufficiency of knee extensors limits knee flexion) or - hip flexion/knee extension (passive insufficiency of knee flexors limits knee extension) (hamstrings, rectus femoris, sartorius, TFL, and gracilis) - medial/lateral rotation occurs during flexion/extension of knee - amount of rotation is dependent on amount of flexion/extension - increased rotation with knee flexion; no rotation with full extension |
|
|
How many degrees of extension are needed at the tibiofemoral joint for the patient to walk properly? ***
|
must be able to extend to 0 degrees
|
|
|
Describe the locking mechanism of the knee. ***
|
- a.k.a. "screw home mechanism"
during flexion/extension, rotation occurs at tibiofemoral joint because: - articulating surface of medial femoral condyle is longer than that of lateral femoral condyle - as knee extends from flexion, lateral femoral condyle completes the articulation, but - but approximately ½ inch of medial condyle is left - in order to complete articulation with medial condyle, femur rotates medially on tibia during last few (10-15) degrees of extension, and knee “locks” - to unlock knee for flexion, femur laterally rotates on tibia - all of the above occur with closed chain activity; in reverse for open chain (tibia rotates laterally on femur, vice femur rotating medially on tibia) |
|
|
Another name for the locking mechanism of the knee. ***
|
"screw home mechanism"
|
|
|
Plain and simple description of tibofemoral rotation during CKC and OKC movement.
|
- when you stand, the femur rotates medially and
- when you sit it rotates laterally; - when you do a leg extension, the tibia rotates laterally and - when you do a leg curl, the tibia rotates medially) |
|
|
If a therapist is working with a patient lacking the tibiofemoral locking mechanism ("screw home mechanism"), what must the therapist do to enable the patient to complete full ROM at the tibiofemoral joint? ***
|
the therapist will have to manually rotate the tibia laterally on the femur to achieve full ROM (OKC knee extension)
|
|
|
Restrictions in ROM at what other joints can affect knee ROM? How? ***
|
- hip and ankle
e.g., - decreased dorsiflexion results in increased knee flexion from heel raise and toe off to heel strike (have to bend knee more to clear foot and make contact again) - increased hip flexion (contracture) results in increased knee (and ankle) flexion while standing (have to semi-squat to compensate for loss of ROM at hip) |
|
|
What is the close packed position of the knee? ***
|
extension
|
|
|
Describe tibial torsion ***
|
- rotation of the tibia laterally or medially
- lateral torsion = toe out - medial torsion = toe in |
|
|
What is the normal torsion range for the tibia and femur? ***
|
- normal lateral tibial torsion of 7- 10 degrees
- normal medial femoral torsion of 12 degrees |
|
|
If excess torsion is present in the LE, how can one distinguish whether it is tibial torsion or femoral torsion (anteversion)? ***
|
- look at the patellae
- tibial torsion will likely present as in-toeing, but with the patellae normally oriented - femoral torsion (anteversion) will likely present as in-toeing, but also with the patellae internally oriented/rotated |
|
|
At the knee,
- genu valgum and - genu varum are more commonly known as: |
- knock knees
- bowed legs |
|
|
What is the mechanical axis of the LE? ***
|
- line of weight-bearing forces from hip to ground
- normally measures approximately 180 degrees - femur may be angled off 5-10 degrees (making it 185-190 degrees), ---- if more (> 195 degrees), genu valgum (knock knees) ---- if less (< 180 degrees), genu varum (bowed legs) |
|
|
Genu valgum (knock knees) is typically associated with what other alignment issue? ***
|
coxa vara
|
|
|
What structural issues can be caused by genu valgum and/or coxa vara? ***
|
- increased compression forces on lateral tibial condyle
- increased tensile forces on medial structures (e.g., MCL) |
|
|
Genu varum (bowed legs) is typically associated with what other alignment issue? ***
|
coxa valga
|
|
|
What structural issues can be caused by genu varum and/or coxa valga? ***
|
- increased compression forces on medial tibia
- increased tensile forces on lateral structures (e.g., LCL) - patient will also have a tight IT band |
|
|
Constant overloading of medial or lateral soft tissues due to genu valga/coxa vara or genu vara/coxa valga can result in: ***
|
- creep
- which can lead to irreversible damage to articular cartilage, contralateral ligaments and the joint capsule |
|
|
What is genu recurvatum? ***
|
- excessive hyperextension of the knee
- a.k.a. "back knee" - result of “hanging on (Y) ligaments” |
|
|
Describe the structure and function of the patellofemoral joint. ***
|
- synovial, modified plane joint
- enclosed in same capsule as tibiofemoral joint - patella articulates with patellar surface of femur, creating the least congruent joint in the body - vertical ridge of patella aligns with central groove of femur (intercondylar groove) - glides superior and inferior - tilts on longitudinal axis medially and laterally (wouldn't medial-lateral tilt be along anterio-posterior axis??) - rotates medially and laterally (this would be longitudinal axis) - during knee extension and flexion movement of patella superiorly/inferiorly, some rotation and tilting to accommodate asymmetry of femoral condyles |
|
|
What is the least congruent joint in the body? ***
|
patellofemoral joint
|
|
|
What is the largest sesamoid bone in the body? ***
|
patella
|
|
|
Describe the patella. ***
|
- largest sesamoid bone in the body
- posterior articulating surface covered with hyaline cartilage (thickest of any articulating surface in the body) - receives the quadriceps tendon and attaches quadriceps to tibial tuberosity via patellar ligament - position of patella in relation to femur is dependent on length of patellar ligament |
|
|
What articulating surface has the thickest layer of hyaline cartilage in the body? ***
|
the posterior surface of the patella
|
|
|
What are the functions of the patella and patellofemoral joint? ***
|
patella:
- decreases friction between quadriceps tendon and femur - protects knee joint - increases the mechanical advantage for pull of quadriceps by serving as an anatomical pulley - lifts quad tendon away from axis of motion of joint thus increasing moment arm and mechanical advantage - removal of patella results in up to 50% decrease in muscle force of quadriceps (book has 25%) |
|
|
Describe the joint reaction forces at the patellofemoral joint. ***
|
- quadriceps tendon and patellar tendon pull on patella in opposite directions during knee movement
---- knee extension decreases forces; patella is suspended between the two and there are no compressive forces on femur ---- knee flexion increases compressive forces between patella and femur due to the oblique lines of pull of tendons |
|
|
Describe the compressive forces at the patellofemoral joint with knee flexion. ***
|
- walking = .5 X body weight
- squats = 7 - 8 X BW - deep knee bends (> 130 degrees) = compressive forces at patellofemoral joint at approximately 7.8 X body weight |
|
|
How would limited motion at the patellofemoral joint affect the tibiofemoral joint? ***
|
- limitations of motion of patellofemoral joint will decrease tibiofemoral ROM
|
|
|
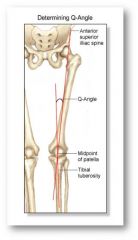
Describe the Q angle. What is its normal range? ***
|
- formed between the line of pull of the quadriceps and the line of pull of patellar ligament
- results in a slight lateral pull of the patella during knee extension - used to detect patellar misalignment, abnormal tracking - measured from ---- ASIS to center of patella (stationary arm) ---- tibial tuberosity to center of patella (movable arm) - normal angle approx 13-18 degrees (book says 10-20 degrees) - this reflects normal genu valga of the knee - the larger the Q-angle or genu valgum, the larger the lateral pull on the patella (the nearly vertical pull of the stronger vastus lateralis shifts ever more laterally, increasingly competing with/overpowering the offsetting pull of the VMO) |
|
|
How is the patella stabilized in the femoral sulcus? What can happen if this balance is upset? ***
|
- stabilization of patella within the femoral sulcus is maintained by passive and dynamic muscle/ligament forces inferiorly/superiorly and medially/laterally
- this normally creates a slight lateral force pull on the patella during extension of the knee - imbalance in forces can change movement of the patella and upset the stability of the knee joint |
|
|
Who has the larger Q angle, males or females? How does this affect patellar tracking? ***
|
females have a larger angle; therefore increased lateral tracking
|
|
|
What pathologies can affect the Q angle and patellar tracking? How? ***
|
- IR of femur
- weak ERs - weak abductors - overpronated feet - tibial torsion - when the Q angle is abnormally increased (20 degrees), increased lateral pull on patella occurs - predisposes patella to pathological changes - increases compressive forces on lateral facet of patella and predisposes to dislocation of patella |
|
|
How are the toes oriented to work the VMO? ***
|
turn toes out to work VMOs
(I have no idea why I have this written down......) |
|
|
Name the knee flexors. ***
|
- knee flexors (posterior knee region)
- seven muscles flex the knee (but adductors can flex it too, depending on position) ---- hamstrings (semimembranosus, semitendinosus, biceps femoris-both heads) ---- sartorius ---- gracilis ---- popliteus ---- gastrocnemius ---- plantaris - most of these also internally or externally rotate the knee |
|
|
Describe the location and actions of the hamstrings. ***
|
- 2-joint muscles
- cross hip and knee joint (except short head of biceps femoris) actions: - extend hip - flex knee - rotate knee - tilt pelvis posteriorly |
|
|
Describe active and passive insufficiency with respect to the hamstrings. ***
|
- active insufficiency: hip extension with knee flexion
- passive insufficiency: hip flexion with knee extension |
|
|
What is important to remember about passive insufficiency? ***
|
the passively insufficient position is a good way to stretch!!
