![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
580 Cards in this Set
- Front
- Back
|
What is heredity? ***
|
the innate capacity of an individual to develop traits and characteristics possessed by ancestors
|
|
|
What attributes are included in heredity? ***
|
among other things:
- mannerisms - appearance - intellect - also includes diseases |
|
|
Upon what does heredity depend? ***
|
upon the presence of genes in the chromosomes of the fertilized ovum from which the individual develops
|
|
|
How many diseases are caused by genetic defects? ***
|
between 2,400 and 5,000
|
|
|
What are the different types of genetic defects? ***
|
- single-gene mutation (environmental)
- multifactoral inheritance - chromosomal aberrations |
|
|
Describe a chromosome. ***
|
- rod-shaped organelles seen in dividing cells
- composed of tightly packed deoxyribonucleic acid (DNA) - arranged in a series of individual units called genes |
|
|
Approximately how many genes are contained in one cell? ***
|
100,000
|
|
|
How are chromosomes arranged within the cell? ***
|
each cell (except sperm/egg) contains 46 chromosomes divided into 23 pairs
half of the 46 chromosomes come from each parent (ovum = 23, sperm = 23) 22 of the chromosomes are called autosomes X and Y are sex chromosomes |
|
|
Which is a cause of genetic defects? ***
a. single gene mutation b. autosomes c. traits and characteristics d. organelles |
a. single gene mutation
|
|
|
What sex chromosomes indicate a male? A female? ***
|
XY = male
XX = female |
|
|
What is the karotype of a cell? ***
|
the complete chromosomal composition of the nucleus of a cell
|
|
|
The gene is the basic ______ ___ _________. ***
|
unit of heredity
|
|
|
Each gene occupies a certain _______ ___ ____ __________. ***
|
locus on the chromosome
|
|
|
Hereditary traits are controlled by ______ ___ ________. ***
|
pairs of genes
|
|
|
What are the three mechanisms of transmission of human traits (inheritance)? ***
|
- autosomal dominant
- autosomal recessive - sex-linked inheritance |
|
|
What is an autosomal dominant trait?
|
a gene carried by one parent that is dominant over its paired gene from the other parent
|
|
|
Each child has a ___% chance of inheritance if an autosomal dominant trait is passed on by only one parent. ***
|
50 percent
|
|
|
What are some examples of autosomal dominant traits? ***
|
- brown eyes (over other colors)
- Huntington's chorea - polydactylism - achondroplasia/achondroplastic dwarfism - Marfan syndrome - familial hypercholesterolemia - male pattern baldness |
|
|
What is Huntington's disease? ***
|
autosomal dominant trait
a rare inherited disease that begins in middle life characterized by progressive dementia and slow, writhing hand and arm movements generally terminal within 10-15 years of diagnosis |
|
|
What is achondroplastic dwarfism? ***
|
autosomal dominant trait
cartilage formation in the fetus is abnormal long bones are shorter than normal, but trunk is normal, head is large and forehead is prominent |
|
|
What is polydactylism? ***
|
autosomal dominant trait
having extra fingers or toes |
|
|
What is an autosomal recessive trait? ***
|
a gene trait inherited from both parents
(parents do not exhibit trait) |
|
|
How are offspring affected by autosomal recessive genes? ***
|
children of two parent carriers of autosomal recessive gene have:
- 25% chance of having the disease - 50% chance of being a carrier of the disease - 25% chance of being unaffected by the disease |
|
|
What are some examples of autosomal recessive disorders? ***
|
- phenylketonuria (PKU)
- sickle cell anemia - cystic fibrosis - galactosemia - Tay-Sachs - albinism |
|
|
What is phenylketonuria? ***
|
autosomal recessive disorder
lack of a specific enzyme which results in a high level of the amino acid phenylaline in the body phenylaline is toxic to the brain and may cause mental retardation, convulsions, poor balance, tremors, hyperactivity child presents with blonde hair and light skin, because the phenylalanine isn't converted to tyrosine, which is needed for melanin pigment production |
|
|
What is sickle-cell anemia? ***
|
autosomal recessive disorder
a disease that is predominant in black families (1 in 12 are carriers!) characterized by abnormal hemoglobin with deformed (sickle-shaped) red blood cells these cells may become lodged in small arterioles and capillaries and block circulation, leading to necrosis and infarcts or death of tissue; the defective red blood cells are removed by the spleen, and this depletion can result in severe anemia oddly, heterozygous carriers, although mildly anemic, have increased resistance to malaria because of the sickle cell trait |
|
|
What is cystic fibrosis? ***
|
autosomal recessive disorder
a disease that affects the exocrine glands, resulting in thick mucus which obstructs intestinal glands, pancreas, and bronchi sweat contains excessive sodium and chloride, which aids in diagnosis |
|
|
What is the cause of cystic fibrosis? ***
|
a faulty chromosome number 7
|
|
|
What is galactosemia? ***
|
autosomal recessive disorder
inborn inability to utilize the sugar galactose, which accumulates in the blood and causes infant failure to thrive, cirrhosis of the liver, and mental retardation treatment consists of eliminating galactose from the diet |
|
|
What is Tay-Sachs disease? ***
|
autosomal recessive disorder
a disorder of lipid metabolism that causes excessive accumulation of lipids in the brain leads to blindness, mental retardation, and infant death primarily affects families of Eastern Jewish (Ashkenazi) origin |
|
|
Tay-Sachs disease, Cystic Fibrosis, Sickle Cell anemia, and Galctosemia are due to gene traits inherited from: ***
a. father b. mother c. grandparents d. both parents |
d. both parents
|
|
|
What is a sex-linked inheritance? ***
|
a defective gene on the X chromosome (because Y chromosome is small and carries few genes)
typically the abnormalities are transmitted by the female, but affect the male offspring recessive gene on the single X-chromosome of a male is unmasked and the trait is expressed (so, although it is recessive, in males it sort of acts dominant) female XX generally negates the trait, but renders a 50% chance of being a carrier and passing on the trait; will only have the disease if she inherits two defective X chromosomes male only transmits the disorder to daughters, because the Y chromosome is normal, and the male contributes only the Y chromosome to males |
|
|
What are some examples of sex-linked inheritance? ***
|
- color blindness
- hemophilia - Duchenne muscular dystrophy - night blindness - ichthyosis |
|
|
What is color blindness? ***
|
sex-linked inheritance
cannot distinguish between colors, usually red-green |
|
|
What is hemophilia? ***
|
sex-linked inheritance
disorder of the intrinsic coagulation mechanism hemophilia a - absence of clotting factor viii hemophilia b - absence of clotting factor ix; affects young males, who may have severe hemorrhage, or joint inflammation leading to arthritic destruction of joints |
|
|
What is Duchenne muscular dystrophy? ***
|
sex-linked inheritance
affects almost exclusively boys (1 in 3,500) and appears between the ages of 3 and 5 characterized by lack of dystrophyn in sarcolemma; progressive skeletal muscle deterioration (very rapid) Gower's sign--walking up thighs to stand--a sign of potential Duchenne's MD |
|
|
What is ichthyosis? ***
|
sex-linked inheritance
problem with keratinization results in scaly, lizard-like skin |
|
|
How do gross chomosomal abnormalities occur? ***
|
- either in structure or number of chromosomes
- cells may fail to separate properly during cell division, causing one deficient daughter cell and one daughter cell with an extra chromsosome - loss of autosomal chromosome is usually incompatible with life - loss of a sex chromosome or presence of an extra one is less serious, but still produces abnormalities |
|
|
What are some examples of gross chromosomal abnormalities? ***
|
- Down's syndrome
- Fragile X syndrome - Cri du chat syndrome |
|
|
What are the characteristics of Down's syndrome? ***
|
gross chomosomal abnormality
three chromosomes 21 (trisomy), because of the failure of two chromosomes to separate as gametes are being formed (nondisjunction) children have wide-set eyes with epicanthic folds, a course protruding tongue, a straight crease across the palm and a shortened 5th finger mental retardation, and may have congenital heart disease and frequent respiratory infections |
|
|
What are the characteristics of Fragile X syndrome? ***
|
gross chomosomal abnormality carried by females
abnormality of X chromosome causes physical and mental disability Fragile X chromosome appears to have broken end and affects connections in the brain similar to autism, child presents with eye avoidance, unexplained temper tantrums, flapping hands and arms, large head with long face and pronounced ears, hyperactivity, distractability, and impulsivity as well as sensory integration dysfunctions |
|
|
What is Cri du chat syndrome? ***
|
gross chomosomal abnormality caused by deletion of part of the short arm of chromosome 5
child presents with abnormally small head and deficiency in cerebral brain tissue, widely spaced yes and mental retardation makes cat-like crying sounds |
|
|
What are some sex anomalies? ***
|
- Turner syndrome - missing sex chromosome (XO)
- Klinefelter syndrome - extra sex chromosome - hermaphrodite - has both testes and ovaries - pseudohermaphrodite - has either testes or ovaries, but rest of anatomy is mixed (a.k.a. sex reversal since the chromosomal sex differs from anatomical sex) |
|
|
What is the complete, detailed family history drawn up by a genetic counselor called? ***
|
pedigree
|
|
|
How are pedigrees used? ***
|
to determine patterns of inheritance of a genetic disease within the family
can assist a couple in deciding if the risks of having genetically abnormal offspring are significant enough for them to decide against having children |
|
|
When is amniocentesis done? ***
|
after the 14th week of pregnancy
|
|
|
How many genetic diseases can amniocentesis detect? ***
|
approximately 200
|
|
|
Are the results of amniocentesis always accurate? ***
|
no, false positives are not uncommon
|
|
|
What is chorionic villus sampling? ***
|
removal of cells from the villi through the cervix
gives embryonic or fetal results (gender and chromosomal information) earlier in the pregnancy |
|
|
What is gene therapy (a.k.a. genetic engineering)? ***
|
a procedure that involves identification, manipulation, and transference of genetic segments into a host to replace defective genes and to perform desired genetic activities
it may be cultured in a microbe and delivered in a viral package or by injection (a la "bubble boy") |
|
|
What are congenital diseases? ***
|
diseases which appear at birth or shortly thereafter, but are NOT caused by genetic or chromosomal abnormalities
congenital defects usually result from some failure in development during the embryonic stage, or in the first 2 months of pregnancy CONGENITAL DISEASES CANNOT BE TRANSMITTED TO OFFSPRING! |
|
|
Can congenital diseases be transmitted to offspring? ***
|
no
|
|
|
What is the function of deoxyribonucleic acid (DNA)?
|
it is the blueprint for directing all cell activities, especially protein synthesis within the cell
|
|
|
All genes are made from:
|
segments of four chemical bases (A,T,G,C), arranged in different orders and in different lengths
|
|
|
Within the nucleus of cells, DNA is assembled into stranded units called _________.
|
chromosomes
|
|
|
Describe meiosis.
|
Within each primary sex organ (ovary or testis), "parent" sex cells contain 46 chromosomes and divide to produce gametes (egg and sperm) that each contain 23 chromosomes
|
|
|
44 of 46 chromosomes are called
|
autosomes
|
|
|
Two of the 46 chromosomes are called:
|
X and Y (or sex) chromosomes
|
|
|
What is the Human Genome Project?
|
a 13-year project begun in 1990 that set out to
-identify all of the approximate 30,000 genes in human DNA, - determine the sequences of the 3 billion chemical base pairs that make up human DNA, and - store this information in databases |
|
|
Who sponsored the Human Genome Project?
|
the US Department of Energy and
the National Institutes of Health |
|
|
Genes for a particular trait occupy:
|
a particular site on a chromosome
|
|
|
Each person has ___ sites or ___ copies of each gene.
|
two, two
one copy from each parent |
|
|
What are alleles?
|
alleles are alternative forms of a gene
(e.g., for brown eyes, for blue eyes, for green eyes--they are all eye-color genes, but in different forms/with different characteristics) |
|
|
Define homozygous.
|
the pair of alleles for a particular trait are the same
(e.g., offspring has BB for brown eyes or bb for blue eyes) |
|
|
Define heterozygous.
|
the pair of alleles for a particular trait are different
(e.g., offspring has Bb alleles, one for brown eyes and one for blue eyes) |
|
|
Which alleles always produce their trait when inherited?
|
dominant alleles
|
|
|
How does a dominant allele (B-brown eyes) express itself when the offspring is:
- homozygous (e.g., BB for brown eyes) - heterozygous (e.g., Bb--alleles for both brown eyes and blue eyes)? |
whether homozygous or heterozygous, the dominant allele will be the one expressed
this offspring will have brown eyes |
|
|
When do recessive alleles express themselves?
|
only when the offspring is homozygous for the trait
(e.g., only bb will have blue eyes) |
|
|
What are codominant alleles? Give an example.
|
alleles that, when both are inherited, both traits express themselves
(e.g., AB blood type, A inherited from one parent and B from the other) |
|
|
What is reduced penetrance?
