![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
243 Cards in this Set
- Front
- Back
|
Describe the structure of bone ***
|
Fibrous connective tissue, impregnated with mineral salts
- Connective tissue gives bone its toughness/elasticity - Mineral salts give bone is hardness/rigidity |
|
|
Bone shapes ***
|
- long
- short - flat - irregular (- sesamoid) |
|
|
What is periosteum? ***
|
tough fibrous outer membranous covering of a bone
|
|
|
Characteristics of periosteum ***
|
- Highly vascular (blood supply to bone)
- Inner lining of periosteum contains osteoblasts (cells responsible for growth and repair of bone) |
|
|
What is compact bone? ***
|
a.k.a. cortical bone
outer bone layer laid down in concentric circles |
|
|
What is spongy bone? ***
|
a.k.a. cancellous bone
inner bone layer; porous appearance |
|
|
Characteristics of spongy bone ***
|
- thin calcified plates (trabeculae) laid down in response to stress
(this is why exercise is important to bones!) - primarily at ends of long bones and in flat bones - contains spaces filled with red marrow (for RBC formation) |
|
|
Components of (long) bone ***
|
- medullary cavity
- diaphysis - epiphysis - metaphysis |
|
|
What is the medullary cavity? ***
|
- central cavity of long bone
- filled with yellow marrow (fat) in adults (this is what can cause embolism with a fracture) |
|
|
What is the diaphysis? ***
|
the shaft of the long bone
|
|
|
What is the epiphysis? ***
|
the expanded ends of the long bone
|
|
|
What is the metaphysis? ***
|
the epiphyseal growth plate
- a disc of cartilage between diaphysis and epiphysis in children - new bone forms here - when growth stops, cartilage disappears and ossification occurs |
|
|
How may bones become infected? ***
|
Infectious agents can enter the bone through
- open fractures - from bloodstream - from adjacent infected tissue |
|
|
What is osteomyelitis? ***
|
inflammation of bone (medullary cavity and spongy bone)
- local and systemic infection - most common in children and adolescents - long bones affected (femur, humerus, tibia) |
|
|
How does osteomyelitis form? ***
|
- infectious pyogenic organism (staph) from bloodstream/open wound enters bones
- abscess forms - pus fills cavity - local inflammatory response (heat swelling, pain) - vessels in area are compressed due to edema - bone tissue ischemia, then necrosis - separation of necrotic bone from healthy bone (sequestrum) - blood clots from infectious tissue travel to other bone sites and form new bone abscesses |
|
|
What are the systemic effects of and treatment for osteomyelitis? ***
|
- systemic effects: fever/chills, elevated WBC level
- tx: massive (IV) antibiotics, NWB, surgery to necrotic bone |
|
|
Characteristics of tuberculosis of bone ***
|
- while TB is primarily a lung disease, it can spread to other structures
- infectious tubercules from lungs travel via bloodstream to bone - iInfectious clumps form on bone, cavities develop in bone, bone tissue is destroyed - commonly affects: ends of long bones, cartilage in joints |
|
|
Sequelae of tuberculosis of bone ***
|
- arthritis of joints
- destruction of growth plates - Pott’s disease (vertebral column of children); results in spinal deformity, possible nerve impingements |
|
|
Treatment for tuberculosis of bone ***
|
- TB antibiotics
- surgery to correct deformities |
|
|
How does Vitamin D deficiency affect bones? ***
|
- Vitamin D is necessary for absorption of calcium and phosphorus into system
- lack of Vitamin D results in soft bones that bend easily: ---- Rickets (children) ---- Osteomalacia (adults) ---- genu varum (bowed legs) ---- genu valgus (knock knees) ---- also spinal curvature, delayed teething, and muscle flabbiness |
|
|
How do deficiencies in blood levels of calcium and phosphorus affect bones? ***
|
result in soft, deformed bone
Vitamin D is needed for these minerals to be absorbed into the system |
|
|
What is the treatment for Vitamin D (and calcium/phosphorous) deficiency? ***
|
- sunshine