|
|
|
Describe the location and action of the gastrocnemius. ***
|
- 2-joint muscle (crosses knee and ankle joint)
actions: - plantar flexes ankle, - flexes knee (prevents knee hyperextension) |
|
|
Describe the positions of active and passive insufficiency with respect to the gastrocnemius. ***
|
- active insufficiency: ankle plantar flexion with knee flexion
- passive insufficiency: dorsiflexion with knee extension |
|
|
Describe the popliteus and its action. ***
|
- deep to gastrocnemius
- 1-joint muscle - action: medial/lateral rotation of knee - “unlocks” the knee from the "screw home mechanism", initiating knee flexion (unlocks with ER in closed-chain, with IR in open chain) |
|
|
Which muscle is referred to as the "key that unlocks the knee"? Why? ***
|
- popliteus
- because it must engage to initiate knee flexion |
|
|
Describe the sartorius. ***
|
- 2-joint muscle
- potentially a knee flexor/rotator - but more active at the hip with hip flexion, hip abduction, and hip external rotation (FABER) |
|
|
Describe the gracilis. ***
|
- 2-joint muscle
- potentially a knee flexor/rotator but more active as hip adductor |
|
|
What is the pes anserine? ***
|
- located at medial proximal tibia
- insertion for sartorius, gracilis, and semitendinosus (SGT - medial to lateral) |
|
|
What is the popliteal fossa? ***
|
- space behind the knee
- bounded by hamstrings (superiorly), gastrocnemius (inferiorly) - contains arteries and nerves to leg and foot |
|
|
Name the knee extensors. ***
|
quadriceps
- rectus femoris - vastus medialis (longus and oblique) - vastus intermedius - vastus lateralis |
|
|
Which of the knee extensors is a 2-joint muscle? ***
|
rectus femoris
|
|
|
Describe the rectus femoris and its actions. ***
|
- 2-joint muscle that crosses hip and knee
action: - flexes hip - extends the knee - tilts pelvis anteriorly |
|
|
Describe the positions of active and passive insufficiency with respect to the rectus femoris. ***
|
- active insufficiency: hip flexion with knee extension
- passive insufficiency: hip extension with knee flexion |
|
|
Describe the vastus lateralis, vastus intermedius, and vastus medialis and their actions. ***
|
- 1-joint muscles
action: - extend knee |
|
|
What are the two divisions of the vastus medialis? What is special about the VMO? ***
|
- vastus medialis longus (VML)
- vastus medialis oblique (VMO) (strengthen the VMO to counterbalance lateral patellar tracking) |
|
|
Which quadriceps muscle do you strengthen to counter lateral tracking of the patella? ***
|
vastus medialis oblique (VMO)
|
|
|
How do the quadriceps relate to the patella? ***
|
- all four muscles merge into a common quadriceps tendon
- quadriceps tendon attaches to patella and continues distally as patellar tendon - patellar tendon inserts into tibial tuberosity - patella lengthens the mechanical advantage of the quads and - increases ability of quad to generate extension torque during contraction |
|
|
What motions do the quadriceps control during weightbearing movements of LE? ***
|
- during weightbearing of LE quads control
1. knee flexion eccentrically (e.g., sitting down) 2. knee extension concentrically (e.g., standing up) |
|
|
Which are stronger, quadriceps group or hamstring group? ***
|
the quadriceps group is two times stronger than the hamstring group
|
|
|
Name the knee rotators. ***
|
medial rotation (of tibia fixed on femur)
- semitendinosus and semimembranosus - popliteus - gracilis - sartorius lateral rotation - biceps femoris - popliteus |
|
|
What structures stabilize the knee? ***
|
- laterally: ITB, LCL, biceps femoris, popliteus
- medially: MCL, pes anserine, semimembranosus - anteriorly: ACL, quads and patellar tendon - posteriorly: PCL, Hamstrings, gastroc, popliteus - rotation: ACL, PCL |
|
|
Etiology of meniscal tear ***
|
occur as a result of sudden rotation of femur on fixed tibia, most often medial meniscus tear (MMT)
|
|
|
To what types of ligament tears is the knee vulnerable? ***
|
to ligament tears that occur with
- forceful excessive blows to knee or - with low level forces to weakened ligaments ACL/PCL: usually ACL MCL: sudden valgus force to knee |
|
|
What is the "terrible triad" of ligament injury to the knee? ***
|
injury to the
- ACL - MCL - medial meniscus (MMT) |
|
|
To what bursa-related pathologies is the knee vulnerable? ***
|
- bursitis due to excessive friction, compression forces
- commonly seen with prepatellar or infrapatellar bursa - inflammation when on knees a lot (e.g., housemaid's knee) |
|
|
What is a baker's cyst? ***
|
- cyst in popliteal fossa
- caused by herniation of synovial tissue through a weakening in posterior capsular wall - causes calf pain and swelling w/o knee pain |
|
|
What are patellar plicae? ***
|
- folds in the synovial membrane near the patella
- may become pinched under patella during knee flexion, becomes inflamed |
|
|
How does osteoarthritis affect the knee? ***
|
- abnormal stresses lead to degenerative changes in joint cartilage
- leads to exposure of underlying bony surfaces - may require TKR/TKA |
|
|
What is chondromalacia patella? ***
|
- osteochondritis of patella
- abnormal patellar tracking may cause articular surface damage - softening of hyaline cartilage of posterior patella - generally found with misalignment or instability of patella 1. small patella 2. genu valgum 3. muscle imbalance (vastus lateralis > vastus medialis |
|
|
Of what does the ankle and foot complex consist? ***
|
- leg (tibia & fibula)
- ankle - foot |
|
|
To what other structure is the ankle-foot complex analogous? ***
|
to the wrist-hand complex
|
|
|
How many bones and joints comprise the ankle and foot complex? ***
|
- 28 bones
- 25 joints |
|
|
What are the functions of the ankle and foot complex? ***
|
- provides stable base of support for the body during weight bearing
- permits foot to conform to changing and varied terrain - absorbs shock of weightbearing forces through LE |
|
|
What are the characteristics of the tibia? ***
|
- only true weightbearing bone of the leg
- tibial plateau, tibial tuberosity, tibial crest, medial malleolus |
|
|
Which is the only true weight bearing bone of the leg? ***
|
tibia
|
|
|
What are the characteristics of the fibula? ***
|
- lateral to tibia
- head, lateral malleolus |
|
|
Where is the interosseous membrane of the leg located? ***
|
between the tibia and fibula
|
|
|
What are the three functions of the interosseous membrane of the leg? ***
|
- connects tibia and fibula
- provides surface for muscle attachment - unites tibia and fibula to disperse forces |
|
|
Name the tarsal bones of the ankle/foot complex. ***
|

- calcaneus (largest and most posterior)
- talus (sits on calcaneus) - navicular (medial, distal to talus) - cuboid (lateral distal to calcaneus) - cuneiforms (1,2,3) medial to lateral - metatarsals (5) - phalanges (14) |
|
|
Name the three segments of the foot and the bones that comprise them. ***
|
- hindfoot: talus and calcaneus
- midfoot: navicular, cuboid, and cuneiforms - forefoot: metatarsals and phalanges |
|
|
Joint motions and ROM of the ankle/foot: ***
dorsiflexion/plantar flexion inversion/eversion |
dorsiflexion: 20 degrees
plantarflexion: 50 degrees inversion: 20 degrees eversion: 10 degrees (inversion and eversion occur in varying degrees at all of the foot joints) |
|
|
Joint motions and ROM of the ankle/foot: ***
flexion/extension abduction/adduction |
all these occur in the toes
|
|
|
Describe the tibiofibular joints. ***
|
- not part of true ankle joint
- superior and inferior joints - superior joint is plane, synovial with minimal movement - inferior joint (syndesmosis) is fibrous joint, no movement with strong ligaments which offer great stability to ankle joint and maintain snug fit of mortise |
|
|
Is the inferior tibiofibular joint part of the ankle joint? ***
|
no
(even though the fibula comprises the lateral malleolus) |
|
|
Overall strength of the ankle joint is dependent on... ***
|
the strength and stability of the inferior tibiofibular joint
|
|
|
Be able to locate the: ***
- interosseous membrane - anterior inferior tibiofibular ligament - posterior inferior tibiofibular ligament - transverse ligament - posterior talofibular ligament - calcaneofibular ligament |
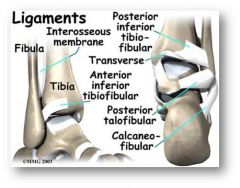
Ligaments of the ankle
|
|
|
Which is the "true" ankle joint? ***
|
talocrural joint
(a.k.a. talotibial joint) articulation of talus with distal tibia and fibula, lateral/medial malleoli |
|
|
Describe the talocrural (talotibial) joint. ***
|
- "true" ankle joint
- articulation of talus with distal tibia and fibula, lateral/medial malleoli - tenon and mortise joint - synovial hinge joint - most congruent joint in body movements: - dorsiflexion - 20 degrees - plantar flexion - 30-50 degrees (book says 60) |
|
|
What is the most congruent joint in the body? ***
|
talocrural (talotibial) joint
|
|
|
Name the ligament groups of the talocrural joint. ***
|
- anterior/posterior tibiofibular ligaments
- deltoid ligament - lateral collateral ligaments |
|
|
Describe the structure and function of the deltoid ligament of the ankle/foot complex. ***
|
- medial side of foot
- group of several ligaments - fan-shaped, extremely strong - from inferior medial malleolus to talus, calcaneous, and navicular bones - strengthen medial ankle joint - hold calcaneous and navicular against talus - helps maintain medial longitudinal arch - protects ankle from eversion injuries |
|
|
Describe the structure and function of the lateral collateral ligament of the ankle/foot complex. ***
|
- three ligamentous bands
- anterior talofibular ligament - calcaneofibular ligament - posterior talofibular ligament - provides lateral support to ankle joint - most frequently injured ankle ligament - majority of ankle injuries are inversion injuries |
|
|
What is the most commonly injured ankle ligament? ***
|
lateral collateral ligament
|
|
|
How are the majority of ankle injuries caused? ***
|
inversion injuries
|
|
|
Describe the structure and function of the subtalar (talocalcaneal) joint. ***
|
- articulation of talus with calcaneus at the rearfoot
- synovial joint, plane (gliding) - movements: primarily supination and pronation components of foot; which allows: - inversion of 0-25 degrees (and adduction) and - eversion of 0-12 degrees (and abduction) - allows adaptation to uneven ground surfaces or cutting laterally or medially while walking or running |
|
|
Other terms for pronation and supination of the foot ***
|
Calcaneovalgus (pronated foot) and calcaneovarus (supinated foot)
|
|
|
Describe the transverse tarsal joint. ***
|
- separates rearfoot from midfoot
- articulation of anterior surface of talus/calcaneous with navicular and cuboid bones - synovial joint, plane - movements inversion/eversion (supination/pronation) - subtalar, talocalcaneonavicular and transverse tarsal joints function interdependently |
|
|
Describe pronation of the foot. ***
|
- movement of talus simultaneously with navicular bone and calcaneus (subtalar)
- functionally subtalar and transverse tarsal joints cannot be separated. - combination of eversion, abduction, and dorsiflexion of any region of the ankle and foot |
|
|
Describe supination of the foot. ***
|
- movement of talus simultaneously with navicular bone and calcaneous (subtalar)
- functionally subtalar and transverse tarsal joints cannot be separated. - combination of inversion, adduction, and plantar flexion of any region of the ankle and foot |
|
|
Describe the MTP joints of the foot. ***
|
- metatarsalphalangeal joints
- articulation of metatarsal heads with bases of phalanges - synovial, condyloid joints - flexion/extension (of toes) - abduction/adduction (of toes) |
|
|
Describe the IP joints of the foot. ***