Give an example. |
when a dominant allele is not fully expressed
(e.g., syndactyly) |
|
|
What factors can modify expression of genes?
|
- other genes
- environmental conditions - gender |
|
|
How does an autosomal dominant allele express with respect to:
- different generations - affecting male or female offspring? |
the autosomal dominant disease will appear in every generation
it will affect male and female offspring equally |
|
|
What is the cause of hereditary or familial diseases?
|
they are generally the result of metabolic breakdown caused by a lack of direction from a missing or compromised gene or chromosomal segment
often the gene responsible for the production of a particular protein (e.g., enzyme or structural type) is missing or defective, and this interrupts the chain of events required to ensure proper metabolic activities |
|
|
What is the most common genetic disorder in the US?
|
hemochromatosis
(affects 1 in 200 to 1 in 400 people) |
|
|
How are hereditary or familial genes passed on?
|
when offspring inherits:
- a single autosomal dominant allele - a pair of autosomal recessive alleles (one from each parent) - a defective allele on the X chromosome |
|
|
What is Marfan syndrome?
|
autosomal dominant trait
dysfunction of gene that codes for connective tissue protein fibrillin lack of fibrillin weakens connective tissue, including tendons, heart valves, and blood vessels, thus it's a multisystemic disease affects 1 in 10,000; detected by lack of fibrillin in blood test |
|
|
What is familial hypercholesterolemia?
|
autosomal (incomplete) dominant trait
common cause of cardiovascular disease (affects 1 in 500) mutation in gene encoding receptor for low-density lipoprotein (LDL); results in lipid deposits in arteries and atherosclerosis incomplete dominant, thus varying outcomes - if both genes are mutated - death in childhood - if only one gene is mutated (heterozygous) - death as young adult |
|
|
Autosomal recessive diseases manifest themselves only when:
|
a person is homozygous for the defective allele
requires both parents to be carriers (heterozygous) offspring have 25% chance of having the disease |
|
|
The chance for inheriting two recessive alleles increases in:
|
close intermarriage
|
|
|
What is albinism?
|
autosomal recessive disorder
manifests with very white skin and hair; increased risk of skin cancer often visual problems (nearsightedness and abnormally high light sensitivity) |
|
|
What is the most commonly inherited cause of mental retardation?
|
Fragile X syndrome
|
|
|
What are familial diseases?
Give some examples |
some diseases appear in families, but means of inheritance is not understood
(e.g., diabetes, epilepsy, allergies, cardiovascular problems, familial polyposis) |
|
|
What seems to be the cause of familial diseases?
|
they do not seem to be the result of a single gene, but effect of several genes working together, known as a multifactorial trait
some familial diseases may not be inherited at all, but instead result form unique environmental conditions or behaviors that are shared by family members |
|
|
When is chorionic villus sampling done?
|
in early pregnancy, between the 8th and 10th week
|
|
|
What is atresia?
|
the absence of a normal opening in an organ
|
|
|
A permanent change in the genetic code of DNA is:
|
a mutation
|
|
|
If the two members of a pair of genes are alike, they are said to be:
|
homozygous
|
|
|
Mutations can result from:
a. viral activity b. radiation c. chemical action d. all three answers are correct |
d. all three answers are correct
|
|
|
The carrier of a genetic disease is someone who has a defective gene and:
|
apparently normal health
|
|
|
The carrier of a genetic disease is:
|
heterozygous
|
|
|
Congenital diseases are those that are:
|
present at birth or shortly thereafter
|
|
|
A genetic disease that always appears in the children of one affected parent must be:
|
an autosomal dominant trait
|
|
|
An individual who is heterozygous for a genetic disease but is not him/herself affected is a carrier for a:
a. dominant autosomal trait b. recessive autosomal trait c. recessive sex-linked trait d. answers 2 and 3 are both correct |
d. answers 2 and 3 are both correct
|
|
|
Typical characteristics seen in a Down syndrome child include:
a. mental retardation b. slanted eyes c. coarse and protruding tongue d. all of the above |
d. all of the above
|
|
|
Marfan syndrome is:
a. XXY chromosomes b. sterile male c. dominant trait d. codominant trait |
a dominant trait
|
|
|
DNA provides a blueprint for protein synthesis. (T/F)
|
true
|
|
|
The karyotype of a cell describes the chromosomes present. (T/F)
|
true
|
|
|
Autosomes are the chromosomes that determine the sex of an individual (T/F)
|
false
|
|
|
Inborn errors of metabolism can result from lack of a particular enzyme. (T/F)
|
true
|
|
|
Sex-linked genes are carried on the X and the Y chromosomes. (T/F)
|
false
|
|
|
Girls do not develop sex-linked genetic disorders. (T/F)
|
false
|
|
|
Lactaid may reduce symptoms of galactosemia. (T/F)
|
true
|
|
|
In males, the Y chromosome is shorter than the X but carries the same number of genes. (T/F)
|
false
|
|
|
Color blindness is a sex-linked trait found only in males. (T/F)
|
false
|
|
|
Fathers only contribute the Y sex chromosome to their sons. (T/F)
|
true
|
|
|
If everyone who inherits one copy of a defective allele develops the related disorder, that allele is ________________.
|
dominant
|
|
|
Huntington's chorea is inherited as a ______________ trait.
|
dominant, autosomal
|
|
|
Phenylketonuria is a genetic disorder resulting from the failure of an afflicted individual to produce ___________.
|
an enzyme
|
|
|
The inheritance of __________ may decrease the likelihood of a person's catching malaria.
|
sickle cell trait
|
|
|
People with Turner's syndrome or Klinefelter's syndrome will be __________.
|
sterile
|
|
|
From two color blind parents, there is ______ chance for a normal visioned offspring?
|
0%
|
|
|
The gene for achondroplasia affects development of the fetal __________.
|
cartilage
|
|
|
The lack of control of salt and mucus secretion is indication of __________________.
|
cystic fibrosis
|
|
|
An autosomal recessive condition causing abnormal lipid metabolism in the brain, with progressive mental and physical retardation, and death by the age of 4 is ___________.
|
Tay-Sachs
|
|
|
The incidence of __________ is higher in mothers over the age of 35.
|
Down syndrome
|
|
|
What is malnutrition? ***
|
- any disease or disorder concerning nutrition
- may result from unbalanced, insufficient or excessive diet - may be the result of impaired absorption, assimilation, or use of foods |
|
|
What are the causes of malnutrition? ***
|
- ignorance and poverty
- gastrointestinal disorders - chronic alcoholism - psychoneurotic disorders |
|
|
What are the basic purposes for nutrients? ***
|
- form body structure
- provide energy - serve as regulators of body processes |
|
|
Body structure is determined by: ***
|
genetics
|
|
|
For the genetic blueprint of the body structure to be fulfilled, an individual must have adequate: ***
|
nutrition
|
|
|
What is energy? ***
|
vital function/fuel that nutrients provide the body
|
|
|
How is energy measured? ***
|
it is measured in calories
|
|
|
How many calories do most adults use daily? ***
|
between 1500 and 3000
|
|
|
What are the nutrients that provide energy? ***
|
- carbohydrates
- lipids - proteins |
|
|
What is another term for regulation? ***
|
metabolism
|
|
|
What are the primary nutrient regulators? ***
|
- proteins
- vitamins - minerals |
|
|
What are the symptoms of Vitamin C deficiency?
How is it treated/prevented? *** |
- bleeding gums and hemorrhages into tissues
- citrus fruits and greens |
|
|
What are the symptoms of Vitamin A deficiency?
How is it treated/prevented? *** |
- results in poor vision in dim light; also dry, cracked mucous membranes
- diets including dairy products and vegetables |
|
|
What are the symptoms of Vitamin D deficiency?
How is it treated/prevented? *** |
- weak, deformed bones
- Vitamin D supplements, fortified milk, and exposure to sunlight |
|
|
What are the symptoms of Vitamin K deficiency?
How is it treated/prevented? *** |
- results in tendency to hemorrhage
- normal diet |
|
|
What are the signs and symptoms of Vitamin A hypervitaminosis, both acute and chronic? ***
|
- acute toxicity: headache, vertigo, diarrhea
- chronic toxicity: cirrhotic-like liver, hypercalcemia, and or generalized edema |
|
|
Which are the fat-soluble vitamins? ***
|
- Vitamin A
- Vitamin D - Vitamin E - Vitamin K |
|
|
What are the signs and symptoms of Vitamin D hypervitaminosis, both acute and chronic? ***
|
- acute toxicity: hypercalcemia, weakness, vomiting, diarrhea, nausea
- chronic toxicity: renal impairment, polydipsia, or excessive thirst |
|
|
What are the signs and symptoms of Vitamin E hypervitaminosis? ***
|
- very minimal in humans
|
|
|
What are the signs and symptoms of Vitamin K hypervitaminosis? ***
|
hemolysis--destruction of RBCs with the release of hemoglobin
|
|
|
Which are the water-soluble vitamins? ***
|
- niacin
- vitamin B6 - vitamin C |
|
|
What are the signs and symptoms of niacin toxicity? ***
|
- flushing
- severe twitching - rash - jaundice - heartburn, nausea, vomiting - hypotension, syncope |
|
|
What are the signs and symptoms of vitamin B6 toxicity? ***
|
convulsive disorders
|
|
|
What are the signs and symptoms of vitamin C toxicity? ***
|
- diarrhea
- urinary acidification - neuropathies |
|
|
What are the principal functions of calcium? ***
|
- muscle contraction
- bone formation - blood clotting |
|
|
What is the principal function of iodine? ***
|
thyroid hormone regulation
|
|
|
What are the principal functions of potassium? ***
|
- nerve activity
- heart and muscle functioning |
|
|
What is the principal function of iron? ***
|
hemoglobin formation
|
|
|
What are the principal functions of sodium? ***
|
- water balance
- nerve and muscle activity |
|
|
What is the etiology of anorexia nervosa? ***
|
- a disease of psychoneurotic origin
- aversion to food leads to emaciation and malnutrition - patient is obsessed with food, but desires to be thinner |
|
|
What is the incidence of anorexia nervosa? ***
|
- most common among teenage females
- greatly increased in recent years - rare in males and older population |
|
|
What are the signs and symptoms of anorexia nervosa? ***
|
- patient has misconception of body image and size
- denies problem, but perceives herself as fat - becomes emaciated with gaunt face and protruding bones |
|
|
What personality changes are associated with anorexia nervosa? ***
|
- irritability
- anxiousness - depression - hostility - obsessed with food - exercises strenuously |
|
|
What does a medical exam of an anorexia nervosa patient generally reveal? ***
|
- low blood pressure
- decreased heart rate - anemia - dehydration - depletion of potassium - muscle weakness - heart abnormalities - lowered immune response |
|
|
What is the treatment for anorexia nervosa? ***
|
hospitalization to correct malnutrition and psychological problems
|
|
|
What is the prognosis for anorexia nervosa patient? ***
|
- frequent relapses
- depression leading to suicide - starvation leading to death with a high mortality rate |
|
|
What is the etiology of bulimia? ***
|
an eating disorder of psychoneurotic origin with a gorge-purge syndrome
similar to anorexia, but the goal is to avoid weight gain, not lose weight |
|
|
Who are the primary bulimia patients? ***
|
females in their teens and early 20s
|
|
|
What are the signs and symptoms of bulimia? ***
|
- usually of average weight or slightly overweight, making it hard to detect
- eating binges followed by self-induced vomiting - excessive use of laxatives and diuretics - constant sore throat - swollen salivary glands - dehydration - electrolyte imbalance - liver damage is common |
|
|
What is the treatment for bulimia? ***
|
may include antidepressants and psychological counseling
management rather than cure is the treatment goal |
|
|
What is the prognosis for bulimia? ***
|
can lead to sudden death from heart failure or ruptured stomach
|
|
|
Bulimia may persist: ***
|
throughout life
|
|
|
What is obesity? ***
|
a nutritional disorder that occurs when an abnormal amount of fat accumulates in adipose tissue
|
|
|
What causes obesity? ***
|
it occurs when an excess of calories is consumed compared to energy expended
the rate of fat synthesis is faster than mobilization of fat to muscles for use as energy |
|
|
What may be said about the underlying cause of obesity? ***
|
it may be complex and difficult to treat
|
|
|
At what point is a person considered obese? ***
|
if the individual is 20% heavier than the upper limit of ideal weight for his/her sex, age, and height
(AT LEAST THAT'S WHAT I THINK THE SLIDE IS TRYING TO SAY--CHECK ON THIS!) |
|
|
What are some of the causes of obesity? ***
|
- overeating (high calorie) foods combined with insufficient exercise
- genetic factors; increased number of adipose cells may be inherited trait - culture and environment; encouraging excessive food intake and using food as a reward set the regulatory system of the hypothalamus at a level that maintains the habit of overeating - emotional dependency on food as a reward to self when depressed or lacking positive feelings - hypothalamus dysfunction and hypoactive thyroid are rarely a cause of obesity - psychological factors: reaction to stress, substitute for other desires, learned behavior as a result of environment |
|
|
What are some of the complications of obesity? ***
|
- hypertension
- hypoventilation - maturity-onset diabetes - diaphragmatic hernia - enlarged heart - atherosclerosis - varicose veins - gallbladder disease - fatty liver - psychological disorders - sleep apnea |