|
- interphalangeal joints
- articulation between phalanges PIP, DIP joints all toes except great toe (IP only) - synovial hinge joints - flexion/extension |
|
|
Name the 3 plantar arches of the foot ***
|
- medial longitudinal arch
- lateral longitudinal arch - transverse arch |
|
|
Where are the arches of the foot located? ***
|
- in static weightbearing on LE, we stand on a triangle
- base of calcaneous to heads of 1st and 5th metatarsals - between these points are three arches 1. medial longitudinal arch (medial border of foot) 2. lateral longitudinal arch (lateral border of foot normally rests on ground during weightbearing) 3. transverse arch (runs medial-lateral at level of cuneiforms/cuboid) |
|
|
How do the plantar arches of the foot function? ***
|
- on loading the foot, arches flatten
- on unloading the foot, arches recoil to normal shape |
|
|
How are the arches of the foot maintained? ***
|
- shape and arrangement of tarsal bones
- supporting ligaments/plantar aponeurosis - muscles spanning the joints |
|
|
What structures offer the most significant support to the arches? ***
|
Ligaments
- spring ligaments: very strong, support medial arch - long and short plantar ligaments: support lateral arch Other supports - plantar aponeurosis: supports longitudinal arches prevents separation of hindfoot and forefoot - bony structure, peroneus longus tendon, and deep transverse metatarsal ligament support transverse arch |
|
|
Differentiate between a functional flat foot and a structural flat foot. ***
|
- functional flat foot has an arch when NWB, flattens on WB
- structural flat foot is always flat, regardless of WB status |
|
|
What do the arches enable the foot to do? ***
|
- allow foot to absorb shock of weight bearing
- allow foot to accommodate to uneven terrain - allow foot to act as rigid lever to propel body through space during push-off |
|
|
Describe the extrinsic muscles of the ankle and foot complex. ***
|
- proximal attachments on tibia, fibula, and/or interosseous membrane
- multijoint muscles; all cross ankle joint and insert into foot bones - all tendons passing over ankle joint region pass under various retinaculi - prevents “bowstringing” - muscles passing medial and lateral ankle joint give reinforcement to medial and lateral arches, |
|
|
How does muscle location affect ankle/foot action? ***
|
- plantar flexion: muscle crosses posterior to joint axis
- dorsiflexion: muscle crosses anterior to joint axis - inversion: muscle crosses medial to joint axis - eversion: muscle crosses lateral to joint axis |
|
|
Which muscles produce plantar flexion? ***
|
- gastrocnemius
- soleus - plantaris - peroneus longus - peroneus brevis - tibialis posterior - flexor digitorum longus - flexor hallucis longus |
|
|
What muscles comprise the triceps surae? ***
|
- gastrocnemius
- soleus |
|
|
Which plantar flexors merge into the calcaneal/Achilles tendon? ***
|
- gastrocnemius
- soleus - plantaris |
|
|
Which muscles are responsible for 95% of plantar flexion? ***
|
- gastrocnemius
- soleus |
|
|
Describe active insufficiency for the gastrocnemius. ***
|
knee flexion with plantar flexion
|
|
|
Describe passive insufficiency for the gastrocnemius. ***
|
knee extension with dorsiflexion
(good means of stretching this 2-joint muscle) |
|
|
Which muscles perform dorsiflexion? ***
|
- tibialis anterior
- extensor hallucis longus - extensor digitorum longus - peroneus tertius (if present) |
|
|
Which muscles invert the foot? ***
|
- tibialis anterior
- tibialis posterior - gastrocnemius - flexor digitorum longus - flexor hallucis longus |
|
|
Which muscles evert the foot? ***
|
- peroneus longus
- peroneus brevis - extensor digitorum longus |
|
|
When using the wobble board or BAPS* board in trying to strengthen the ankle/foot, what else is affected? ***
* Biomechanical Ankle Platform System |
these not only help strengthen the structures, but also aid in improving proprioception
|
|
|
Describe the intrinsic muscles of the foot. ***
|
- origins/insertions within foot
- movements analogous to muscles in hand - all intrinsics located on plantar surface except extensor digitorum brevis - arranged in four layers with interossei being deepest layer - support arches during dynamic gait activities |
|
|
What are the primary functions of the intrinsic muscles of the foot? ***
|
- toe stabilization
- toe motion (- arch support) |
|
|
What is one means of diagnosing rupture of Achilles tendon? ***
|
observing that the patient cannot walk on his/her toes
|
|
|
What is one means of diagnosing weakness or absence of tibialis anterior? ***
|
observing that the patient cannot walk on his/her heels
|
|
|
What is indicated when a patient is unable to walk on his/her toes? ***
|
possible rupture of Achilles tendon
|
|
|
What is indicated when a patient is unable to walk on his/her heels? ***
|
possible absence of tibialis anterior
|
|
|
What is pes planus? What are two other names for it? ***
|
flat feet
- pes valgus - pronated foot |
|
|
Causes of pes planus ***
|
- excessive medial rotation of leg = abnormal Q angle
- overpronated subtalar joint - stress on/overstretched/weakened plantar ligament = pain (plantar fasciitis) often results in - slight apparent or effective reduction in leg length - hallux valgus - lowering of arch |
|
|
What is pes cavus? What are two other names for it? ***
|
- high arches
- pes varus - supinated foot |
|
|
Describe pes cavus ***
|
- less common than pes planus; but more serious problem
- prohibits joints of foot from participating in shock absorption or adapting to terrain - results in lateral rotation of leg - foot is rigid and cannot disperse forces; weight is borne on metatarsal heads and calcaneus - puts additional strain on ankle joint laterally (more lateral sprains) |
|
|
"Coxa valga" describes: ***
a. the position of the hip when standing with an anterior pelvic tilt b. an angle of inclination significantly greater than 125 degrees c. the position of the hip when standing with a posterior pelvic tilt d. an angle of inclination significantly less than 125 degrees |
b. an angle of inclination significantly greater than 125 degrees
|
|
|
The anterior superior iliac spine is a bony landmark found on the: ***
a. ischium b. proximal femur c. ilium d. pubis |
c. ilium
|
|
|
The iliofemoral, ischiofemoral, and pubofemoral ligaments all limit: ***
a. extension of the hip b. flexion of the hip c. abduction of the hip d. internal rotation of the hip |
a. extension of the hip
|
|
|
Standing with a hip flexion contracture is likely to: ***
a. involve a hyperlordotic posture of the lumbar spine b. involve a posterior pelvic tilt c. over-stretch the iliofemoral ligament d. a and c e. b and c |
a. involve a hyperlordotic posture of the lumbar spine
|
|
|
Which of the following best describes an anterior pelvic tilt? ***
a. short-arc, pelvic-on-femoral hip extension with the trunk remaining essentially upright b. short-arc, pelvic-on-femoral hip flexion with the trunk remaining essentially upright c. an open-chain hip extension motion d. long-arc hip flexion with the trunk moving the same direction as the pelvis |
b. short-arc, pelvic-on-femoral hip flexion with the trunk remaining essentially upright
|
|
|
The normal range of motion for hip flexion is: ***
a. 0 to 90 degrees b. 0 to 50 degrees c. 0 to 30 degrees d. 0 to 120 degrees |
d. 0 to 120 degrees
|
|
|
Which of the following statements is true regarding an individual hiking the right side of the pelvis? ***
a. this motion is produced by active contraction of the right hip abductors b. this motion involves closed-chain abduction of the left hip c. this motion involves activation of the left gluteus medius d. a and c e. b and c |
e. b and c
|
|
|
Which group of muscles is largely innervated by the obturator nerve? ***
a. hip extensors b. hip abductors c. hip adductors d. hip external rotators |
c. hip adductors
|
|
|
Which of the following actions occurs in the horizontal plane? ***
a. hip flexion b. hip internal rotation c. hip abduction d. hip extension |
b. hip internal rotation
|
|
|
Which of the following muscles is a primary hip flexor? ***
a. iliopsoas b. semitendinosus c. piriformis d. gluteus maximus |
a. iliopsoas
|
|
|
Which of the following muscles is involved with the force-couple that produces a posterior pelvic tilt? ***
a. iliopsoas b. gluteus maximus c. rectus abdominis d. a and b e. b and c |
e. b and c
|
|
|
An anterior pelvic tilt involves: ***
a. a force-couple between the gluteus maximus and the erector spinae b. increasing lordosis of the lumbar spine c. decreasing lordosis of the lumbar spine d. strong activation of the hamstring muscles |
b. increasing lordosis of the lumbar spine
|
|
|
If the abdominal muscles are weak, resisted hip flexion will likely result in: ***
a. increased lordosis of the lumbar spine b. decreased lordosis of the lumbar spine c. co-activation of the gluteus maximus d. rupture of the pubofemoral ligament |
a. increased lordosis of the lumbar spine
|
|
|
Which of the following statements is true regarding a posterior pelvic tilt? ***
a. involves increasing lordosis of the lumbar spine b. is performed by a force-couple involving the iliopsoas and the erector spinae c. involves decreasing lordosis of the lumbar spine d. a and b e. b and c |
c. involves decreasing lordosis of the lumbar spine
|
|
|
When the hip is flexed to 70 degrees: ***
a. the gluteus maximus is slackened b. many of the adductors have a favorable line of pull to perform hip extension c. the iliofemoral ligament becomes taut d. the psoas major is maximally elongated |
b. many of the adductors have a favorable line of pull to perform hip extension
|
|
|
When standing only on the right leg, the primary muscles involved in keeping the left side of the pelvis from dropping are the: ***
a. left hip abductors b. right hip abductors c. left hip adductors d. right hip adductors |
b. right hip abductors
|
|
|
If a patient's left hip is arthritic or painful, a clinician would most likely recommend: ***
a. the patient perform heavy resistive exercises with the left leg b. the patient use a cane in the left hand c. the patient perform deep squatting exercises d. the patient use a cane in the right hand |
d. the patient use a cane in the right hand
|
|
|
The right external rotators of the hip are highly involved in which of the following activities? ***
a. planting the right foot and cutting sharply to the left b. planting the left foot and cutting sharply to the right c. strongly adducting the hip across the midline d. flexing the hip past 100 degrees |
a. planting the right foot and cutting sharply to the left
|
|
|
Which of the following is not an action of the gluteus maximus? ***
a. hip extension b. hip external rotation c. posterior pelvic tilt d. hip internal rotation |
d. hip internal rotation
|
|
|
Which of the following statements is true? ***
a. normal range of motion for hip external rotation is 0 to 15 degrees b. normal range of motion for hip extension is 0 to 90 degrees c. normal range of motion for hip abduction is 0 to 40 degrees d. normal range of motion for hip flexion is 0 to 100 degrees |
c. normal range of motion for hip abduction is 0 to 40 degrees
|
|
|
When stretching the iliopsoas muscle, the pelvis must be stabilized to prevent: ***
a. unwanted lordosis of the lumbar spine b. unwanted stretching of the hamstrings c. excessive flattening of the lumbar spine d. activation of the quadriceps muscles |
a. unwanted lordosis of the lumbar spine
|
|
|
An anterior pelvic tilt is a type of hip flexion? ***
a. true b. false |
a. true
|
|
|
During standing at ease, the line of gravity (from body weight) normally travels anterior to the medial-lateral axis of the hip. ***
a. true b. false |
b. false
it travels posterior to the medial-lateral axis of the hip |
|
|
A posterior pelvic tilt is accompanied by decreasing lordosis of the lumbar spine. ***
a. true b. false |
a. true
|
|
|
If a man with osteoarthritis of the right hip must carry a load such as a suitcase, he should carry it on the right side. ***
a. true b. false |
a. true
|
|
|
The rectus femoris is maximally elongated in a position of hip flexion and knee flexion. ***
a. true b. false |
b. false
in a position of hip extension and knee flexion |
|
|
Three of the four hamstring muscles attach proximally to the ischial tuberosity. ***
a. true b. false |
a. true
|
|
|
The hip joint is a condyloid joint allowing 2 degrees of freedom. ***
a. true b. false |
b. false
a ball-in-socket joint allowing 3 degrees of freedom |
|
|
Abduction of the hip occurs about a medial-lateral axis of rotation. ***
a. true b. false |
b. false
about an anterior-posterior axis |
|
|
A positive Trendelenburg sign indicates weakness of the hip adductors. ***
a. true b. false |
b. false
hip abductors |
|
|
Which of the following describes the primary sagittal plane function of the anterior cruciate ligament? ***
a. resists posterior translation of the femur relative to a fixed tibia b. resists anterior translation of the femur relative to a fixed tibia c. resists anterior translation of the tibia relative to a fixed femur d. a and c e. b and c |
d. a and c
|
|
|
Which of the following structures is the distal attachment for all heads of the quadriceps? ***
a. tibial plateau b. tibial tuberosity c. pes anserinus d. lateral epicondyle of the femur |
b. tibial tuberosity
|
|
|
Measured on the lateral side of the knee, normal genu valgum of the knee is typically: ***
a. 30 degrees b. 100 degrees c. 120 to 140 degrees d. 170 to 175 degrees |
d. 170 to 175 degrees
|
|
|
The primary ligament involved in resisting large valgus-producing forces at the knee is the: ***
a. medial collateral ligament b. posterior cruciate ligament c. lateral collateral ligament d. arcuate popliteal ligament |
a. medial collateral ligament
|
|
|
The "terrible triad" describes: ***
a. three primary muscles involved in a hamstring strain b. triangular forces produced during a deep squat c. simultaneous injury of the medial collateral ligament, anterior cruciate ligament, and medial meniscus d. simultaneous activation of the quadriceps, hamstring, and gastrocnemius muscles |
c. simultaneous injury of the medial collateral ligament, anterior cruciate ligament, and medial meniscus
|
|
|
Which of the following statements best describes the function of the medial and lateral menisci of the knee? ***
a. absorb compressive forces between the patella and the femur b. absorb and disperse the compressive forces between the tibia and the femur c. prevent friction between the hamstring muscles and the epicondyles of the femur d. significantly reduce the area of joint contact between the femur and the tibia |
b. absorb and disperse the compressive forces between the tibia and the femur
|
|
|
Which of the following best describes the screw-home mechanism of the knee? ***
a. active extension of the knee causes a superior migration of the patella b. passive flexion of the knee results in an inferior migration of the patella c. an automatic rotation that assists in locking the knee into extension d. simultaneous activation of the medial and lateral hamstring muscles |
c. an automatic rotation that assists in locking the knee into extension
|
|
|
Which of the following muscles is innervated by the femoral nerve? ***
a. biceps femoris--long head b. semitendinosus c. rectus femoris d. a and c e. b and c |
c. rectus femoris
|
|
|
Which of the following muscles is able to perform hip extension and knee flexion? ***
a. semitendinosus b. biceps femoris--long head c. biceps femoris--short head d. a and b e. all of the above |
d. a and b
|
|
|
Which of the following muscles is not associated with the pes anserinus? ***
a. sartorius b. rectus femoris c. gracilis d. semitendinosus |
b. rectus femoris
|
|
|
Which of the following muscles is not innervated by the tibial branch of the sciatic nerve? ***
a. semitendinosus b. biceps femoris--long head c. semimembranosus d. biceps femoris--short head |
d. biceps femoris--short head
|
|
|
A muscle that courses anterior to the medial-lateral axis of rotation of the knee is able to perform: ***
a. knee flexion b. knee extension c. knee internal rotation d. knee external rotation |
b. knee extension
|
|
|
Which of the following statements best describes genu recurvatum? ***
a. internal rotation of the tibia relative to a fixed femur b. a knee that displays marked hyperextension c. a knee that consistently displays a knock-kneed or valgus appearance d. a knee that consistently displays a bow-legged or varus appearance |
b. a knee that displays marked hyperextension
|
|
|
Which of the following statements best describes a function of the patella? ***
a. prevents excessive hyperextension of the knee b. assists the medial hamstrings with internal rotation of the patella c. increases the internal moment arm of the quadriceps, enhancing knee extension torque d. prevents excessive flexion of the knee e. b and d |
c. increases the internal moment arm of the quadriceps, enhancing knee extension torque
|
|
|
Which of the following factors are likely to contribute to excessive lateral tracking of the patella? ***
a. tight iliotibial band or lateral retinaculum b. excessive pronation of the ankle and foot c. weakness of the hip abductors and hip external rotators d. b and c e. all of the above |
e. all of the above
|
|
|
An "extensor lag" is best described as: ***
a. activation of the vastus medialis and vastus lateralis occurring after activation of the rectus femoris b. activation of the quadriceps that occurs after activation of the hamstrings c. inability to complete the final few degrees of knee extension possibly due to swelling within the knee d. extension of the knee occurring after extension of the hip |
c. inability to complete the final few degrees of knee extension possibly due to swelling within the knee
|
|
|
The hamstrings are maximally elongated in a position of: ***
a. hip flexion and knee flexion b. hip extension and knee flexion c. hip flexion and knee extension d. hip extension and knee extension |
c. hip flexion and knee extension
|
|
|
On standing with the knees fully extended, an individual with tight hamstrings is most likely to display: ***
a. a relative anterior pelvic tilt b. a relative posterior pelvic tilt c. genu varum d. genu valgum |
b. a relative posterior pelvic tilt
|
|
|
The rectus femoris remains strong throughout a motion that combines hip flexion with knee flexion because: ***
a. the rectus femoris becomes maximally elongated b. the hamstrings are able to assist with flexing the hip c. the rectus femoris is shortened across the hip but elongated across the knee--maintaining a near-optimal length for producing force d. the vastus medialis and vastus lateralis assist with flexing the hip, whereas the one-joint gluteus maximus assists with flexing the knee |
c. the rectus femoris is shortened across the hip but elongated across the knee--maintaining a near-optimal length for producing force
|
|
|
Which of the following muscles is not multiarticular? ***
a. vastus lateralis b. vastus medialis c. rectus femoris d. a and b e. all of the above are multiarticular muscles |
d. a and b
|
|
|
Which of the following muscles is not considered a quadriceps muscle? ***
a. semimembranosus b. vastus intermedius c. rectus femoris d. vastus lateralis e. a and c |
a. semimembranosus
|
|
|
If the quadriceps are active eccentrically: ***
a. the knee is moving into extension b. the hip is moving into flexion c. the knee is moving into flexion d. the patella is migrating superiorly |
c. the knee is moving into flexion
|
|
|
A large Q-angle can contribute to excessive lateral tracking of the patella. ***
a. true b. false |
a. true
|
|
|
The gastrocnemius muscles have the potential to perform knee extension. ***
a. true b. false |
b. false
knee flexion |
|
|
Active extension of the knee involves a superior migration of the patella. ***
a. true b. false |
a. true
|
|
|
One of the primary functions of the popliteus muscle is to assist in locking the knee. ***
a. true b. false |
b. false
unlocking the knee |
|
|
A deep squat produces more patellofemoral compression force than a shallow squat. ***
a. true b. false |
a. true
|
|
|
The rectus femoris becomes actively insufficient when performing the combined motions of hip flexion and knee extension. ***
a. true b. false |
a. true
|
|
|
One of the primary functions of the posterior cruciate ligament is to resist a posterior translation of the tibia relative to a fixed femur. ***
a. true b. false |
a. true
|
|
|
The medial and lateral collateral ligaments are at less risk of injury with the knee fully extended because they are slackened in knee extension. ***
a. true b. false |
b. false
greater risk |
|
|
What structures comprise the hip joint?
|
- femur
- acetabulum |
|
|
By what two means can hip motion occur?
|
- rotating femur relative to fixed pelvis
- rotating pelvis (and often trunk) relative to fixed femur |
|
|
What are some closed chain movements (rotating pelvis relative to fixed femur) of the hip?
|
- walking/running
- going from standing to sitting and vice versa |
|
|
What is the innominate bone?
|
the pelvis
(means "nameless" in Latin) |
|
|
What structures form the innominate bone?
|
- ilium
- ischium - pubis (on right and left) |
|
|
Where is the greater sciatic notch?
|
between the PIIS and the ischial spine
|
|
|
How is the greater sciatic foramen formed?
|
greater sciatic notch is closed off by the:
- sacrospinous ligament (PIIS to sacrum) and - sacrotuberous ligament (sacrum to ischial tuberosity) |
|
|
What opening is formed by the ischium and pubis?
|
obturator foramen
|
|
|
By what is the obturator foramen covered, and why?
|
- obturator membrane
- so it can serve as attachment point for obturator internus and obturator externus muscles |
|
|
By what is the acetabulum formed?
|
by the joining of the ilium, ischium, and pubis
|
|
|
What is the lunate surface?
|
- the horseshoe-shaped articular superior surface of the acetabulum
- heavily lined with articular cartilage - the only part of the acetabulum that normally contacts the femoral head |
|
|
What is the fovea?
|
a small cup-like depression on the head of the femur
|
|
|
What is the ligamentum teres?
|
- a ligament which connects the fovea at the head of the femur to the transverse acetabular ligament
- contains a branch of the obturator artery |
|
|
What is the linea aspera?
|
- "rough line" in Latin
- a line of slightly raised bone that courses along much of the posterior side of the femur - distal attachment for many adductor muscles and proximal attachment for two quadriceps muscles |
|
|
What is the pectineal line?
|
- distal attachment for the pectineus muscle
- small crest of bone that runs from lesser trochanter to the superior aspect of the linea aspera |
|
|
What is the gluteal tuberosity?
|
- arises from the superior-lateral portion of the linea aspera
- distal attachment for the gluteus maximus |
|
|
What is the adductor tubercle?
|
- raised portion of bone at the medial knee
- distal attachment of the adductor magnus muscle |
|
|
What is the angle of inclination?
|
- frontal plane angle between the neck and shaft of the femur
|
|
|
What is a normal angle of inclination?
|
125 degrees
|
|
|
Why is 125 degrees a normal angle of inclination?
|
it directs the femur toward the midline, which positions the knee joint directly under the weight of the body
|
|
|
What is coxa valga?