|
|
What is the treatment for obesity? ***
|
- diet
- exercise - drugs - surgery |
|
|
What aspects of a diet can help reduce obesity? ***
|
- it is the most effective method of overcoming obesity
- change eating habits (choice and volume) - balanced diet of protein, some unsaturated fat, and adequate carbohydrates to provide glucose to cell (minimizes feeling of hunger) - reduce intake of sodium and table salt - increase daily intake of water - weight reduction programs - provide support for difficult process |
|
|
What is an optimal weekly weight loss goal for lasting results? ***
|
loss of 1-3 pounds
|
|
|
At what calorie levels does weight loss occur for:
men? women? *** |
men - 1500-2000 calories per day
women - 500-1000 calories per day |
|
|
How does an exercise program facilitate weight loss? ***
|
- daily exercise will facilitate weight loss by expending calories
- exercise releases endorphins which will help you feel better - exercise tends to help suppress habitual feelings of hunger |
|
|
What types of drugs are used to assist weight loss? ***
|
- appetite suppressants (depressants) and amphetamines initially assist with new eating habits, but may cause nervousness, restlessness, insomnia, dry mouth, and constipation
- mild antidepressant drugs used if depression is a contributing factor to obesity |
|
|
How can surgery be used to facilitate weight loss? ***
|
- decrease size of intestines
- decrease size of stomach (pouch procedure/gastric bypass) - lap band |
|
|
What are some positive effects of weight loss? ***
|
- decreased blood pressure
- lower levels of circulating lipids that may contribute to atherosclerosis - distress of osteoarthritis is reduced (decreased joint pain, increased mobility) - more effective, efficient control of diabetes - decreased cardiovascular and respiratory problems - increased activity level which helps maintain weight loss - increased self-image - less stressed and greater life satisfaction - increased longevity - sleep apnea reduced |
|
|
What is alcoholism? ***
|
illness characterized by significant impairment that is directly associated with persistent and excessive use of alcohol
|
|
|
What types of impairment are associated with alcoholism? ***
|
impairment may involve physiological, psychological, or social dysfunction
|
|
|
What percentage of alcohol consumers are considered alcoholics? ***
|
in 1995, 10% of alcohol consumers were considered alcoholics, number has increased annually
|
|
|
What psychological problems are noted with alcoholism? ***
|
- emotional disturbances during childhood or past
- feelings of insecurity, inadequacy, or loneliness - hostility - depression |
|
|
What sociological problems are noted with alcoholism? ***
|
- sanctioned behavior - heavy drinking is socially acceptable in some professions or cultures
- peer pressure: social groups consider drinking "adult behavior" - teens and young adults engage in alcohol binges - socially promoted as relaxing and forgetting troubles by having a few drinks |
|
|
What causes alcoholism-related malnutrition? ***
|
- unavailability of required nutrients or skipping meals
- eating unbalanced meals - diseases that prevent the utilization of ingested foods - psychoneurotic disorders |
|
|
What treatment options are available for alcoholism? ***
|
- best controlled by early intervention and continuing attention
- treatment directed toward enabling patient to develop better problem-solving strategies - mental and physical health of alcoholic determines best treatment approach - personal physician, psychotherapist, group therapy, or AA or behavior modification are options - detoxification centers are available for the acutely intoxicated - general and psychiatric hospitals may be required for treatment of DT, hepatic comas, and other medical emergencies - halfway houses and recovery houses are helpful in assisting the recovering alcoholic with adjusting and transitioning to life without alcohol |
|
|
Upon what body systems does alcohol have a negative effect? ***
|
- central nervous system
- digestive system - cardiovascular system |
|
|
What specific effects does chronic alcoholism have on the digestive system? ***
|
- gastritis
- liver disease - pancreatitis - gynecomastia - blood clotting disturbances - ascites (abnormal accumulation of fluid in the abdomen) - ecchymoses (bruising) - epistaxis (nosebleeds) |
|
|
What specific effects does chronic alcoholism have on the cardiovascular system? ***
|
- fatty infiltration of the heart
- coronary thrombi - enlargement of the heart - progressive cardiac failure |
|
|
What specific effects does chronic alcoholism have on the nervous system? ***
|
- impaired judgment
- poor powers of concentration - delirium tremens - hepatic coma |
|
|
What is fetal alcohol syndrome? ***
|
- caused by babies being born to alcoholic mothers
- most likely to occur if mother has a 5-10 year history of drinking problems - incidence is increasing along with the increase in alcoholism among young females |
|
|
What are the signs and symptoms of fetal alcohol syndrome? ***
|
- mental retardation
- delayed physical growth - limb and joint abnormalities - heads are smaller than normal - eye slits smaller and with epicanthal folds - flat midface - nose short and upturned - smooth philtrum and thin upper lip - jaws underdeveloped - born with withdrawal symptoms, stiffness, and irritability |
|
|
What is the treatment for fetal alcohol syndrome? ***
|
detoxification and life support
|
|
|
What is the prognosis for fetal alcohol syndrome? ***
|
good, if near full term or normal birth weight with no other physical abnormalities
|
|
|
What membranes does the heart contain? ***
|
- myocardium - cardiac muscle
- endocardium - smooth membrane lining heart chambers - pericardium - double-membrane sac enclosing heart - epicardium - inner layer of pericardial sac |
|
|
What is the septum of the heart? ***
|
the structure that separates the right and left sides of the heart
(there is an interatrial septum and interventricular septum) |
|
|
List the chambers of the heart. ***
|
2 atria, 2 ventricles
- atria - receiving chambers - ventricles - pumping stations |
|
|
What are the functions of the 2 atria? ***
|
right atrium receives blood from the body (deoxygenated - CO2)
left atrium receives blood from the body (oxygenated - O2) |
|
|
What are the functions of the 2 ventricles? ***
|
right ventricle - pumps blood to lungs (CO2)
left ventricle - pumps blood to the body and brain (O2) |
|
|
What do the heart valves do? ***
|
they assure one-way flow of blood
(the lub-dub sound is their opening and closing) |
|
|
What two types of valves are contained in the human heart? ***
|
- atrioventricular valves
- semilunar valves |
|
|
What are the atrioventricular valves? ***
|
valves between atria and ventricles (duh!)
- bicuspid (mitral) valve is between the left atrium and ventricle - tricuspid valve is between the right atrium and ventricle |
|
|
What is another name for the bicuspid valve? ***
|
mitral valve
|
|
|
What are the semilunar valves? ***
|
- pulmonary valve - between right ventricle and pulmonary artery
- aortic valve - between left ventricle and aorta |
|
|
What is the function of the coronary arteries? ***
|
they supply blood to the muscles of the heart
if the coronary arteries become blocked, the result is heart attack |
|
|
What is the primary function of the human heart? ***
|
- muscular pump
- keeps blood flowing to all cells and tissues |
|
|
Trace the flow of blood through the human heart. ***
|
- deoxygenated blood from inferior and superior vena cava enters right atrium
- flows through tricuspid valve into right ventricle - pumped through pulmonary valve into pulmonary artery, which branches to the left and right lungs - CO2 is exchanged for O2 - oxygenated blood is pumped through pulmonary veins to left atrium - flows through mitral/bicuspid valve into left ventricle - pumped through aortic valve into aorta for distribution to brain and rest of body |
|
|
What is the cardiac cycle? ***
|
alternating contraction and relaxation of atria and ventricles
|
|
|
How many phases are there in the cardiac cycle? What are they? ***
|
two phases
- systole - active, contracting phase - diastole - relaxing, filling with blood period |
|
|
What is the typical speed of the cardiac cycle? (Each cycle and cycles per minute) ***
|
- each cycle takes approximately 0.85 seconds
- roughly 72 cycles per minute |
|
|
How do the ventricles and atria function together? ***
|
when ventricles are alternately contracting, the atria are alternately relaxing and filling
|
|
|
What does blood pressure express? ***
|
ventricular systole/diastole
(contraction/relaxation) BLOOD PRESSURE IS VENTRICULAR!!! |
|
|
The human heart can contract continuously and rhythmically without: ***
|
nerve stimulation
|
|
|
By what mechanism does the heart beat? ***
|
sinoatrial node - specialized patch of tissue on right atrial wall acts as a pacemaker, initiating a beat
impulse travels over right and left atria and causes atrial contraction stimulates atrioventricular node near septum special bundle of fibers (Bundle of His) rapidly spreads impulses from atria to ventricles impulses terminate in Purkinjie fibers which branch throughout ventricles contraction of ventricles occurs |
|
|
Which portion of the nervous system influences heart rate? ***
|
autonomic nervous system
|
|
|
How does the autonomic nervous system influence heart rate? ***
|
via innervation to the heart (cardiac nerves for acceleration, vagus nerve for slowing)
(sinoatrial and atrioventricular nodes) |
|
|
What does the vagus nerve do? ***
|
- causes release of neurotransmitter acetylcholine (ACh) which slows contraction during sleep or rest (parasympathetic nervous system)
- right vagus innervates sinoatrial node |
|
|
What does the cardiac accelerator nerve do? ***
|
causes release of neurotransmitter epinephrine, which speeds up contractions for strenuous physical activity, when excited, or when body needs more blood flow (sympathetic nervous system)
|
|
|
What are some common heart diseases and defects? ***
|
- coronary artery disease (CAD)
- hypertensive disease (HTN) - cor pulmonale - congestive heart failure - congenital heart defects - valvular disorders - rheumatic heart disease - infectious endocarditis - abnormalities of heart action |
|
|
What is coronary artery disease? ***
|
- coronary arteries supplying O2 blood to heart muscles become occluded due to coronary thrombosis (clot) or narrowing of the lumen (atherosclerosis)
- ischemia (deficiency of blood supply) develops, resulting in heart attack - sudden deprivation of blood to myocardium causes tissue death - infarct is the dead muscle tissue, repairs as scar tissue and is no longer functional |
|
|
Another name for a heart attack. ***
|
myocardial infarction
|
|
|
What is the prognosis for a patient suffering a myocardial infarction? ***
|
depends on:
- speed of medical attention/CPR - size of coronary artery occluded - how much heart muscle is damaged - if collateral blood vessels to area are sufficient to lessen damage |
|
|
What are some signs of impending MI? ***
|
- severe chest pain
- heartburn, nausea - clammy feeling - shortness of breath (SOB) - referred pain into left side of neck and/or shoulder, down left upper extremity (LUE) - can also be right-sided pain |
|
|
What are some treatments for a myocardial infarction? ***
|
- thrombolytic drugs and anticoagulants (Coumadin, Heparin, aspirin)
- CABG - LE saphenous vein to replace occluded area - angioplasty to break up plaque - lasers to break up plaque |
|
|
What is angina pectoris? ***
|
temporary O2 deficiency to heart (not > 30 minutes)
|
|
|
What causes angina pectoris? ***
|
- stress
- overexcitation - heavy meals - strenuous exercise |
|
|
What are the signs of angina pectoris? ***
|
severe, sharp chest pains which may radiate to neck, jaw, and left arm, and/or
feeling of tightness or suffocation |
|
|
What is the treatment for angina pectoris? ***
|
nitroglycerin pills to dilate arteries
|
|
|
What is hypertensive heart disease? ***
|
the heart is overworked due to pumping against great resistance (narrowed vessels) because of a history of uncontrolled high blood pressure (150/90 or higher)
the hypertensive heart is enlarged (hypertrophy and dilation) the left ventricle becomes exhausted and the heart fails |
|
|
What are the signs and symptoms of hypertensive heart disease? ***
|
- often asymptomatic for months to years
- vague symptoms of lightheadedness, tinnitus, fatigue, heart palpitations |
|
|
What is the treatment for hypertensive heart disease? ***
|
- minimize risk factors
- diet and moderate exercise - decrease stress - vasodilators and diuretic medications |
|
|
What is cor pulmonale? ***
|
caused by right-sided heart failure due to chronic lung disease
right ventricle works against too much resistance, with resultant dilation and hypertrophy |
|
|
What is the treatment for cor pulmonale? ***
|
relieving causative lung disease by bronchodilators and ventilation
|
|
|
What is the main function of the circulatory system?
|
transport
|
|
|
The circulatory system carries:
|
- oxygen and nutrients needed for metabolism to the tissues
- waste products from cellular metabolism to kidneys and other excretory organs for elimination - electrolytes and hormones needed to regulate various body functions |
|
|
What is considered the pacemaker of the heart?
|
the sinoatrial node (SA node)
|
|
|
What are the two circulatory routes?
|
- systemic circulation
- pulmonary circulation |
|
|
What is the smallest artery called?
|
arteriole
|
|
|
What are capillaries?