Coxa vara? |
- angle of inclination significantly greater than 125 degrees (goes along with genu vara)
- angle of inclination significantly less than 125 degrees (goes along with genu valga) |
|
|
What is femoral torsion?
|
a twist between the shaft and neck of the femur
|
|
|
What is normal anteversion?
|
- the femoral neck projects anteriorly about 15 degrees
|
|
|
How does the hip handle the large forces that routinely cross it?
|
through a system of
- thick articular cartilage - strong muscles - cancellous (spongy) bone |
|
|
What is the transverse acetabular ligament?
|
spans the acetabular notch, completing the "cup" of the acetabulum
|
|
|
What does the obturator artery provide to the femur?
|
some of its blood supply (nourishment)
|
|
|
What is the acetabular labrum?
|
- sharp ring of fibrocartilage that surrounds the outer rim of the acetabulum
- increases stability of hip by deepening the socket and firmly gripping the femoral head - helps seal the joint, providing a partial vacuum for added stability |
|
|
What is the articular cartilage of the hip joint?
|
- covers the lunate surface
- acts as shock absorber within the joint - thickest at superior pole of femoral head where joint pressures are highest during stance phase of gait |
|
|
What is the "Y" ligament?
|
- iliofemoral ligament
- one of the thickest ligaments in the body - attaches to intertrochanteric line of femur (from ilium) - limits hip extension |
|
|
What is the ischiofemoral ligament?
|
- spirals around femoral neck
- attaches near apex of greater trochanter - limits hip extension and internal rotation |
|
|
What is the pubofemoral ligament?
|
- attaches distally to lower half of intertrochanteric line of femur
- limits abduction and extension |
|
|
Why can people stand for prolonged periods of time using minimal muscular energy?
|
- because of the balancing act between the line of gravity at the hip and the ligaments of the hip
- line of gravity passes posterior to the medial-lateral axis of rotation of the hip, providing passive extension torque - ilio/ischio/pubofemoral ligaments of the hip resist extension and offset the pull of gravity |
|
|
How are persons who are paralyzed able to stand using the ligaments of the hip?
|
by using crutches, braces at the knees and ankles, leaning the trunk and pelvis back, and resting on the ligaments of the hip
"hanging on the Ys" |
|
|
What occurs with a hip flexion contracture?
|
- shifts the line of gravity anterior to the medial-lateral axis of the hip
- passive standing mechanism is then disabled, thus hip and back extensor muscles and quadriceps (due to increased lordosis and bent knees) must continuously hold the person upright - compressive forces of weight bearing are directed through structures not designed for dispersing them - muscles then fatigue, causing person to want to sit, perpetuating the cycle (of both hip and knee flexion contractures) - can also damage lumbar facet joints as well as other joints, causing osteoarthritis |
|
|
True or false: Once shortened or contracted, the hip flexor muscles and ligaments of the hip are difficult to re-lengthen.
|
true
|
|
|
What are some methods of preventing hip flexion contractures?
|
- lying prone, if tolerated, or at least flat
- strengthening hip extensors - standing vs sitting - avoid sleeping with pillows under knees - regularly stretch hip flexors |
|
|
What are the three kinematic strategies of motion between the femur and the pelvis?
|
- femoral-on-pelvic motion
- long-arc pelvic-on-femoral motion - short-arc pelvic-on-femoral motion |
|
|
Describe the kinematic strategy of femoral-on-pelvic motion?
|
- open-chain
- femur rotates about relatively fixed pelvis |
|
|
Describe the kinematic strategy of long-arc pelvic-on-femoral motion?
|
- closed-chain
- maximizes ROM of trunk relative to stationary femurs (e.g., bending over to pick something up off the floor) - lumbar spine moves in SAME direction as pelvis |
|
|
Describe the kinematic strategy of short-arc pelvic-on-femoral motion?
|
- closed-chain
- pelvis can rotate in a relatively short arc relative to fixed femur as trunk remains essentially stationary - trunk remains essentially upright and lumbar spine rotates in the opposite direction |
|
|
Describe the difference in movement of the lumbar spine between long-arc and short-arc pelvic-on-femoral motion.
|
- in long-arc pelvic-on-femoral motion, the lumbar spine moves in the SAME direction as the pelvis
- in short-arc pelvic-on-femoral motion, the lumbar spine moves in the OPPOSITE direction of the pelvis |
|
|
Hip flexion
- femoral-on-pelvic - long-arc pelvic-on-femoral - short-arc pelvic-on-femoral |
- femur moves anteriorly, pelvis fixed (knee to chest)
- pelvis rotates anteriorly about stationary femoral heads, with lumbar spine moving in same direction (bending over to touch toes) - pelvis tilts anteriorly, trunk remains relatively upright, lumbar spine moves in opposite direction, increasing lordosis (extending butt to sit down) |
|
|
ROM for hip flexion
- femoral-on-pelvic - short-arc pelvic-on-femoral |
- 0 to 120 degrees
- about 30 degrees |
|
|
Hip extension
- femoral-on-pelvic - long-arc pelvic-on-femoral - short-arc pelvic-on-femoral |
- femur moves posteriorly, pelvis fixed (as if trying to walk backwards)
- pelvis rotates posteriorly about stationary femoral heads, with lumbar spine moving in same direction (arching the back) - pelvis tilts posteriorly, trunk remains relatively upright, lumbar spine moves in opposite direction, decreasing lordosis (rolling hips backward) |
|
|
ROM for hip extension
- femoral-on-pelvic - short-arc pelvic-on-femoral |
- about 20 degrees beyond neutral (limited by tension in ligaments and muscles on anterior side)
- about 15 degrees |
|
|
Hip abduction
- femoral-on-pelvic - long-arc pelvic-on-femoral - short-arc pelvic-on-femoral |
- femur moves away from midline, pelvis fixed (kicking leg out to side)
- lumbar spine and pelvis move in same frontal plane direction (both tip downward), relative to a stationary femur (picking up a suitcase on the side) - downward tilt (abduction) of the hip, trunk remains relatively upright, lumbar spine moves in opposite direction (opposite hip rises = hip hike) |
|
|
ROM for hip abduction
- femoral-on-pelvic - short-arc pelvic-on-femoral |
- 0 to 40 degrees
- about 30 degrees |
|
|
Hip adduction
- femoral-on-pelvic - long-arc pelvic-on-femoral - short-arc pelvic-on-femoral |
- femur moves toward or across midline relative to a fixed pelvis
- lumbar spine and pelvis both rotate away from fixed femur (rare during normal activities; imagine standing on right leg and flexing the body to the left) - upward tilt (adduction) of the hip, trunk remains relatively upright, lumbar spine moves in opposite direction (opposite hip lowers = hip drop) |
|
|
ROM for hip adduction
- femoral-on-pelvic - short-arc pelvic-on-femoral |
- 0 to 25 degrees
- about 25 degrees |
|
|
What is a
- hip hike - hip drop |
- short-arc, pelvic-on-femoral hip abduction
- short-arc, pelvic-on-femoral hip adduction The action is at the contralateral hip in each case - right hip is abducted, left hip is hiked - right hip is adducted, left hip is dropped |
|
|
Hip internal and external rotation
- femoral-on-pelvic - long-arc pelvic-on-femoral - short-arc pelvic-on-femoral |
- femur rotates on fixed pelvis
- with one limb off ground, rotation through the supported hip; trunk follows pelvis in same direction (cutting) - pelvis rotates slightly, trunk remains stationary |
|
|
ROM for hip internal and external rotation
- femoral-on-pelvic - short-arc pelvic-on-femoral |
- 0 to 35 degrees (IR) and 0 to 45 degrees (ER)
- about 15 degrees |
|
|
Arthrokinematics of the hip joint (femoral-on-pelvic motion)
|
roll and slide in opposite directions
|
|
|
What are the two largest nerves of the lumbar plexus?
|
- femoral
- obturator |
|
|
What is the largest nerve in the body?
|
sciatic nerve (of the sciatic plexus)
|
|
|
What two nerves bundled together comprise the sciatic nerve?
|
- tibial
- common peroneal |
|
|
Why are pelvic tilts commonly used to treat the lower back?
|
- they require simultaneous movement of the hips and lumbar spine
- they call the patient's attention to swayback or flatback postures that may, over time, increase the chances of herniated disc, disc damage, overcompressed facet joints, or lower back pain - help reduce exaggerated postures |
|
|
Another name for:
- swayback - flatback |
- hyperlordotic
- hypolordotic |
|
|
Muscles innervated by the femoral nerve:
|
- rectus femoris
- vastus medialis - vastus intermedius - vastus lateralis - sartorius |
|
|
Muscles innervated by the obturator nerve:
|
- adductor magnus (adductor head)
- adductor longus - adductor brevis - pectineus - gracilis - obturator externus |
|
|
Muscles innervated by the sciatic nerve (tibial part):
|
- biceps femoris (long head)
- semitendinosus - semimembranosus - adductor magnus (extensor head) |
|
|
Muscles innervated by the superior gluteal nerve:
|
- gluteus medius
- gluteus minimus - tensor fascia lata |
|
|
Muscles innervated by the inferior gluteal nerve:
|
- gluteus maximus
|
|
|
Nerve to the piriformis innervates:
|
the piriformis
|
|
|
Nerve to the obturator internus innervates:
|
- obturator internus
- gemellus superior |
|
|
Nerve to the quadratus femoris innervates:
|
- quadratus femoris
- gemellus inferior |
|
|
From what plexus do the superior and inferior gluteal nerves originate?
|
sacral plexus
(along with the nerves to the piriformis, obturator internus, and quadratus femoris) |
|
|
From where do the nerves to the piriformis, obturator internus, and quadratus femoris originate?
|
sacral plexus
(along with the superior and inferior gluteal nerves) |
|
|
Name the primary hip flexors
|
- iliopsoas (iliacus and psoas major)
- rectus femoris - sartorius - TFL |
|
|
Any muscle with the potential to flex the hip has the same potential to....
|
anteriorly tilt the pelvis (closed chain)
|
|
|
Which is the body's most powerful hip flexor?
|
iliopsoas
|
|
|
Which is the only muscle of the quadriceps group that crosses both the knee and hip joints?
|
rectus femoris
(it flexes the hip and extends the knee, thus the position of the knee influences the function of the rectus femoris at the hip and vice versa) |
|
|
What is the pes anserius?
|
"goose's foot"
the three-pronged appearance of the sartorius, gracilis, and semitendinosus coming together to insert o n the proximal medial tibia |
|
|
What is the longest muscle of the body?
|
sartorius
|
|
|
Describe the function of the sartorius.
|
- crosses anterior to medial-lateral axis of hip
- crosses posterior to medial-lateral axis of the knee - thus is a hip flexor and knee flexor FABER - flexion, abduction, external rotation |
|
|
Where does the IT band originate and insert?
|
- iliac crest
- lateral tubercle of tibia |
|
|
What is the function of the TFL?
|
- hip flexion
- hip abduction - hip internal rotation - tightens IT band to provide increased stability across lateral hip and knee |
|
|
Which muscles act as a force couple to produce anterior pelvic tilt?
|
- iliopsoas
- rectus femoris (hip flexors) - erector spinae |
|
|
Since the hip flexors and erector spinae work as a force couple to produce anterior pelvic tilt, what would tightness in the hip flexors cause?
|
- tightness in the low back
- swayback (excessive thoracic kyphosis with lumbar lordosis |
|
|
Upon what other muscles do the hip flexors depend for stability?
|
- abdominal muscles
|
|
|
When performing a SLR, how will weak abdominal muscles present?
|
- pelvis will tilt anteriorly (and back will arch) because rectus abdominis cannot counteract the large forces generated by the extended leg
|
|
|
What is the Thomas test used for and how is it performed?
|
- used to check for tight hip flexors
- pt holds non-tested hip and knee fully flexed to keep from cheating with anterior pelvic tilt and lumbar lordosis - pt then attempts to lower other leg to the mat, if the pt cannot make contact with the mat, the hip flexors are considered tight |
|
|
Excessive lumbar lordosis is often a clinical sign of...
|
weak abdominal muscles
(or tight hip flexors) |
|
|
To successfully elevate the leg in a SLR, the hip flexors must produce a force that likely exceeds ___ times the weight of the leg.
|
10
|
|
|
Name the primary hip extensors.
|
- gluteus maximus
- biceps femoris (long head) - semitendinosus - semimembranosus - adductor magnus--extensor head |
|
|
What muscle may be used as a knee extensor in patients with knee extensor paralysis or who lack true knee extensors due to amputation?
|
gluteus maximus can perform the last 20-30 degrees of knee extension by pulling the femur back with the foot firmly in contact with the ground
|
|
|
What is the most easily palpated, superficial structure on the posterior-medial aspect of the knee? What can one do to make it even easier to find?