What do they do? |
they connect arteries (arterioles) and veins (venules)
deliver oxygen and nutrients to tissues |
|
|
Composition of veins:
|
- thinner walls than companion arteries
- lumens are larger, however - less muscle and elasticity makes them more likely to collapse when empty - have valves to return blood to heart against pull of gravity (esp in legs) |
|
|
What are some diseases of arterial circulation?
|
- hyperlipidemia
- hypercholesterolemia - arteriosclerosis - atherosclerosis - peripheral artery disease - Raynaud's disease - aortic aneurysm |
|
|
What are some diseases of arterial pressure?
|
- arterial hypertension
- pulmonary arterial hypertension |
|
|
What are some diseases of venous circulation?
|
- venous circulation of the lower extremities
- varicose veins - chronic venous insufficiency - venous thrombosis |
|
|
What are some diseases of cardiac function?
|
- coronary heart disease
|
|
|
What are some myocardial and endocardial diseases?
|
- myocarditis
- cardiomyopathy |
|
|
What are some diseases of the endocardium?
|
- infective endocarditis
- rheumatic heart disease |
|
|
What are some valvular heart diseases?
|
- mitral stenosis
- mitral regurgitation - aortic stenosis - aortic regurgitation |
|
|
What are some cardiac conduction disorders?
|
- cardiac arrhythmias
|
|
|
What is congestive heart failure?
|
a condition in which the heart cannot pump enough blood to meet the blood and oxygen needs of other body organs
it is a complication of most forms of heart disease, including coronary and peripheral atherosclerosis |
|
|
What are some heart diseases noted in infants and children?
|
congenital heart disease consisting of:
- cyanotic heart disease (tetrology of fallot, transposition of the great arteries) - non-cyanotic congenital heart disease (septal defects, patent ductus arteriosus, coarctation of the aorta) |
|
|
What general disorders cause heart disease?
|
disorders of
- blood flow - blood pressure - cardiac function |
|
|
What is hyperlipidemia?
|
generic term for elevated lipids or fats in the blood
|
|
|
What are lipids?
|
- cholesterol
- cholesterol esters - phospholipids - triglycerides |
|
|
Cholesterol is transported throughout the system by:
|
transport proteins called lipoproteins
|
|
|
Why is LDL the "bad" cholesterol?
|
accumulations of it form a plaque or thick hard deposit that narrows the arteries and impedes blood flow
|
|
|
Why is high-density lipoprotein (HDL) the "good" cholesterol?
|
it carries about 1/4 to 1/3 of the cholesterol
it carries cholesterol away from the arteries and to the liver, where it is eliminated from the body |
|
|
What are triglycerides?
|
the form that fat exists in the human body
|
|
|
What are the two classifications of hypercholesterolemia?
|
primary - develops independent of other causes
secondary - associated with other health problems or lifestyle |
|
|
Many types of hypercholesterolemia have _____
|
a genetic basis
|
|
|
A cause of primary hypercholesterolemia:
|
familial hypercholesterolemia (an autosomal dominant genetic disorder)
|
|
|
Causes of secondary hypercholesterolemia:
|
- obesity
- diabetes mellitus |
|
|
What does arteriosclerosis lead to? Why?
|
hypertension
because affected arteries cannot stretch and rebound in response to pressure of blood forced through them |
|
|
What is the most common cause of arteriosclerosis?
|
atherosclerosis
|
|
|
What are some risk factors for atherosclerosis?
|
- hypercholesterolemia
- smoking - hypertension - diabetes |
|
|
What are the three types of lesions associated with atherosclerosis?
|
- fatty streak
- fibrous atheromatous plaque - complicated lesion |
|
|
What are fatty streaks?
|
thin, flat discolorations in the vasculature that progressively enlarge and thicken
|
|
|
How do fatty streaks evolve?
|
they are present in children and increase in number to about age 20, then they either remain static or regress
|
|
|
What is the basic lesion of clinical atherosclerosis?
|
the fibrous atheromatous plaque
|
|
|
How is the fibrous atheromatous plaque characterized?
|
by accumulation of intracellular and extracellular lipids and formation of scar tissue
|
|
|
How does fibrous atheromatous plaque begin?
|
as a whitish gray lesion thickening of the vessel intima (inner coat of the vessel) that contains a lipid core covered by a fibrous plaque
as the lesion increases in size, it may cause an occlusion |
|
|
What are complicated lesions?
|
more advanced than fatty streaks or fibrous atheromatous plaque
characterized by hemorrhage, ulceration, and scar tissue deposits |
|
|
How is a thrombosis formed?
|
the clot within a blood vessel is formed by turbulent blood flow in the region of the plaque and ulceration of the plaque
|
|
|
When are symptoms of atherosclerosis felt?
|
not usually until the interior of the artery is extensively occluded
|
|
|
On what do symptoms of atherosclerosis depend?
|
location and severity of occlusion
|
|
|
Occlusion of the coronary arteries may result in:
|
chest pain and shortness of breath
|
|
|
Blockage of the carotid arteries can cause:
|
reduced blood supply to the brain and a stroke
|
|
|
Blockage or hardening of arteries in the leg is known as:
|
peripheral artery disease
(peripheral vascular disease) |
|
|
Peripheral artery disease (peripheral vascular disease) can lead to:
|
pain in the muscles of the leg
in severe cases, ulceration or gangrene of the extremities |
|
|
What medications are used to treat atherosclerosis?
|
- antihypertensive medications
- cholesterol-lowering medications |
|
|
What is peripheral arterial disease?
|
similar diseases as affect coronary or carotid arteries, but in the peripheral arteries of the body
|
|
|
What are the symptoms of peripheral artery disease?
|
- ischemia (lack of blood and oxygen supply); foot will feel cool to touch and pulse will be faint or absent
- pain (esp. with walking - a.k.a. intermittent claudication) - impaired function - infarction - tissue necrosis (ulceration and gangrene) - thinning of skin and subcutaneous tissues of lower leg |
|
|
What arteries are most commonly affected by peripheral artery disease?
|
- femoral
- popliteal |
|
|
What are the signs of ischemia?
|
- subcutaneous atrophy
- pallor - coolness - absent pulse |
|
|
Treatment for peripheral artery disease:
|
- prevention of further damage
- walking slowly - avoiding injury to areas with compromised circulation - blood thinners - surgical bypass/removal |
|
|
Symptoms of Raynaud's disease? ***
|
- skin change from pallor to cyanosis
- cold, numbness, tingling, pain - may lead to arthritis, ulceration, or rarely gangrene |
|
|
How are aneurysms classified?
|
- location
- size - morphology (configuration and structure; e.g., fusiform, saccular) - origin |
|
|
Where do aneurysms usually occur?
|
- abdomen below the kidneys (abdominal aortic aneurysm)
- chest cavity (thoracic aneurysm) - cerebral or brain aneurysms are less common |
|
|
Causes of aneurysms? ***
|
- atherosclerosis (most common for abdominal aneurysms)
- connective tissue disease - congenital defect - infection - inflammation - trauma |
|
|
Treatment of aneurysms? ***
|
possibly surgical repair, depending on size and location
|
|
|
Arterial blood pressure is a measure of:
|
the force of blood against arterial walls
systolic <120 mm Hg diastolic <80 mm Hg |
|
|
What is the cause of congestive heart failure? ***
|
inadequate pumping of the heart
|
|
|
What is chronic congestive heart failure? ***
|
the result of many cardiac and pulmonary pathologies
|
|
|
What is acute congestive heart failure? ***
|
results from myocardial infarction
|
|
|
What becomes congested in congestive heart failure? ***
|
either
- systemic veins or - pulmonary veins pressure builds up in either vascular system |
|
|
What happens in right-sided congestive heart failure? ***
|
- peripheral edema
- pitting edema of ankles - distended neck veins - enlarged liver/spleen because blood is backing up in the vena cava to the rest of the body |
|
|
What happens in left-sided congestive heart failure? ***
|
- pulmonary edema
- shortness of breath because blood is backing up into the lungs |
|
|
What is the treatment for congestive heart failure? ***
|
- diuretics to decrease edema
- reduction of salt and water intake - medications to improve cardiac output - antihypertensives - antiarrhythmics - medications to slow heart rate and allow heart muscle to relax and fill with blood - bed rest in severe cases |
|
|
What are congenital heart defects? ***
|
caused by abnormalities of birth due to failure of normal heart development in utero
|
|
|
What is the most common congenital heart defect? ***
|
most are septal defects--abnormal openings in the septum
|
|
|
What is an ASD? ***
|
atrial septal defect
a defect (opening) in the septum between the two atria |
|
|
What is a VSD? ***
|
ventricular septal defect
a defect (opening) in the septum between the two ventricles |
|
|
What is a PDA? ***
|
patent ductus arteriosis
a defect (opening) connecting the pulmonary artery and aorta |
|
|
What is the Tetralogy of Fallot? ***
|
a collection of four heart abnormalities
|
|
|
How does a ventricular septal defect produce cyanosis? ***
|
- initially the pressure gradient is higher in the left ventricle, so the oxygenated blood flows to the right ventricle (lower pressure)
- pressure in right ventricle increases and deoxygenated blood begins to flow back to left ventricle - deoxygenated blood is pumped out the aorta and to the body, producing cyanosis |
|
|
What abnormalities occur in Tetralogy of Fallot? ***
|
- narrowing of pulmonary artery (decreased size or by valvular stenosis)
- large ventricular septal defect (VSD) - thicker (hypertrophied) right ventricle - displaced aorta that crosses interventricular septum (allows blood from both ventricles into systemic circulation) one of the most serious congenital heart defects |
|
|
What is coarctation of the aorta? ***
|
narrowing or stricture of the aorta, and decreased blood flow to the lower body
|
|
|
What is the usual treatment for congenital heart defects? ***
|
surgical correction
|
|
|
What occurs in patent ductus arteriosis? ***
|
the ductus arteriosis connecting the pulmonary artery and aorta fails to close after birth
higher blood pressure in aorta causes blood to flow backwards into pulmonary artery (lower pressure) |
|
|
What are some types of valvular disorders? ***
|
- stenosis
- valvular insufficiency - malfunctions/defects |
|
|
What is valvular stenosis? ***
|
the opening is too small for sufficient blood flow
(e.g., mitral stenosis due to rheumatic fever--mitral valve cusps become rigid and fuse) |
|
|
What can cause mitral stenosis? ***
|
Rheumatic fever is the predominant cause
blood clots deposit on inflamed mitral valve cusps and they become rigid and fuse, causing stenosis |
|
|
What is valvular insufficiency? ***
|
the valvular opening is too large
e.g., mitral insufficiency - mitral valve cannot close completely due to poor or weak papillary muscle contractions and cusps flutter open (allow backflow) |
|
|
What do valvular disorders result in? ***
|
- decreased blood flow, circulation
- cyanosis - blood backs up and leads to hypertrophy and CHF - thrombus formation leads to emboli to brain or organs |
|
|
What other minor issue can valvular disorders cause? ***
|
a heart murmur, which may be asymptomatic if not a serious problem
|
|
|
How are valvular disorders corrected? ***
|
- surgical reconstruction
- valve replacements |
|
|
What is the cause of rheumatic heart disease? ***
|
- rheumatic fever (a systemic disease)
- sequela of infection by a Group A hemolytic streptococci - autoimmune reaction with antibodies attacking body's tissue, especially the heart/mitral valve |
|
|
What organs/tissues are affected by rheumatic fever? ***
|
- joints
- CNS - skin - heart - mitral valves primarily involved with mitral stenosis and mitral insufficiency |
|
|
Who is primarily affected by rheumatic fever? ***
|
usually children, teens, and young adults
it's uncommon today because of antibiotics |
|
|
What are the signs and symptoms of rheumatic fever? ***
|
- begins with sore throat and ears
- progresses to fever, inflamed and painful joints - sometimes a rash (shiny red swelling of joints -- associated with rheumatic conditions) |
|
|
What is infectious carditis/infective endocarditis? ***
|
- microbial infection affecting endocardial endothelium and heart valves
- bacteria and fungi cause it, and in acute cases form nodules or vegetations in a fibrous clot |
|
|
What are the symptoms of infective endocarditis?
|
- fever
- chills - change in sound or character of an existing heart murmur - evidence for embolization of the vegetative lesions |
|
|
How does infectious carditis/infective endocarditis occur? ***
|
caused by streptococcus bacterium entering bloodstream due to UTI, skin infection or tooth infection, etc.
bacteria migrate to heart already damaged by congenital defect and/or rheumatic heart lesions form bacteria-filled nodules which are friable (break apart easily) and enter bloodstream as emboli to brain/organs |
|
|
What is the treatment and prognosis for infectious carditis/infective endocarditis? ***
|
- blood test for causative organism
- EKG to detect valve disease and vegetations - treatment with antimicrobials - surgical interventions when heart is severely damaged prognosis is good (was fatal prior to antibiotics) |
|
|
What is an arrhythmia? ***
|
loss or irregularity of normal heart rhythm
irregularity in impulse generation and impulse conduction |
|
|
What is a normal heart rate? ***
|
- adults - 72-78 bpm
infants - 110-150 bpm normal rate slows with age |
|
|
What are four types of arrhythmias? ***
|
- heart block
- excitation - atrial fibrillation - ventricular fibrillation |
|
|
What is a heart block? ***
|
failure of SA node or AV node impulse conduction due to scar formation
(usually sequela of MI) |
|
|
What is excitation? ***
|
firing of impulses is slowed or irregular
(can be corrected by pacemaker) |
|
|
What are fibrillations? ***
|
chronic twitching of the heart with or without regular contractions
result of disorganized current flow within the atria or ventricles that interrupts normal contractions |
|
|
What are atrial fibrillations? ***
|
most common cardiac arrhythmia
atria twitch and ventricles receive irregular input and do not fill properly |
|
|
What are ventricular fibrillations? ***
|
more serious
ventricles "twitch" and blood is not pumped leads to cardiac arrest, permanent damage to brain, heart, organs, and death within minutes |
|
|
What are premature ventricular contractions (PVC)? ***
|
ventricles skip a beat or beat too soon, causing irregular rhythms or beats that are out of synchronization
|
|
|
What is tachycardia? ***
|
heart rate increases rapidly (greater than 100 bpm)
|
|
|
What is bradycardia? ***
|
heart rate is abnormally slow (< 60 BPM) (book says < 50 BPM)
|
|
|
What is auscultation? ***
|
listening through a stethoscope for abnormal sounds
|
|
|
What is an ECG? ***
|
electrocardiogram
non-invasive procedure to check electrical activity of heart |
|
|
What are P waves?
QRS waves? T waves? *** |
- atrial contraction
- ventricular contraction - repolarization of ventricles |
|
|
What does an ECG help diagnose? ***
|
- coronary artery disease
- myocardial infarction - valvular heart disease - congenital heart disease - arrhythmias - heart blockages |
|
|
What is an echocardiogram? ***
|
a non-invasive procedure that uses ultrasound waves to examine the
- size, shape, and motion of heart structures, - heart valve movements, - measurements of chambers, and - changes of chambers during cardiac cycle |
|
|
What is color Doppler echocardiography? ***
|
explores blood flow patterns and changes in velocity, and allows evaluation of valvular stenosis or insufficiency
|
|
|
What is coronary arteriography? ***
|
selective injection of contrast dyes into coronary artery with X-rays showing blood vessel action/blockages
|
|
|
What are some treatment procedures for cardiac disease/defects? ***
|
- drug therapy
- angioplasty - lasers - pacemaker implants - open-heart surgeries |
|
|
What are some available drug treatments for cardiac disease? ***
|
- vasodilators - Capoten (Captopril), Vasotec (Enalapril), Corgard (Nadolol)
- anticoagulants (or thinners), Persantine (Diprydiamole), Coumadin (Warfin Sodium), Calciparine (Heparin) - antibiotics – penicillin or any of a number - diuretics – Lasix, Furomide (Furosemide) - antiarrhythmics – Lanoxin (Digoxin) - antidepressants or antianxiety medications – Xanax (Alprazolam), BusSpar (Buspirone Hydrochloride) |
|
|
What are some surgical treatments for cardiac disease? ***
|
- angioplasty - balloon catheterization and stent increase internal vessel diameter, thereby allowing increased blood flow rate
lasers - improves circulation by dissolving blockages - pacemaker implants – provides regularity of stimulation to SA and AV nodes - open heart surgeries: CABG, reconstruction/replacement, transplant |
|
|
What are some open heart surgeries? ***
|
- CABG – coronary artery bypass graft using LE saphenous vein as replacement
- reconstruction/replacement – repair and replacement with synthetic materials - transplant – implantation of donor heart |
|
|
What elements comprise the arterial system? ***
|
- arteries
- arterioles - capillaries |
|
|
Describe an artery. ***
|
- muscular and thick walls
- strong - considerable elastic tissue - several layers - lined with endothelium (intima) |
|
|
Describe an arteriole. ***
|
- smaller lumen than artery
- thinner walls, mostly of smooth muscle fiber arranged circularly - lined with endothelium - constrict/dilate via ANS to SNS, which alters blood flow to tissues |
|
|
Describe capillaries. ***
|
- minute vessels, about 1/2 to 1 mm long
- lumen as wide as RBC - walls consist of a layer of endothelium only |
|
|
How do veins compare to arteries? ***
|
- thinner walls
- larger lumen - less elastic (collapse easily) - most superficial of the blood vessels - contain one-way valves to help return blood upward to heart against gravity - skeletal muscle contractions greatly assist blood movement as well - deeper veins are located parallel with arteries |
|
|
What are some diseases of the arteries? ***
|
- arteriosclerosis
- atherosclerosis - thrombosis/embolism - aneurysm - hemorrhagia - Raynaud's disease |
|
|
What is arteriosclerosis? ***
|
"hardening" of the arteries
- affects small arteries/arterioles - degenerative (aging) process - vessels become brittle and lose elasticity; can rupture - leads to hypertension - progressive thickening/roughening of intima makes vessels susceptible to thrombus (blood clot) formation - clot formation can result in decreased blood flow to tissue distal to thrombus (= ischemia) - partly due to calcium deposition |
|
|
What is atherosclerosis? ***
|
fatty hardening of the arteries
- affects medium and large arteries; a form of arteriosclerosis - lipid plaque (fatty deposit) build up on intima - lumen narrows and may become occluded - occlusion can result in decreased/absent blood flow to tissue distally (= ischemia) |
|
|
In what arteries is atherosclerosis of the most concern? ***
|
- coronary artery (MI)
- cerebral artery (CVA) |
|
|
What is a thrombus? ***
|
formation of blood clots on blood vessel walls due to adherence of platelets on roughened surfaces
occlusion can cause infarct (tissue necrosis) |
|
|
Where do thrombi typically form? ***
|
- in areas of slower blood flow (veins)
- in areas of turbulence (scarred/diseased heart valves) - on roughened vessel walls (atherosclerosis and rheumatic heart disease) - can form when blood's platelet count is too high (increased viscosity) |
|
|
What is the typical treatment for thrombi? ***
|
anticoagulants
sometimes surgery to remove the thrombus or embolism |
|
|
What is an embolism? ***
|
a traveling mass of undissolved matter present in a vessel
can be comprised of fibrin, bits of tissue, blood clots, tumor cells, fat globules, air bubbles, clumps of bacteria, any foreign bodies occlusion of vessel can cause infarct |
|
|
When do emboli occur in vessels? ***
|
- when a thrombus breaks loose
- entry of bacteria due to lack of sterile techniques (septic embolism) - entry of air bubbles during surgery - entry of fat globules with fracture - entry of foreign body with injury |
|
|
Emboli can travel in vessels and cause: ***
|
occlusion
ischemia infarct (MI, CVA, blockage in an organ) |
|
|
What happens to tissues after an infarct? ***
|
tissue death allows bacteria to enter
gangrene follows gangrene can infect viable tissue leads to possible amputation or death |
|
|
What is coagulation necrosis? ***
|
localized tissue death distal to the clot
|
|
|
What is an aneurysm? ***
|
localized dilation (fusiform) or sac-like (saccular) formation in arterial wall (lumen)
can enlarge and rupture, resulting in hemorrhaging which can be life-threatening, especially in the brain, aorta, heart, etc. |
|
|
How are aneurysms treated? ***
|
if detected early enough can sometimes be surgically repaired with grafts
depends on location and size |
|
|
What is hemorrhagia? ***
|
- a large loss of blood internally or externally
- often caused by aneurysms, head injuries, and bleeding diseases |
|
|
What is Raynaud's disease? ***
|
- functional disorder of the arteries caused by vasospasms
- poor blood flow to the fingers or toes causing numbness, discoloration, and intermittent pain - vasospasm in fingers/toes that cuts off circulation - brought on by exposure to cold or by stressful events |
|
|
What are some diseases of the veins? ***
|
- phlebitis
- varicose veins |
|
|
What is phlebitis? ***
|
inflammation of a vein, usually of the lower extremities
|
|
|
What causes phlebitis? ***
|
- injury
- infection - obesity - poor circulation it is a serious problem if in deep veins because it can lead to DVT (thrombophlebitis) |
|
|
What are the symptoms of phlebitis? ***
|
- warmth
- pain - edema - erythema to area of DVT - thrombus can dislodge and cause embolism |
|
|
What is the treatment for phlebitis? ***
|
- anticoagulants
- occasionally surgery to remove clot |
|
|
What are varicose veins? ***
|
enlarged, swollen knotty superficial veins, usually in the lower leg (saphenous vein)
caused by stagnation and pooling of blood in veins often painful |
|
|
How do varicose veins form? ***
|
the veins become dilated due to
- poor milking action of muscles to enhance venous return; blood pools - increased back pressure of blood (due to some sort of obstruction) |
|
|
Stagnating blood causes ______ on veins and results in dilation of veins.
|
pressure
leads to incompetent valves and pooling of blood |
|
|
What are some causes of varicose veins? ***
|
- history of prolonged standing/sitting
- pregnancy or uterine tumor (increased pressure on veins in pelvic region resulting in backup or pooling of blood) - heredity - obesity - can result in venostasis (slowed venous blood flow leading to ulcers due to poor circulation) |
|
|
What is the treatment for varicose veins? ***
|
- elastic wraps
- support stockings - walking - elevating legs when sitting - stripping and ligation - laser |
|
|
What is hypertension (HTN)? ***
|
- persistently high arterial blood pressure (150/90); (book says 140/90 mm Hg)
- caused by persistent peripheral resistance to blood flow (atherosclerosis) - often called the "silent killer" as it is the leading cause of CVA, CHF |
|
|
What are some causes of/risk factors for hypertension? ***
|
- prehypertension
- heredity (esp. African Americans) - advancing age - smoking - obesity - excessive salt, fat, and/or alcohol intake - lack of exercise |
|
|
How does the nervous system attempt to control blood pressure? ***
|
if low, nervous system vasoconstricts vessels to increase peripheral pressure
if excessively high, nervous system causes dilation of arterioles in kidney resulting in increased blood flow to kidneys and increased urine output, which lowers blood volume and thus blood pressure |
|
|
With what other disease/organ is hypertension linked? ***
|
hypertension can cause kidney failure
kidney disease can cause hypertension decreased kidney function leads to water retention, increased blood volume, and elevated blood pressure long-standing hypertension causes arteriosclerosis of renal artery that reduces blood flow to kidneys and causes damage to them |
|
|
What are the two types of hypertension? ***
|
- primary (essential) - develops for idiopathic reasons, may be asymptomatic for months/years; 90-95% of cases
- secondary - results from another pathology/disease (e.g., kidney disease, tumor of adrenal gland which regulates salt retention) |
|
|
What are the effects of hypertension? ***
|
- overworks heart, leading to CHF or MI
- vessels become sclerotic, resulting in thrombus formation, embolus, or ruptures (CVA, MI) - affects kidneys, heart, eyes, blood vessels |
|
|
What is the treatment for hypertension? ***
|
- diuretics (decrease fluid volume)
- vasodilators (decrease peripheral resistance) - decrease salt intake (decrease fluid retention) - weight reduction - cessation or decrease of smoking - increase exercise (increase circulation) |
|
|
What is shock? ***
|
a life-threatening vascular change resulting from assault or injury in which blood flow/pressure is inadequate to sustain life
condition that reduces heart's ability to pump effectively or decreases venous return |
|
|
Name four types of shock. ***
|
- hypovelemic shock
- neurogenic shock - cardiogenic shock - anaphylactic shock - septic shock |
|
|
What is hypovolemic shock? ***
|
results from decreased blood volume due to excessive loss of fluid (hemorrhaging causing blood loss, severe burns causing plasma loss)
|
|
|
What is neurogenic shock? ***
|
results from decreased vasomotor tone/damage to central nervous system (poor venous return) due to SCI, spinal anesthesia, drugs
|
|
|
What is cardiogenic shock? ***
|
results from extensive MI or arrhythmia which causes inadequate oxygen
|
|
|
What is anaphylactic shock? ***
|
severe allergic reaction (insect bite, drug, food, etc.)