|
- semitendinosus tendon
- resisted knee flexion |
|
|
Describe the heads of the biceps femoris.
|
- long head is a traditional hamstring that crosses both hip and knee joints
- short head crosses only the knee |
|
|
What is the most easily palpated, superficial structure on the posterior-lateral aspect of the knee? What can one do to make it even easier to find?
|
- biceps femoris tendon
- resisted knee flexion |
|
|
The semitendinosus and semimembranosus are sometimes together referred to as:
|
the medial hamstrings
|
|
|
Which muscles act as a force couple to produce posterior pelvic tilt?
|
- hip extensors (gluteus maximus and hamstrings)
- trunk flexors/abdominals (rectus abdominis and external obliques) |
|
|
What type of pelvic tilt is commonly used to address low-back problems?
|
posterior pelvic tilt (to counteract the lordosis typically associated with low-back pain)
|
|
|
How do the hip extensors get assistance from the hip flexors in generating large forces?
|
- large extension forces are generally required just as the hip has cycled through full flexion
- this puts a quick stretch on the extensors, increasing their tension and putting them at a more favorable length to generate large forces - additionally, many hip adductor muscles which are capable of producing hip flexion in anatomic position become capable of producing hip extension when the hip is flexed (line of pull passes from anterior to the axis of rotation to posterior to it) |
|
|
How do multiarticular muscles like the hamstrings stay strong throughout their entire ROM?
|
for the hamstring
- in a squat, they are tight over the hip but slack across the knee - on standing, they are slack across the hip but tight over the knee - this ability to assume the appropriate length-tension relationship and minimize the rate and amount of contraction preserves the muscle's force-generating ability |
|
|
Name the primary hip abductors.
|
- gluteus medius
- gluteus minimus - TFL (secondary are - piriformis - sartorius - superior fibers of gluteus maximus) |
|
|
When is the most demand placed on the hip abductors?
|
- when walking
- holding the pelvis steady in stance phase while the opposite limb is in swing phase |
|
|
Which is the largest hip abductor muscle?
|
gluteus medius
(occupies about 60% of the total abductor muscle cross-sectional area) |
|
|
What other motions, besides abduction, does the gluteus medius assist in?
|
- anterior fibers assist with flexion and internal rotation
- posterior fibers assist with extension and external rotation |
|
|
To hold the pelvis steady, the hip abduction force and internal moment arm must exceed...
|
the hip adduction force produced by body weight and the external moment arm
[since the internal moment arm is half that of the external moment arm, the hip abductors must generate a force 2X body weight to maintain equilibrium (level pelvis)] |
|
|
What is Trendelenburg sign? How does it manifest?
|
- the classic indicator of hip abductor weakness
- pt stands on one leg (the weaker side); if the pelvis drops toward unsupported leg, positive Trendelenburg sign |
|
|
What does the therapist have to watch for when checking for Trendelenburg sign?
|
that the patient is not leaning toward the weakened stance leg, thereby shortening the external moment arm and reducing the hip abductor force needed to keep the pelvis level
|
|
|
When a patient leans to the side of a weakened hip during gait it is called:
|
- gluteus medius limp or
- compensated Trendelenburg gait |
|
|
The combination of the hip abductor force and the body weight force produces joint reaction forces of...
|
up to three times body weight
(hip abductor force needs to be at least 2X body weight, and body weight is 1X body weight = total of at least 3X body weight; if the pelvis is kept level, that is) |
|
|
How are the hip abduction forces beneficial to the joint? Detrimental?
|
- in a healthy joint, the hip abduction forces help stabilize the joint and provide nutrition to the articular cartilage
- in a person with OA or hip pain, the forces can aggravate the joint and lead to further inflammation and degeneration |
|
|
What are some principles of hip joint protection?
|
- use a cane in the hand opposite the affected hip
- lose excess body weight - walk slowly - correct faulty postures, such as hip flexion contractures - maintain relative flexibility of muscles about the hip and lower back - avoid carrying heavy loads, especially one-handed loads on the side opposite the painful hip (it seems counterintuitive, but a heavy suitcase would be carried on the side of the affected hip) - avoid excessive bending or standing on one limb |
|
|
Why is a cane held in the hand opposite an injured hip?
|
- the cane force (which acts upward b/c the earth returns the same pushing force as applied downward by the hand) has a very long moment arm and produces a torque in the same direction as the joint's hip abduction force
- this allows the hip abductor force and cane force (and their moment arms) to combine to counteract the external torque of the body weight and its moment arm - the pelvis can then be kept level with less force - theoretically, a cane force of only 10% of body weight can reduce hip joint force by about 50% in single-limb support |
|
|
Name the primary hip adductors.
|
- gracilis
- pectineus - adductor longus - adductor brevis - adductor magnus (both heads) |
|
|
Which hip adductor attaches to the femur at the most proximal point?
|
pectineus
|
|
|
Which is one of the most superficial adductor muscles?
|
adductor longus
|
|
|
What are the two heads of the adductor magnus?
|
- posterior head (extensor) - similar to the hamstrings in innervation (sciatic nerve), hip extension ability, and proximal attachments
- anterior head (adductor) - similar to the adductor brevis in innervation (obturator nerve), hip flexion ability, and proximal attachments both are primary adductors of the hip |
|
|
How would the hip adductor muscles work together in dribbling a soccer ball (as in fig 9-32 on pg 265)?
|
- bilateral cooperation
- left adductor magnus contracts in closed-chain, pelvic-on-femoral adduction, producing hip drop on the contralateral side - right pectineus, adductor brevis, adductor longus contract in open-chain, femoral-on-pelvic adduction, accelerating the right LE toward the midline |
|
|
All the hip adductors less one can function as either hip flexors or hip extensors. How is this possible? Which one cannot do both?
|
- when the hip is flexed greater than about 50-60 degrees, the line of pull of the adductors falls posterior to the medial-lateral axis of the hip
- when the hip is in an extended position, the line of pull falls anterior to the medial-lateral axis of the hip (so when flexed, they extend; when extended, they flex; this heavy workload may be why they have a high susceptibility to muscle strain during running) - the adductor magnus (posterior/extensor head) only does extension |
|
|
Why does the body have no individual, strong internal rotators at the hip?
|
- because a strong internal rotator needs horizontal fibers/line of pull
- most of the internal rotators of the hip have near-vertical lines of pull and must work together to produce internal rotation |
|
|
How does the angle of the hip affect the internal rotators?
|
- when the hip is flexed, the internal rotator muscles are at a nearly perpendicular orientation and this increases internal torque
- internal rotation torque increases by 50% when the hip is flexed - keep this in mind when performing manual muscle testing |
|
|
What is a typical gait pattern for persons with cerebral palsy?
|
- crouched gait
- hips flexed and externally rotated |
|
|
What is the intercondylar notch of the femur?
|
- located on posterior-inferior aspect of distal femur, separating the medial and lateral condyles
- passageway for the ACL and PCL |
|
|
What is the intercondylar eminence of the tibia?
|
- double-pointed projection of bone separating the medial and lateral condyles of the tibia
- attachment site for the ACL and PCL, as well as the medial and lateral menisci |
|
|
Where does the quadriceps muscle attach to the patella?
|
at the base
|
|
|
Where does the patellar tendon attach to the patella?
|
at the apex (point on the bottom)
|
|
|
Why is the patella at risk for abnormal gliding or subluxation?
|
because it is embedded in the quadriceps tendon (sesamoid) and highly mobile
|
|
|
Despite strong activation of the quadriceps naturally producing a net lateral pull on the patella, what factors keeps the patella on track?
|
- the steep slope of the lateral facet of the femur and matching patellar surface
|
|
|
Functions of the patellofemoral joint
|
- protect delicate structures of the knee
- improve moment arm for quadriceps, increasing torque-producing potential |
|
|
What is normal genu valgum?
|
170 to 175 degrees
this is the angle between the femur and tibia, caused by the angle of inclination of the femur (normal 125 degrees) and the approximately vertical orientation of the tibia |
|
|
What is excessive genu valgum? Genu varum?
|
- lateral angle less than 170 degrees (goes with coxa vara)
- lateral angle greater than 180 degrees (goes with coxa valga) |
|
|
Knee stabilizers?
|
- ACL
- PCL - MCL - LCL - menisci |
|
|
ACL and PCL protect against...
|
large anterior-posterior shear forces
|
|
|
ACL is susceptible to:
PCL is susceptible to: |
ACL susceptible to:
- hyperextension - large valgus- or varus-producing forces with foot planted - either of the preceding combined with large torsional force at knee PCL is less frequently injured, but susceptible to: - hyperflexion - fall directly on the proximal tibia of bent knee ("dashboard injury") - severe hyperextension - large valgus- or varus-producing forces with foot planted - any of the above along with large torsional force at the knee - may also be ruptured along with ACL |
|
|
How are ACL/PCL injuries typically repaired?
|
- usually requires surgery
- replace torn ligament with tendon from another muscle (autograft) or cadaver (allograft) |
|
|
Function of ACL:
Function of PCL: |
ACL function:
- resist anterior translation of tibia relative to fixed femur (open chain) - resist posterior translation of femur relative to fixed tibia (closed chain) - resists extremes of knee extension - resists valgus and varus deformations - resists excessive horizontal plane rotations PCL function: - resists posterior translation of tibia relative to fixed femur (open chain) - resists anterior translation of femur relative to fixed tibia (closed chain) - resists extremes of knee flexion - resists valgus and varus deformations and excessive horizontal plane rotations |
|
|
Function of MCL:
Function of LCL: |
MCL function:
- resists valgus deformation of the knee - resists excessive knee extension LCL function: - resists varus deformation of the knee - resists excessive knee extension |
|
|
MCL is susceptible to:
LCL is susceptible to: |
MCL susceptible to:
- valgus-producing force with foot planted - severe hyperextension of the knee LCL susceptible to: - varus-producing force with foot planted - severe hyperextension of the knee |
|
|
Function of posterior capsule:
Function of medial and lateral menisci: |
Posterior capsule function
- resists excessive knee extension Menisci function: - improve overall congruency of the tibiofemoral joint - dissipate compression and shear forces across the knee |
|
|
Posterior capsule is susceptible to:
Menisci are susceptible to: |
Posterior capsule is susceptible to:
- severe hyperextension Menisci are susceptible to: - extreme valgus- or varus-producing forces at the knee - extreme rotations of the knee, especially under large compression forces |
|
|
Why is full active knee extension avoided after ACL reconstruction?
|
- pt usually limited from active or forceful knee extension from 40 degrees of flexion through full extension
- activation of quadriceps at these ranges produces anterior shear forces that pull tibia anterior relative to femur (the exact motion the ACL is designed to prevent) - movements to promote co-contraction of muscles surrounding the knee are encouraged - therapist must watch for complications such as increased pain, swelling, instability, as well as prolonged atrophy within the quadriceps |
|
|
Where does the LCL attach on the tibia?
|
- it doesn't, it attaches to the lateral epicondyle of the femur and the head of the fibula
|
|
|
Why do the MCL and LCL become taut at full extension?
|
- to help lock the extended knee
- allows periodic rest for the quadriceps |
|
|
Why are the MCL and LCL more susceptible to injury when the knee is at full extension?