results in vasodilation throughout vessels causing a decreased blood flow to vital organs |
|
|
What are some diagnostic procedures for vascular diseases? ***
|
- auscultation
- electrocardiogram (ECG/EKG) - echocardiography - Doppler echocardiography - exercise tolerance test - cardiac catheterization - angiocardiography - coronary arteriography - carotid phonoangiography - ultrasound arteriography - angiography |
|
|
What is an electrocardiogram?
|
ECG/EKG
electrical recording of heart action to aid in diagnosis of coronary artery disease, myocardial infarction, valve disorders, and some congenital heart diseases, as well as arrhythmias and heart block |
|
|
What is echocardiography?
|
ultrasound cardiography
noninvasive procedure that uses high-frequency sound waves to examine the size, shape, and motion of heart structures it gives a time-motion study of the heart, which permits direct recordings of heart valve movement, measurements of the heart chambers, and changes that occur in the heart chambers during the cardiac cycle |
|
|
What is an exercise tolerance test?
|
used to diagnose coronary artery disease and other heart disorders
it monitors the ECG and blood pressure during exercise, and problems that do not normally occur at rest are revealed |
|
|
What is cardiac catheterization? ***
|
procedure in which a catheter is passed into the heart through blood vessels to sample the blood in each chamber for oxygen content and pressure
findings can indicate valve disorders or abnormal shunting of blood and aid in determining cardiac output |
|
|
What is angiocardiography?
|
a contrast indicator (dye) is injected into the cardiovascular system
in conjuction with X-rays of the heart and great vessels, the aorta, and pulmonary artery to detect blockage in vessels |
|
|
What is carotid phonoangiography? ***
|
- non-invasive procedure
- special microphones over abnormal sounds heard with stethoscope (areas of carotid arteries); sound reproduced on oscilloscope to locate carotid stenosis |
|
|
What is ultrasound arteriography? ***
|
- non-invasive procedure
- (a.k.a. Doppler imaging) -- special ultrasound equipment uses echoes of moving blood to produce images of vessel wall outline, measures velocity of blood and degree of arterial stenosis |
|
|
What is angiography? ***
|
- invasive procedure
- examination of blood vessels by X-ray, vessels made visible by injection of radioactive substances (e.g., arteriograms and venograms) |
|
|
The cardiovascular system pumps blood through approximately _______ miles of blood vessels? ***
|
60,000
|
|
|
Disorders of what functions are directly and indirectly responsible for many of the diseases that affect pulmonary and systemic circulation?
|
disorders of:
- blood flow - blood pressure - cardiac function |
|
|
Disorders of blood flow and blood pressure include:
|
the diseases of
- arterial and - venous circulation |
|
|
Disorders of cardiac function consist of diseases of:
|
- pericardium
- coronary heart disease - myocardial disease - endocardial disease - heart valve disease - cardiac conduction disturbance - heart failure - heart disease in infants and children |
|
|
What are the transport proteins that carry cholesterol throughout the body called?
|
lipoproteins
|
|
|
Which is the major cholesterol carrier in the blood?
|
low-density lipoproteins (LDL)
|
|
|
What are risk factors for peripheral artery disease?
|
- male
- age 70-80 - heredity - environmental risks |
|
|
Treatment of Raynaud's disease includes:
|
- reducing triggers
- protecting hands from trauma and cold - avoiding emotional stress - sometimes medications that prevent vasospasm |
|
|
What is a fusiform aneurysm?
|
a uniform shape with symmetrical dilation around the entire circumference of the artery
|
|
|
What is a saccular aneurysm?
|
an outpouching of only one portion of the aortic wall
|
|
|
Blood pressure ranges
|
below 120/80 - healthy
120/80 to 139/89 - prehypertension - 140/90 - 159/99 - stage 1 HTN - 160/100 and up - stage 2 HTN |
|
|
What is the most common cardiovascular disorder?
|
hypertension
affects about 20% of adult population worldwide |
|
|
What is pulmonary arterial hypertension?
|
idiopathic or secondary high blood pressure in the pulmonary artery that causes the following changes :
- vasoconstriction - endothelial and/or smooth muscle proliferation - intimal fibrosis and thrombosis of the pulmonary capillaries or arterioles |
|
|
Symptoms of pulmonary arterial hypertension?
|
- dyspnea (shortness of breath)
- syncope (loss of consciousness) as the disease advances, pumping ability of heart weakens and symptoms occur at rest |
|
|
Treatment for pulmonary arterial hypertension?
|
- medication
- oxygen therapy - lung transplant without treatment, prognosis is poor with median survival rate less than 3 years |
|
|
How is blood returned to the heart from the lower extremities?
|
blood flows from superficial (saphenous) veins to deeper venous channels for return
valves along the deeper veins and skeletal leg muscles assist in moving the blood |
|
|
What are spider veins?
|
small, dense networks that appear as red or blue discolorations on the skin
|
|
|
Cause of spider veins?
|
unknown
may be genetic, hormonal (puberty, birth control pills, pregnancy, HRT) |
|
|
Treatment of spider veins?
|
laser treatment or saline injection to scar them shut
followed by continuous compression for several weeks, and walking to activate leg muscle venous pumps |
|
|
What is chronic venous insufficiency (CVI)?
|
condition of poor venous blood return to the heart
|
|
|
What are the most common causes of chronic venous insufficiency (CVI)?
|
- deep vein thrombosis
- incompetence of venous valves and muscles that aid in blood return |
|
|
What are the signs and symptoms of chronic venous insufficiency (CVI)?
|
- tissue congestion
- edema - necrosis or skin atrophy - pain on walking - venous stasis ulcers in advanced cases |
|
|
What are the risk factors for chronic venous insufficiency (CVI)?
|
- advancing age
- family history of deep vein thrombosis (DVT) - sedentary lifestyle - obesity - smoking |
|
|
When is the peak incidence of chronic venous insufficiency (CVI)?
|
- men in their 70s
- women in their 40s |
|
|
What is the treatment for chronic venous insufficiency (CVI)?
|
- mild cases - diet, exercise, and compression stockings
- more severe - surgical repair of valves, vein bypass/stripping |
|
|
What are some signs and symptoms of venous thrombosis?
|
- asymptomatic in 50% of cases
- similar to inflammation with pain, swelling, deep muscle tenderness |
|
|
Why is early detection and prevention of venous thrombosis important?
|
to prevent potentially fatal complications such as emboli
|
|
|
What is the most common cause of coronary heart disease?
|
atherosclerosis (90% of cases)
|
|
|
What is the leading cause of death worldwide?
|
coronary heart disease
|
|
|
What are the symptoms of coronary heart disease?
|
- chest pain/angina pectoris
- palpitations - dizziness/fainting - weakness - shortness of breath - nausea - pallor - cardiac arrest/MI |
|
|
How is coronary heart disease treated?
|
- blood pressure-lowering agents
- blood thinners - diuretics - nitrates to stop chest pain - lipid-lowering medications - lifestyle changes (diet/exercise) |
|
|
What is myocarditis and what causes it?
|
inflammatory disease of the heart muscle
caused by virus (e.g., HIV, Coxsackie, adenovirus, echovirus) or bacteria |
|
|
How is myocarditis diagnosed?
|
- EKG detects conduction disturbances
- echocardiogram may show enlargement/inflammation of heart - blood culture test to show infection, detect certain heart muscle enzymes |
|
|
What are the symptoms of myocarditis?
|
- it's often asymptomatic
- history of viral illness - fever - chest pain that feels like heart attack - shortness of breath - tachycardia |
|
|
How is myocarditis treated?
|
- prevention of further damage with bed rest
- antibiotics if bacterial infection |
|
|
What is cardiomyopathy and what are the 3 types?
|
functional disease of the myocardium
- dilated cardiomyopathy - hypertrophic cardiomyopathy - restrictive cardiomyopathy |
|
|
What is dilated cardiomyopathy and how is it treated?
|
- most common form
- dilation of the ventricle, contractile dysfunction, symptoms of CHF - treated with medications, rest, and surgical transplant in severe cases |
|
|
What are the causes and signs/symptoms of dilated cardiomyopathy?
|
may result from:
- infections - myocarditis - toxic agents - metabolic disorders - genetic disorders - immune disorders - often idiopathic symptoms include: - dyspnea on exertion - orthopnea - weakness - fatigue - ascites - peripheral edema |
|
|
What is hypertrophic cardiomyopathy and how is it treated?
|
- characterized by ventricular hypertrophy/excessive ventricular growth
- most common cause of sudden cardiac death in the young - treatment includes medications and surgery |
|
|
What are the causes and signs/symptoms of hypertrophic cardiomyopathy?
|
- etiology often unknown, but some genetic mutations found
- may be asymptomatic |
|
|
What is restrictive cardiomyopathy?
|
- least common form of cardiomyopathy
- associated with reduced heart-filling pressures and endocardial scarring/rigidity in the ventricle - endemic in parts of Africa, India, Asia, and South/Central America |
|
|
What are the cause and signs/symptoms of restrictive cardiomyopathy?
|
- most common cause is amyloidosis, a group of diseases in which one or more organ systems accumulates abnormal protein deposits
- symptoms include dyspnea, orthopnea, peripheral edema, ascites, weakness, and fatigue |
|
|
How does mitral stenosis manifest?
|
- mitral valve opening is narrowed by rigidity in the cusps, which often fuse together (most often due to sequela of rheumatic fever)
- blood flow from left atrium to left ventricle meets resistance and atrial wall hypertrophies - resistance leads to back pressure into pulmonary veins causing pulmonary congestion - backed up fluid leaks into tissues causing edema - poor circulation causes cyanosis because left ventricle doesn't have time to fill before it beats - backup of blood and congestion cause heart to become exhausted and may lead to CHF |
|
|
What is another risk of mitral stenosis?
|
increased risk for a thrombus to form on the valve, become detached, and become an embolus
|
|
|
How is mitral stenosis remedied?
|
- surgical valvuloplasty (similar to angioplasty)
- may lead to complications such as leaky valve, in which case it will be replaced with metal alloy or a pig valve |
|
|
How does mitral insufficiency/regurgitation manifest?
|
- valve is unable to close completely (often due to failure of papillary muscles/chordae tendinae)
- blood leaks back into atrium with each ventricle contraction - causes lung congestion |
|
|
What is mitral valve prolapse (MVP)?
|
papillary muscles and chordae tendinae are unable to prevent mitral valve cusps from opening upward under force of expelled ventricular blood
|
|
|
How is mitral valve prolapse (MVP) treated?
|
- most people are asymptomatic and lead normal lives
- those with moderate to severe cases may take antibiotics to prevent bacteria from colonizing in the defective valves - in most severe cases, surgical reconstruction or replacement |
|
|
What is aortic stenosis and what causes it?
|
- aortic semilunar valve narrows
- may be sequela of rheumatic fever, - congenital defect, or - arteriosclerosis - most common in men over 50 |
|
|
What are the symptoms of aortic stenosis and how is it treated?
|
symptoms include:
- left ventricular hypertrophy - syncope - can be corrected surgically |
|
|
What is aortic insufficiency/regurgitation and what causes it?
|
- aortic semilunar valve doesn't close properly and blood flows back into left ventricle from aorta
- can result from endocarditis or a dilated aorta |
|
|
What are the symptoms of aortic insufficiency/regurgitation?
|
- gradual onset; asymptomatic for a number of years; only sign may be a heart murmur
- diastolic BP drops - left ventricle hypertrophies, becomes exhausted, and fails - dyspnea, even at rest - syncope |
|
|
Two categories of cardiac arrhythmias
|
supraventricular arrhythmias--those generated by electrical abnormalities in the:
- sinoatrial (SA) node - atria - atrioventricular (AV) node - and junctional tissue in the heart ventricular arrhythmias generated in the ventricular conduction system and in the ventricle |
|
|
Which are the most serious arrhythmias?
|
ventricular arrhythmias, since the ventricles are the pumping chambers, these arrhythmias can be life-threatening
|
|
|
What are two disorders of cardiac rhythm (arrhythmia)?
|
- tachycardia (sustained > 100 BPM)
- bradycardia (sustained < 50 BPM) (she says < 60 BPM) |
|
|
What can interruption of the flow of impulses through the conduction system of the heart lead to?
|
heart block
|
|
|
What does heart block cause the atria and ventricles to do?
|
contract independently of one another
|
|
|
What is the most serious consequence of a heart block?
|
circulation to vital organs is cut off
|
|
|
What is an ectopic pacemaker?
|
an excitable focus outside the pacemaker of the heart (SA node) that can cause additional beats or take over normal pacemaker activity
|
|
|
What are some symptoms of cardiac arrhythmias?
|
- palpitations
- syncope - edema - shortness of breath |
|
|
What are some causes of cardiac arrhythmias?
|
- history of coronary heart disease
- heart valve disease - myocardial infarction - hypertension - atherosclerosis - metabolic diseases - smoking, drug abuse, etc. |
|
|
How are cardiac arrhythmias treated?
|
- electrocardioversion with an external (AED) or surgically placed internal pacemaker/defibrillator
- catheter ablation - nonsurgical procedure of inserting catheter into heart to direct energy to sever pathway of abnormal rhythm - antiarrhythmic medications to alter physiological properties of heart's conduction system |
|
|
What is septic shock?
|
shock caused by toxins released by bacterial infection
|
|
|
What puts a baby at increased risk of congenital heart disease?
|
- born to parents with a history of congenital heart disease
- born with chromosomal abnormalities such as Down syndrome - maternal diabetes, rubella infection, maternal alcoholism,, and treatment with anticonvulsant drugs - maternal age over 40 |
|
|
How is congenital heart disease classified?
|
- etiologies that do not cause cyanosis
- etiologies that cause cyanosis (by allowing deoxygenated blood to bypass the lungs and return to systemic circulation) |
|
|
Symptoms of Tetrology of Fallot
|
- difficulty feeding/gaining weight
- poor development - cyanosis, especially with strain (feeding, crying, defecation) - fainting - sudden death - clubbing of fingers - squatting during episodes of cyanosis |
|
|
Treatment for Tetrology of Fallot
|
numerous corrective surgeries
|
|
|
What is transposition of the great arteries?
|
the aorta and pulmonary artery are transposed
aorta is connected to right ventricle and pulmonary artery to left ventricle |
|
|
How is transposition of the great arteries treated?
|
- if found prenatally, prostaglandin administration to keep patent ductus arteriosus open
- surgery within first 2-3 weeks of life to correct |
|
|
Symptoms of coarctation of the aorta
|
- dizziness
- shortness of breath - cold legs - harsh murmur |
|
|
How is coarctation of the aorta treated?
|
surgical correction
|
|
|
In a normal heart, blood flows from the left atrium into the:
|
left ventricle
|
|
|
What does an EKG record?
a. blood flow to the heart b. pulmonary trunk and pulmonary circulation c. electrical events of the heart d. blood pressure |
c. electrical events of the heart
|
|
|
The bicuspid valve normally maintains one-way blood flow into the:
|
left ventricle
|
|
|
The rate of contraction of the heart can be increased by increased activity in the:
a. sinoatrial node b. sympathetic nerves c. parasympathetic nerves d. a and b are correct |
d. a and b are correct
|
|
|
The primary cause for hypertension is:
|
atherosclerosis
|
|
|
Hypertrophy of the myocardium due to excess work in pumping against high blood pressure produces what type of heart disease?
a. hypertensive heart disease b. myocardial infarction c. congestive heart failure d. congenital disease |
a. hypertensive heart disease
|
|
|
In a heart attack caused by blood clots blocking the coronary arteries, circulation can be quickly restored by administration of:
a. nitroglycerin b. thrombolytic drugs c. CPR d. angioplasty |
b. thrombolytic drugs
|
|
|
The tetralogy of Fallot involved four defects in the structure of the heart, including:
a. pulmonary stenosis b. atrial septal defect c. open foramen ovale d. patent ductus arteriosis |
a. pulmonary stenosis
|
|
|
Blood can flow back into the atrium and cause pulmonary hypertension in what type of valvular disease?
|
mitral insufficiency
|
|
|
Failure of the ventricle to contract when heart block occurs is caused by an abnormal
a. valve action b. contraction of the cardiac muscle c. conduction system d. tachycardia |
c. conduction system
|
|
|
Diuretics help with congestive heart failure. (T/F)
|
true
|
|
|
Left heart congestive failure produces edema in the ankles, liver and spleen, with enlargement of the neck veins. (T/F)
|
false
left side causes lung congestion |
|
|
The parasympathetic nerve impulses act as a braking system to slow heart rate. (T/F)
|
true
|
|
|
Highly oxygenated blood is found in the right side of the heart (T/F)
|
false
|
|
|
Cardiomyopathy tends to result in congestive heart failure. (T/F)
|
true
|
|
|
Strokes may be hemorrhagic or ischemic. (T/F)
|
true
|
|
|
Diastolic pressure is the pressure in the venous blood. (T/F)
|
false
|
|
|
Heart murmurs are sounds that indicate abnormality of valves. (T/F)
|
true
|
|
|
Rheumatic heart disease is an infection of the endocardium and valves by Group A hemolytic streptococci. (T/F)
|
false
|
|
|
Stasis of blood flow frequently causes vegetations to form on the valve cusps. (T/F)
|
false
|
|
|
Contraction of the ventricles is called ________.
|
systole
|
|
|
Syncope is caused by a _________ of blood to the brain.
|
lack
|
|
|
________________ is a temporary chest pain from lack of oxygen to heart.
|
angina pectoris
|
|
|
The heart requires stimulation from the _________ to regulate the rate of contraction.
|
sinoatrial node
|
|
|
__________ disease is caused by constriction of arteries in fingers and toes.
|
Raynaud's
|
|
|
As a result of hypertension, the left ventricle develops __________ as it constantly pumps against high resistance in the arterial system, and eventually develops __________ as it weakens from the overload.
|
hypertrophy; dilation
|
|
|
Left-sided congestive heart failure produces ___________ in the patient.
|
pulmonary edema
|
|
|
In a child with a ventricular septal defect, ____________ indicates blood is shunting from left to right.
|
cyanosis
|
|
|
The ________ is a fetal vessel used to bypass the non-functioning fetal lungs.
|
patent ductus arteriosus
|
|
|
______________ stems from pulmonary hypertension and causes right-side heart failure.
|
cor pulmonale
|
|
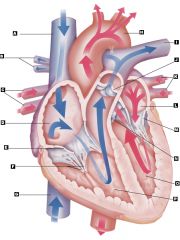
|
1.1 Tricuspid valve E.
1.2 Bicuspid (mitral) valve M. 1.3 Left pulmonary artery (to lung) I. 1.4 Right atrium D. 1.5 Left atrium L. 1.6 Right ventricle P. 1.7 Left ventricle O. 1.8 Aorta H. 1.9 Right pulmonary veins (from lung) C. 1.10 Left pulmonary veins (from lung) K. 1.11 Chordae tendineae F. 1.12 Inferior vena cava (from trunk and legs) G. 1.13 Superior vena cava (from head and arms) A. 1.14 Pulmonary semilunar valve J. 1.15 Right pulmonary artery (to lung) B. 1.16 Aortic valve N. |
|
|
tachycardia
|
excessively rapid heart rate, > 100 BPM
|
|
|
major congenital heart anomaly
|
tetrology of Fallot
|
|
|
phlebitis
|
inflamed veins
|
|
|
ischemia
|
deficient blood supply
|
|
|
infarct
|
area of dead tissue
|
|
|
myocardial infarction
|
heart attack
|
|
|
blood test for MI
|
serum enzymes
|
|
|
stasis
|
slowed blood flow
|
|
|
sclerotic
|
hardened, scarred
|
|
|
fibrillation
|
uncoordinated, inefficient contraction
|
|
|
What are the primary purposes of blood? ***
|
- transportation
- defense |
|
|
What are the prime elements of blood? ***
|
formed elements
- erythrocytes (RBCs) - leukocytes (WBCs) - thrombocytes (platelets or cell fragments; clotting cells) nonformed elements - plasma |
|
|
What elements does blood transport? ***
|
- O2/CO2
- water - nutrients - salts - proteins - hormones - waste products - bloodborne diseases |
|
|
What does blood defend against? ***
|
- diseases
- infections - toxins - antigens - other foreign elements |
|
|
What are the formed elements of blood? ***
How much of the blood do they account for? *** |
- erythrocytes
- leukocytes - thrombocytes/platelets account for 45% of blood |
|
|
What is plasma? ***
How much of blood does it account for? *** |
- liquid element (everything else)
- accounts for 55% of blood |
|
|
Where do erythrocytes come from? ***
|
- cells formed only in red bone marrow of flat bones (e.g., sternum, iliac crest, ribs)
- process is called erythropoeisis |
|
|
What are some properties of erythrocytes? ***
|
- mature cells are biconcave, have no nucleus and few organelles
- prime component is hemoglobin, a chromoprotein of red color that carries oxygen - most abundant cell in human body - RBCs outnumber WBCs 700 to 1 |
|
|
Where are leukocytes formed? ***
|
in red bone marrow and lymph tissue
|
|
|
What WBCs comprise the granulocytes, and what are their functions? ***
|
- neutrophils (65%) - ingest bacteria
- eosinophils (2-4%) - function unknown - basophils (0.5%) - function unknown |
|
|
What WBCs comprise the agranulocytes, and what are their functions? ***
|
- lymphocytes (25%) - large and small, non-phagocytic, likely source of serum protein and immune bodies
- monocytes (5%) - ingest larger particles |
|
|
What condition(s) is indicated by an elevated number of neutrophils? ***
|
- acute bacterial infections
- inflammatory disorders - certain drugs - stress |
|
|
What condition(s) is indicated by an elevated number of eosinophils? ***
|
- allergies
- parasitic infestations |
|
|
What condition(s) is indicated by an elevated number of lymphocytes? ***
|
viral infections
|
|
|
What condition(s) is indicated by an elevated number of monocytes? ***
|
chronic severe infections when controlled
(what the hell does this even mean?) |
|
|
What are platelets? ***
|
- cell fragments
- formed in red bone marrow - a.k.a. thrombocytes - essential for blood clotting; form knots to which fibrin adheres, liberating thromboblastin and facilitating the blood clot - stimulate the phagocytic action of leukocytes |
|
|
Trace the (re)-development of red blood cells ***
|
- proerythroblast - red bone marrow
- erythroblasts - nuclei shrink as hemoglobin develops - reticulocytes - nuclei digested but endoplasmic reticulum remains; emerge from marrow at this stage - mature erythrocytes |
|
|
What are some common blood disorders? ***
|
- anemias - reduced hemoglobin or HGB hg
- polycythemias - excessive amount of RBCs - neoplastic diseases - cancers of WBCs, bone marrow, and/or lymph tissue - infectious mononucleosis - viral infection |
|
|
What are some causes of anemias? ***
|
- prolonged bleeding (e.g., GI ulcers, surgical procedures, menstruation)
- hemolysis - rupture of cells, sickle cell anemia - disturbances of RBC formation - inhibition, loss, or failure of bone marrow - deficiencies of iron or B12 - chronic disease |
|
|
What are some signs and symptoms of anemia? ***
|
- pallor - decreased color of skin, mucous membranes, and nail beds due to decreased hemoglobin
- fatigue and muscle weakness due to decreased oxygen - dyspnea and tachycardia - shortness of breath, increased heart rate, increased respiratory rate (body's attempt to get more O2 to tissues) - heart palpitations - reflex from coronary arteries - jaundice and enlarged spleen (with hemolytic anemia) |
|
|
What are some types of anemia? ***
|
- pernicious anemia (B12 deficiency)
- hemolytic anemia (sickle cell, spheroidal) - hypochromic anemia also - iron deficiency anemia (same as hypochromic????) - anemia of chronic disease (RA, TB deplete iron stores) - anemia of renal disease (fail to produce erythropoietin) - megaloblastic anemia (impaired DNA synthesis due to deficiency in B12 and/or folic acid) - folic acid deficiency anemia |
|
|
Characteristics of pernicious anemia ***
|
- a.k.a. Vitamin B12 deficiency anemia