|
at full extension the MCL and LCL are taut and are thus much closer to the rupture point at the time of impact
|
|
|
While walking, compressive forces at the knee routinely reach:
|
2-3 times body weight
|
|
|
What ligaments make up the posterior capsule of the knee?
|
- arcuate popliteal ligament
- oblique popliteal ligament |
|
|
How well do menisci heal?
|
- outer 1/3 - good blood supply, may heal without surgery
- middle 1/3 - poor blood supply - inner 1/3 - essentially avascular - not likely to heal well |
|
|
ROM at the knee for
- flexion/extension - internal/external rotation |
- flexion - 0 - 140 degrees
- extension 0 - 5 degrees hyperextension - IR - 0 - 15 degrees (with knee flexed) - ER - 0 - 30 degrees (with knee flexed) - and it is the same, whether open-chain or closed-chain |
|
|
Roll and slide arthrokinematics of the knee:
- open- chain - closed-chain |
- open-chain: roll and slide in same direction due to concave tibia rolling on convex femoral condyles
- closed-chain: roll and slide in opposite direction due to convex femoral condyles rolling on concave tibia |
|
|
Is the medial-lateral axis of rotation of the knee fixed?
|
- no, it migrates slightly with knee movement
- thus if a pt is in a knee brace it may "piston" slightly as the knee flexes and extends; the therapist must be aware of this and monitor for abrasions or other signs of discomfort |
|
|
Muscles of the knee are innervated by which 3 nerves?
|
- femoral
- sciatic (tibial and peroneal branches) - obturator |
|
|
What can happen with laceration or damage to the femoral nerve?
|
as it is the sole source of innervation to the quadriceps, damage can result in complete paralysis of the knee extensor muscles
|
|
|
Muscles innervated by the sciatic nerve (peroneal portion)
|
- biceps femoris (short head)
|
|
|
Muscles innervated by the tibial nerve
|
- gastrocnemius
- popliteus - plantaris |
|
|
Which muscle is the only true antagonist to the hamstrings?
|
rectus femoris (because it is a hip flexor and knee extensor)
|
|
|
How can one more effectively stretch the rectus femoris?
|
- must work opposite both its actions (i.e., must extend the hip and flex the knee)
- many people allow the pelvis to tilt anteriorly, eliminating the hip extension - activate the abdominals to hold the pelvis in posterior tilt and extend the hip |
|
|
How are the VML and VMO oriented? Why is this important?
|
- VML has a line of pull about 18 degrees off mid-line
- VMO has line of pull about 50-55 degrees off mid-line - the VMO is the only muscle able to effectively counteract the strong, lateral pull of the vastus lateralis on the patella - if these two forces are balanced, result is optimal patellar tracking |
|
|
Which is the largest, strongest muscle of the quadriceps?
|
vastus lateralis
this is what contributes to abnormal tracking or lateral dislocation of the patella |
|
|
How is the patellofemoral joint affected by deep squats?
|
- patellofemoral joint pain (one of the most common clinical conditions of the knee)
- joint is unable to tolerate large compressive forces - the deeper the squat, the further the line of body weight moves posterior to the medial-lateral axis of the knee - to control the squat, quadriceps must be strongly activated, strongly compressing patella into intercondylar groove - vector generated by lines of pull of quadriceps tendon and patellar ligament increases, creating larger joint force |
|
|
Intrinsic factors that can cause excessive lateral tracking of the patella.
|
- imbalance of forces between VMO (weakness) and vastus lateralis (hypertrophy)
- tight IT band or lateral patellar retinaculum - both are firmly attached to lateral aspect of patella - decreased slope of the lateral facet on the intercondylar groove of the femur - lateral facet normally has steep slope that keeps it from gliding too far laterally |
|
|
Extrinsic factors that can cause excessive lateral tracking of the patella.
|
- large Q-angle - malalignment of the hip or ankle creates bowstringing that pulls patella laterally on activation of the quadriceps
- weak external rotators or abductors of the hip - allows femur to adduct and internally rotate, increasing genu valgum of the knee and patella is forced laterally - excessive pronation of the foot - can force tibia medially, increasing valgus and the potential for lateral tracking of the patella |
|
|
What is extensor lag?
|
- after injury/surgery to knee, the quadriceps show considerable difficulty in performing the last 15-20 degrees of active knee extension
- can adversely affect LE function - usually caused by swelling |
|
|
How does extreme tightness of the hamstrings often manifest?
|
- as knee flexion contractures
- however, on standing, the additional stretch placed on the tight hamstrings is transferred proximally and can be expressed as extreme posterior pelvic tilt and flattened lumbar spine - the flattened lumbar spine may over-stretch the connective tissues in the lumbar region, thereby increasing the likelihood of posterior HNP |
|
|
Most functional activities of the LE combine the motions of:
|
- hip flexion and knee flexion
- hip extension and knee extension |
|
|
How do the flexors and extensors of the hip and knee maintain optimal length and force production?
|
e.g., in the push-off phase of running:
- the hip extensor (semitendinosus) actively extends the hip, passively stretching the hip flexor (rectus femoris), while simultaneously - the knee extensor (rectus femoris) actively extends the knee, passively stretching the knee flexor (semitendinosus) - this symbiotic/synergistic relationship keeps either 2-joint muscle from overshortening and becoming actively insufficient; maintains optimal length-tension relationship |
|
|
Internal rotators of the knee
|
- semitendinosus
- semimembranosus - gracilis - sartorius - popliteus - negligible rotation with knee extended, maximal with knee flexed to 90 degrees |
|
|
External rotators of the knee
|
- biceps femoris - long and short heads
- negligible rotation with knee extended, maximal with knee flexed to 90 degrees |
|
|
Which knee rotators dominate--internal or external?
|
the internal rotator muscles of the knee far outweigh the strength of the external rotators
(there are more of them) |
|
|
Bones of rearfoot
|
- calcaneus
- talus |
|
|
Bones of midfoot
|
tarsals
- navicular - cuboid - medial cuneiform - intermediate cuneiform - lateral cuneiform |
|
|
Bones of forefoot
|
- metatarsals
- phalanges |
|
|
What is the gait cycle?
|
- the events that occur (while walking) within two successive heel contacts of the same leg
|
|
|
Each gait cycle is divided into what 2 phases?
|
- stance phase (60%) - foot in contact with the ground
- swing phase (40%) - foot is in the air advancing for the next step |
|
|
Five events of the stance phase:
|
- heel contact/strike
- foot flat - mid stance - heel off - toe off |
|
|
Three events of the swing phase:
|
- early swing
- mid swing - late swing |
|
|
What is the fibular notch?
|
a concave portion of the distal tibia that articulates with the fibula, forming the distal tibiofibular joint
|
|
|
Distal tibiofibular joint
|
- allows a very little gliding motion
- primary function is stable rectangular concavity that accepts the talus to form the talocrural (ankle) joint |
|
|
Tarsal bones
|
- calcaneus
- talus - navicular - cuboid - medial cuneiform - intermediate cuneiform - lateral cuneiform |
|
|
Features of the talus
|
- trochlea - dome-shaped superior portion
- three facets - on plantar aspect for articulation with calcaneus - head - articulates with navicular bone |
|
|
Features of the calcaneus
|
- calcaneal tuberosity - attachment for the Achilles' tendon
- three facets - on superior (dorsal) aspect for articulation with the talus - sustentaculum talus - medial projection of bone that serves as a shelf to support the medial side of the talus |
|
|
Features of the navicular
|
- navicular tuberosity - prominent medial projection of bone; site of distal attachment for the spring ligament and tibialis
|
|
|
Features of medial, intermediate, and lateral cuneiforms
|
form the medial half of the transverse arch of the foot
|
|
|
Features of the cuboid
|
forms the lateral half of the transverse arch of the foot
|
|
|
Features of the metatarsals
|
all 5 consist of
- base - proximal aspect - shaft - convex head - distal aspect |
|
|
Features of the phalanges
|
each of the 14 is composed of
- concave base - shaft - convex head |
|
|
Proximal joints of the ankle/foot:
|
- talocrural
- subtalar - transverse tarsal |
|
|
Distal joints of the ankle/foot
|
- tarsometatarsal (TMT)
- metatarsophalangeal (MTP) - interphalangeal (IP, PIP, DIP) |
|
|
Fundamental movements of the ankle/foot
|
those in the planes which we've already discussed (sagittal, frontal, horizontal)
|
|
|
Applied movements of ankle/foot
|
- those movements that do not fall neatly into one of the cardinal planes
- pronation or supination |
|
|
Distal joints of the ankle/foot
|
- tarsometatarsal (TMT)
- metatarsophalangeal (MTP) - interphalangeal (IP, PIP, DIP) |
|
|
Applied movements of ankle/foot
|
- those movements that do not fall neatly into one of the cardinal planes
- pronation or supination |
|
|
Inversion of the foot
|
turns a point anywhere on the plantar aspect of the foot toward the midline
|
|
|
Eversion of the foot
|
turns a point anywhere on the plantar aspect of the foot away from the midline
|
|
|
Adduction of the foot
|
horizontal plane rotation of the foot toward the midline
|
|
|
Abduction of the foot
|
horizontal plane rotation of the foot away from the midline
|
|
|
Applied motion - pronation
|
combined movement that includes:
- eversion - abduction - dorsiflexion of any region of the ankle and foot |
|
|
Applied motion - supination
|
combined movement that includes:
- inversion - adduction - plantar flexion of any region of the ankle and foot |
|
|
Where do the specialized movements (applied motion) of pronation and supination of the ankle/foot occur most regularly?
|
at the
- subtalar and - transverse tarsal joints |
|
|
Talocrural joint
- articulation - features |
- trochlea of the talus articulates with the rigid concavity formed by the distal tibia and fibula
- primarily designed for dorsiflexion and plantar flexion - the primary joint of the distal leg that allows a forward progression of the body while walking - joint resembles a carpenter's mortise |
|
|
Subtalar joint
- articulation - features |
- composed of the articulation between the three inferior facets of the talus and the matching superior facets of the calcaneus
- designed primarily to permit an arc of motion that combines inversion/adduction and eversion/abduction - during the stance phase this joint allows the lower leg to rotate slightly within frontal and horizontal planes, independent of the fixed calcaneus - effective subtalar joint motion requires the trochlea of the talus remains mechanically stable within the mortise shape of the talocrural joint |
|
|
Transverse tarsal joint
- articulation - features |
- consists of 2 articulations: talonavicular joint and calcaneocuboid joint
- designed to allow motions that cut through all three planes (i.e., allows the most pure form of pronation and supination) - allows the midfoot to move independently of the rearfoot - greatly enhances the overall kinematic versatility of the foot |
|
|
Tarsometatarsal joint
- articulation - features |
- formed by the articulation between the distal surfaces of the three cuneiforms and cuboid with the bases of all 5 metatarsals
- the relatively flattened joint surfaces allow a variety of adaptive motions - the second ray functions as a stable central longitudinal pillar throughout the foot - junction between midfoot and forefoot - allows dorsiflexion and plantar flexion (primarily at the first joint) |
|
|
Metatarsophalangeal joint
- articulation - features |
- formed by the articulation between the convex metatarsal head and the concave base of each corresponding phalanx
designed to allow 2 degrees of freedom: - flexion (0-35 degrees) - extension (0-65 degrees) and - abduction-adduction (limited range) - about 60-65 (up to 85) degrees of hyperextension are required at the first MTP joint during push-off phase of walking |
|
|
Interphalangeal joints
- articulation - features |
- formed by articulations between the convex head of the more proximal phalanx and concave base of the more distal phalanx
- designed to allow extension (typically limited to 0-degree/neutral position) and flexion (up to 70 degrees) only - first toe has only 1 IP joint; other 4 digits have PIPs and DIPs |
|
|
What factors contribute to the stability of the talocrural joint?