- RBCs cannot develop, few in number, membranes rupture easily - more common in anglos, rare before age 30 - intrinsic factor in gastric juice not secreted - normally intrinsic factor enables extrinsic factor of vitamin B12 to be absorbed from small intestines into the blood - vitamin B12 cannot be absorbed and RBCs cannot develop |
|
|
What are the signs and symptoms of pernicious anemia? ***
|
- numbness and tingling of hands and feet
- diarrhea - vomiting - nausea - sore tongue with smooth, glazed appearance - responds well to IM injection of vitamin B12 |
|
|
Characteristics of hypochromic anemia ***
(Is this also run-of-the-mill iron-deficiency anemia?) |
- iron deficiency due to chronic blood loss from bleeding ulcers, malignant tumor, or excessive menstrual bleeding
- results in decreased amount of hemoglobin per cell, but number of RBCs is adequate (the cells are pale = hypo + chromic) - responds well to large doses of iron |
|
|
Characteristics of hemolytic anemia ***
|
- malformed RBCs rupture prematurely (before 90-120 day average lifespan)
- hemoglobin breaks down, yielding bilirubin (pigment formed is orange/yellow and accumulates in plasma, causing yellow appearance in skin, sclera, etc.) - can be caused by malarial parasites, immune disorders, or as an allergic reaction to drugs such as sulfonamides |
|
|
Characteristics of sickle cell anemia ***
|
- red cell deficiency, cells are crescent shaped and tend to rupture
- RBCs contain abnormal form of hemoglobin (hemoglobin S) - pain in arms, legs, abdomen - recurrent fever, jaundice of sclera - crisis period with headache, paralysis and convulsions as well as tissue and eventual organ death - no cure; only able to treat symptoms |
|
|
Characteristics of spherodoidal anemia ***
|
- cells are spherical rather than biconcave
- cell ruptures due to fragility - results in jaundice and splenomegaly - treatment may be removal of spleen, resulting in increased susceptibility to infection |
|
|
Characteristics of erythroblastosis fetalis ***
|
- disease of newborns
- anemia, jaundice, enlarged liver and spleen - Rh- mother develops antibodies against Rh+ blood factor fetus inherits from father - severity: mild anemia to death - treated by vaccine of Rh immunoglobulin (RhoGam) within 24 hours of delivery of Rh- infant - next fetus will not have condition - blood testing as part of prenatal care can prevent disease |
|
|
Characteristics of aplastic anemia ***
|
- bone marrow stops producing RBCs, WBCs, and platelets
- pt is anemic, cannot fight infection, has tendency to bleed - caused by excessive radiation, certain drugs, and industrial poisons - treatment is blood transfusion and bone marrow transplants |
|
|
What is secondary anemia? ***
|
- accompanies another disease
- chronic kidney disease - leukemia - cancer - number of cells is normal, but Hgb is low - treated with administration of iron |
|
|
Characteristics of polycythemias/excessive RBCs ***
|
- primary polycythemia myeloproliferative or excessive RBC count
caused by: - hyperactivity of red bone marrow, usually secondary to tumor - elevated RBC count increases blood volume, raises blood pressure, increased work load on heart - blood flow is reduced due to increased viscosity and tendency to clot |
|
|
What are some signs and symptoms of polycythemia? ***
|
- purplish skin
- red mucous membranes - bloodshot eyes - enlarged spleen - elevated RBC, WBC, and platelet count - dizziness - headaches - visual disturbances - itching - pain in fingers and toes - thromboembolism resulting in death |
|
|
Treatment for polycythemia ***
|
- purpose is to reduce RBC count and blood volume
- phlebotomy: periodic blood letting - radiation therapy to decrease red cell production - chemotherapy to suppress production of all blood cells by bone marrow |
|
|
Characteristics of secondary polycythemia ***
|
- erythrocytosis or high RBC count
causes - any inadequate O2 supply to the body results in production of excessive RBCs as compensation - high altitudes have low O2 in air - muscles of elite athletes have increased need for O2 - increased O2 needs for patients with congenital heart disease, CHF, and emphysema |
|
|
How are primary and secondary polycythemia differentiated? ***
|
- primary - all blood cell types produced in bone marrow are affected
- secondary - only RBC count is elevated |
|
|
What is hemophilia? ***
|
- defective or absent clotting mechanism
- mother-to-son inherited genetic disorder - caused by absence of clotting factor due to lack of plasma protein for coagulation, although blood platelets are normal - treatment is transfusion or administration of clotting protein concentrates |
|
|
Characteristics of purpura (idiopathic thrombocytopenic purpura--ITP) ***
|
- thrombocytopenia or deficiency in number/excess destruction of platelets needed for blood clotting mechanism
- results in spontaneous hemorrhaging in skin, mucous membranes of mouth and internal organs - often follows viral infection in children under 5, and resolves in a few weeks; chronic condition and not associated with viral infection in adults caused by - impaired platelet production (bone marrow), - ratio of antibodies to platelets (immune system), - allergic response to drugs |
|
|
Signs and symptoms of purpura (idiopathic thrombocytopenic purpura--ITP) ***
|
- petechia - small, flat, red spots on the skin
- ecchymoses - large, irregularly-shaped hemorrhagic areas of the skin - gastrointestinal and urogenital hemorrhages - severe nosebleeds and bleeding from mucous membranes of the mouth - treatment is corticosteroids or splenectomy |
|
|
Neoplastic diseases ***
|
- cancers of WBCs, bone marrow, and/or lymph tissue
- leukemia - uncontrolled production of (immature?) WBCs - cause - malignancy of WBCs affecting bone marrow and lymph tissue |
|
|
Signs and symptoms of leukemia ***
|
- anemia, pallor, fever, bone/joint pain
- enlarged spleen (splenomegaly) - swollen lymph nodes (lymphadenopathy) - enlarged liver (heptamegaly) - abnormal bleeding and tendency to bruise easily - unexplained weight loss - general weakness, shortness of breath, heart palpitations - susceptible to infection since immature WBCs cannot fight off infection |
|
|
Types of leukemia ***
|
- myelogenous
- lymphatic |
|
|
Characteristics of myelogenous leukemia ***
|
- cancer of the bone marrow
- acute myelogenous leukemia is more common in adults and males - chronic myelogenous leukemia has a prolonged course affecting mature cells |
|
|
Characteristics of lymphatic leukemia ***
|
- cancer of the lymph nodes
- acute lymphatic leukemia is more common in children with an abrupt onset and rapid progression - chronic lymphatic leukemia has a prolonged course affecting mature cells |
|
|
What is the treatment for leukemia? ***
|
- often fatal, but some respond well to chemotherapy
- three stages: induction, consolidation, and maintenance - 50-90% complete remission possible depending on type of leukemia |
|
|
Characteristics of malignant lymphomas ***
|
- malignancies of lymphoid tissue (phagocytic cells - histocytes and macrophages)
- thought to be caused by virus that interferes with normal lymphocyte production - Hodgkin's disease is most common |
|
|
Signs and symptoms of malignant lymphomas ***
|
- swelling in one lymph node
- fever - weight loss |
|
|
Treatment for malignant lymphomas ***
|
- responds well to radiation and chemotherapy if localized to one or two areas
- cure rate good if treated early |
|
|
Characteristics of infectious mononucleosis ***
|
- viral infection common in children and young adults
- caused by Epstein-Barr herpes virus |
|
|
Signs and symptoms of infectious mononucleosis ***
|
- mild fever
- marked fatigue - sore throat - swollen lymph nodes - elevated WBCs - high percentage of atypical lymphocytes that resemble monocytes - tender, enlarged spleen |
|
|
Treatment of infectious mononucleosis ***
|
- antibiotics not effective vs. viruses
- bed rest if fever present - avoid contact sports to protect spleen |
|
|
Composition of hemoglobin
|
globulin - a protein
heme - a molecule which binds to iron |
|
|
How does hemoglobin function?
|
- in lungs, binds to O2 in exchange for CO2
- O2 RBCs travel to tissues and release O2 in exchange for CO2 |
|
|
How long do RBCs live, and how are they disposed of afterward?
|
about 120 days
removed from body by liver and spleen |
|
|
Does anemia typically develop slowly or quickly?
With symptoms or asymptomatic? |
typically slowly and asymptomatically
|
|
|
How does the body control iron balance?
|
- it is conserved for reuse
- no excretory pathway - only means of iron loss from the body are blood loss and loss of epidermal cells from the skin and gut |
|
|
How much iron is required daily and how much do we typically ingest?
|
1.0 - 1.4 mg/day
average 15 mg/day (males) and 11 mg/day (females) |
|
|
Where does iron absorption take place?
|
in the small intestine
|
|
|
How does iron-deficiency anemia progress?
|
- first stage - negative iron balance (anemia may not yet be present)
- second stage - iron stores in body are depleted; syntheis of hemoglobin impaired and RBCs become pencil-shaped |
|
|
What is the leading cause of anemia worldwide?
Whom does it chiefly affect? |
iron-deficiency anemia
preschool children and adolescent/adult females |
|
|
Characteristics of folic acid deficiency anemia
|
caused by
- low intake of folic acid, - malabsorption due to bowel inflammation (e.g., Crohn's disease), - excessive demand, as during pregnancy, or - side effect of some medications treated with oral supplementation |
|
|
How is hemolytic anemia treated?
|
depends on underlying etiology
- splenectomy (decreases risk of gallstones, hemolytic crises and pathological changes to bone marrow) - blood transfusion (in cases of severe blood loss) - antibiotics for infectious causes - immunosuppressants for immune disorders - cease taking offending medications |
|
|
What are hemoglobinopathies?
|
- disorders affecting structure, function, or production of hemoglobin
- usually inherited - mutations that result from synthesis of abnormal hemoglobin |
|
|
Name the two most common hemoglobinopathies.
|
- sickle cell anemia
- thalassemia |
|
|
By what mechanism do cells assume the sickled shape in sickle cell anemia?
|
when the RBC deoxygenates, hemoglobin S forms cross-links with other hemoglobin S molecules and long crystals develop, pulling the cell into the characteristic shape
|
|
|
Treatment of sickle cell anemia
|
- no cure
- aim is to prevent crisis, control anemia, and relieve pain - blood transfusions |
|
|
What are the most common genetic disorders in the world
|
thalassemias
|
|
|
Symptoms of thalassemia
|
in most severe form:
- severe, life-threatening anemia - bone marrow hyperactivity - enlargement of spleen - growth retardation - bone deformities due to deficient synthesis of alpha or beta chains required for proper formation and performance of hemoglobin |
|
|
Treatment of thalassemia
|
blood transfusions required to sustain life, and life expectancy reduced
|
|
|
What causes bleeding disorders (poor clotting/continuous bleeding)?
|
- platelet dysfunction/deficiency
- vitamin K deficiency - clotting factor deficiency |
|
|
Where are platelets produced?
Where are clotting factors produced? |
in the bone marrow
in the liver |
|
|
What elements are critical to hemostasis?
|
- platelets
- prothrombin - thrombin - vitamin K - calcium |
|
|
What is thrombocytopenia?
What causes it? |
abnormally small number of circulating platelets
conditions that - impair production - increase destruction, or - cause sequestration of platelets |
|
|
What is the most common bleeding problem among hospitalized patients?
|
thrombocytopenia
|
|
|
What is disseminated intravascular coagulation?
|
- condition involving destruction of platelets and consumption of clotting factors
- thrombin released into systemic circulation causing systemic coagulation and suppression of normal physiological anticoagulation mechanisms - causes extensive ischemia, organ damage, and depletion of platelets and clotting factors |
|
|
Occurrence of disseminated intravascular coagulation
Treatment of disseminated intravascular coagulation |
occurs in conjunction with:
- sepsis/blood infection - endothelial damage as in shock, OB complications or neoplasms (cancer) treatment includes platelet transfusions, coagulation inhibitors, IV anticoagulants when needed |
|
|
What is neutropenia?
|
reduction in circulating neutrophils that increases risk for bacterial and fungal infections
|
|
|
Causes of neutropenia
|
- cancer chemotherapy
- using immunosuppressive drugs - immune destruction of neutrophils with RA |
|
|
Treatment of neutropenia
|
- growth factors/colony-stimulating factors
- corticosteroids if immune destruction is the cause |