|
- tight, rectangular fit of the talus in the mortise
- support of numerous collateral ligaments and muscles - strength of distal tibiofibular joint |
|
|
Supporting structures of the talocrural joint
|
- interosseous membrane
- anterior and posterior tibiofibular ligaments - deltoid ligament (MCL) ---- tibionavicular fibers ---- tibiocacaneal fibers ---- tibiotalar fibers - lateral collateral ligaments ---- anterior talofibular ---- calcaneofibular ---- posterior talofibular |
|
|
Normal ROM for
- dorsiflexion - plantar flexion |
- 0 to 20 degrees
- 0 to 50 degrees |
|
|
Injury to which ligaments is often involved with a "high ankle" sprain?
|
- anterior tibiofibular ligament
- posterior tibiofibular ligament |
|
|
Function of the
- deltoid ligament - lateral collateral ligaments |
- limits eversion
- limit inversion |
|
|
Which of the ligaments of the ankle is most frequently injured?
|
- the anterior talofibular ligament
(of the lateral collateral ligaments, b/c most ankle sprains are due to inversion) |
|
|
Arthrokinematics of the talocrural joint
|
- OKC - roll and slide of convex trochlea in concave mortise is in opposite directions
- CKC - roll and slide of concave mortise over convex trochlea is in the same direction |
|
|
In what position is the ankle most stable (close-packed)? Why?
|
- full dorsiflexion
- because most of the collateral ligaments and all plantar flexor muscles are stretched, and the wider anterior part of the trochlea is wedged into the mortise |
|
|
From a functional perspective, why does wearing high heels predispose one to ankle sprains?
|
- because the shoe places the ankle into a weight-bearing status while plantar flexed
- in this open-packed position, all the plantar flexor muscles and most of the collateral ligaments are slack, and the narrower (and less stable) portion of the trochlea is in the mortise |
|
|
What is the primary shock absorbing structure of the foot?
|
medial longitudinal arch (instep)
|
|
|
Plantar fascia/aponeurosis
- location - function |
- base of calcaneus to proximal phalanges
- absorbs body weight as it supports the height of the medial longitudinal arch |
|
|
How does a person compensate for pes planus? What other difficulties could this cause?
|
- person must rely on intrinsic and extrinsic muscles of the foot to support the arch
- muscles may be overtaxed, possibly leading to fatigue, heel spurs, and other inflammatory conditions (e.g., plantar fasciitis) |
|
|
How does the medial longitudinal arch function during gait?
|
- as the primary dynamic shock absorber
- gives slightly during early stance so foot can gradually accept body weight (as part of this mechanism, the subtalar joint everts slightly as well) - above movements are controlled by eccentric activation of the inverter muscles (tibialis anterior/posterior) for slow and controlled descent - in later stance phase the arch rises and subtalar joint inverts to combine with the stabilizing force of dorsiflexion to accept the strong activation of the plantar flexors during push off |
|
|
Extrinsic muscles of the foot and ankle
- compartments - innervation |
- anterior, lateral, and posterior compartments
- each innervated by a different nerve, each arising from the sciatic nerve |
|
|
Muscles innervated by deep peroneal nerve:
|
muscles in the anterior compartment--primarily dorsiflexors
- tibialis anterior - extensor digitorum longus - extensor hallucis longus - peroneus tertius (if present) |
|
|
Muscles innervated by superficial peroneal nerve:
|
muscles in the lateral compartment--primarily plantar flexors/everters
- peroneus longus - peroneus brevis |
|
|
Muscles innervated by the tibial nerve:
|
muscles in the posterior compartment--primarily plantar flexors/inverters
- gastrocnemius - soleus - plantaris - tibialis posterior - flexor digitorum longus - flexor hallucis longus |
|
|
Is the extensor hallucis longus an invertor or evertor?
|
neither
it courses parallel to the axis of rotation at the subtalar joint so it doesn't pull either way, just simply dorsiflexes |
|
|
If a patient has weakness of the anterior tibialis, with which muscle may they try to compensate?
|
extensor digitorum longus
they may use it to dorsiflex |
|
|
Tightness, spasticity, or overuse of the extensor digitorum longus may result in....
|
"claw toe" deformity of toes 2-5 (hyperextension of the MTP and flexion of the PIP and DIP joints)
|
|
|
Two important functions of dorsiflexors during gait
|
- to elevate the foot to clear the ground in swing phase
- to eccentrically lower the foot during early stance phase (between heel strike and foot flat) |
|
|
Injury to the deep peroneal nerve can cause
|
weakness or paralysis of the dorsiflexors, resulting in:
- foot drop - foot drops into plantar flexion during swing phase (compensated for by high-stepping), or - foot slap - unable to lower foot eccentrically, so it quickly "slaps" to the ground after heel strike |
|
|
Shin splints
- descriptioin - cause - treatment |
- painful condition that may affect muscles that attach to medial and posterior tibia, usually dorsiflexors
- during running, dorsiflexors must repeatedly shift from concentric activation (lifting foot) to eccentric activation (lowering foot); if weak, they may become inflamed through overuse - excessive pronation may worsen the condition because the dorsiflexors are repeatedly activated in an overstretched position - treated with orthotics for support, rest, ice, ultrasound, therapeutic taping |
|
|
How does the peroneus longus maintain its line of pull?
|
using the lateral malleolus and a groove in the cuboid as biomechanical pulleys to produce plantar flexion and eversion
|
|
|
Which muscle is frequently involved with an avulsion fracture of the styloid process of the 5th metatarsal? How?
|
- peroneus brevis
- "dancer's fracture" - strong contraction of the peroneus brevis in an attempt to catch oneself during an excessive (and often unexpected) inversion of the ankle/foot - may also rupture several of the lateral collateral ligaments |
|
|
Function of peroneus longus and brevis in gait
|
- offset the inverting pull of the plantar flexor muscles (most of which invert the foot)
- help maintain lateral stability, especially during late stance phase as heel rises in preparation for push-off |
|
|
Superficial group of the posterior compartment
|
- gastrocnemius
- soleus - plantaris |
|
|
Deep group of the posterior compartment
|
- tibialis posterior
- flexor digitorum longus - flexor hallucis longus |
|
|
Why are the lateral collateral ligaments of the ankle sprained far more often than the deltoid ligaments?
|
- size - LCL is relatively thin, while the deltoid is strong, thick, and wide
- inversion bias - available motion into inversion at the subtalar joint is twice that of eversion (25 degrees vice 12 degrees) - lack of quick response from supporting musculature - peroneal muscles are the best designed to react to excessive inversion, however most sprains occur before they can respond; this is where proprioceptive training with wobble boards, trampolines, BAPS boards, etc. and dynamic balance activities can help train them to react more quickly |
|
|
Which of the calf muscles is a "pure" plantar flexor?
|
soleus
|
|
|
Muscular composition of the soleus
|
- mostly slow-twitch fibers
- makes it ideally suited for activities requiring low forces over a long duration (e.g., standing or controlling postural sway) |
|
|
Muscular composition of the gastrocnemius
|
- more fast-twitch fibers
- make it better equipped to perform more explosive activities such as sprinting and jumping - these explosive activities combine plantar flexion with knee extension, a combination of motions that prevents over-shortening of this 2-joint muscle (as the gastrocnemius shortens to produce plantar flexion, it is stretched across the extending knee, maintaining it's ability to effectively produce force) |
|
|
Why is it relatively easy to rise up on tiptoe?
|
- largely due to the large moment arm available to the gastrocnemius
- on rising, the axis of rotation switches from the talocrural joint to the MTP joints, greatly increasing the moment arm available to the muscle - the internal moment arm is about 3X longer, thus someone weighing 180 lbs would only require 60 lbs of plantar flexion force to rise up on tiptoes (but the center of gravity of the body will be elevated only 1/3 the distance that the muscle contracts) |
|
|
What other role can the soleus have in closed-chain plantar flexion?
|
- knee extensor
- persons with weak quadriceps may be able to use this function as an alternative source of knee extension |
|
|
What issues can an over-active (spastic) soleus cause?
|
- excessive, undesired extension of the knee while bearing weight through lower limb
- can cause genu recurvatum as weight is placed over the leg - seen often in stroke patients |
|
|
Which is the foot's most effective inverter of the subtalar joint and supinator at the transverse tarsal joint? Why?
|
- tibialis posterior
- the extensive distal attachments (every tarsal bone except talus, bases of metatarsals 2-4) |
|
|
What is the relationship between the tibialis posterior and medial longitudinal arch of the foot? What happens if the tibialis posterior tendon ruptures?
|
- supports the arch
- ruptured tendon often causes traumatic pes planus |
|
|
Function of the flexor hallucis longus
|
- highly active during end stage of push-off, when great toe is hyperextended
- generates force that creates friction between plantar surfaces of the toes and the walking surface |
|
|
What is turf toe?
|
- result of traumatic hyperextension of the MTP joint of great toe
- surrounding capsule may become torn and base of great toe becomes swollen and painful - treated with rest, ice, NSAIDs and and rigid plate in sole of shoe to prevent unwanted extension |
|
|
Deep group of the posterior compartment* are the primary ______ of the foot.
(*tibialis posterior, flexor hallucis longus, and flexor digitorum longus |
- invertors or supinators
- most often used eccentrically to resist eversion or pronation during early stance phase |
|
|
When are the intrinsic muscles of the foot most active?
|
- during push-off phase
- contract as a group to help reinforce the relatively raised position of the medial longitudinal arch - stabilize the foot just at the time the plantar flexor muscles contract for push-off |
|
|
What is the sole intrinsic muscle of the dorsum of the foot? What is its function?
|
- extensor digitorum brevis
- extension of the toes |
|
|
How many layers of intrinsic muscles cover the plantar aspect of the foot? What comprises the outermost layer?
|
- 4
- plantar fascia |
|
|
First layer of intrinsic muscles of the foot
|
- flexor digitorum brevis
- abductor hallucis - abductor digiti minimi - all innervated by medial plantar nerve |
|
|
Second layer of intrinsic muscles of the foot
|
- quadratus plantae
- 4 lumbricals - innervated by lateral plantar nerve except lumbrical to 2nd toe (medial plantar) |
|
|
Third layer of intrinsic muscles of the foot
|
- adductor hallucis
- flexor hallucis brevis - flexor digiti minimi - innervated by lateral plantar nerve except flexor hallucis brevis (medial plantar) |
|
|
Fourth layer of intrinsic muscles of the foot
|
- 4 dorsal interossei
- 3 plantar interossei - all innervated by lateral plantar nerve |