- supplements - fortified milk - cod liver oil |
|
|
What is osteitis fibrous cystica? ***
|
- caused by hyperactivity of parathyroid
- excessive production of parathyroid hormones pulls calcium from bones (increases activity of osteoclasts) - cysts and nodules form in bones, which decalcify and become porous - results in bone deformities, spontaneous fractures, calcium in vessels, kidney stones, depressed nervous system |
|
|
Treatment for osteitis fibrous cystica ***
|
- drug therapy
- removal of parathyroid tumor - surgery to correct deformity |
|
|
What is Paget's disease? ***
|
- softening of the bone
- causes remodeling and overproduction of soft “immature” bones - etiology unknown; possibly genetic - results in enlarged bones (primarily skull, pelvis, vertebrae) - also frequent fractures and bony deformities |
|
|
Treatment for Paget's disease? ***
|
- if mild, none
- if severe: NSAIDS, diet, drugs to prevent bone loss |
|
|
What is osteoporosis? ***
|
- increased porosity of bone
- leads to reduction in bone mass - skeletal system becomes fragile (primarily vertebral bones, pelvis, femur, radius) - traebecular/spongy bone affected mostly, but compact bone too - occurs most frequently in white females > 50 yrs. |
|
|
Causes of osteoporosis ***
|
- possibly heredity
- females with small bone mass - aging process with decreased estrogen post-menopause - immobilization/disuse atrophy - calcium-poor diet (particularly in teen years when bone is developing) - lack of exercise |
|
|
Complications of osteoporosis ***
|
- compression fractures of vertebral bodies (causing pain, spinal nerve pressure)
- fractures of weight bearing bones (hips, pelvis) radius (wrist) - curvature of spine (kyphosis) - decreased height |
|
|
Treatment for osteoporosis ***
|
- exercise
- estrogen therapy - calcium-rich diet - surgery for fractures |
|
|
What are the two most common deformities of the spinal column? ***
|
- scoliosis
- kyphosis |
|
|
Name four types of bone neoplasms ***
|
- osteoma
- giant cell tumors - osteogenic sarcoma - secondary tumors |
|
|
What is osteoma? ***
|
- benign growth
- usually develops at end of long bone - can affect joints |
|
|
What are giant cell tumors? ***
|
- benign or malignant
- removed surgically |
|
|
What is osteogenic sarcoma? ***
|
- primarily malignant
- most common in children (long bones, knee) - can develop from Paget's disease - treated with chemotherapy or amputation |
|
|
What are secondary tumors? ***
|
- cancer that has metastasized (generally from lung or breast)
- very painful in bone - easily fractures ribs, sternum, skull (highly vascular bones) |
|
|
What is a fracture and what are some causes? ***
|
- disruption of the continuity of bone
caused by - trauma excessive stress on bone - fatigue - repeated stress on bone (stress fracture) - pathology - disease process (TB, CA, osteoporosis) |
|
|
Name ten types of fractures ***
|
- open (compound)
- closed (simple) - avulsion - comminuted - compression - depressed - greenstick - impacted - multiple - spiral |
|
|
Open fracture ***
|
a.k.a. compound fracture
- fractured bone pierces skin can result in - infection (osteomyelitis) - contamination - soft tissue damage |
|
|
Closed fracture ***
|
a.k.a. simple fracture
- no communication with external - skin not pierced |
|
|
Impacted fracture ***
|
- one fractured end is forced into the other end
- commonly due to falls - also common in hip fractures |
|
|
Greenstick fracture ***
|
bone fractures on one side, but bends on the other
common in children because their bones have more organic matrix and are more flexible |
|
|
Comminuted fracture ***
|
fracture with splintered, fragmented, bony pieces
common in those with brittle bones, such as osteogenesis imperfecta |
|
|
Multiple fracture ***
|
more than one segment of bone fractures
|
|
|
Avulsion fracture ***
|
occurs when a fracture of bone tears away from the main bone due to external force or trauma
|
|
|
Compression fracture
|
bone is crushed
common in patients with osteoporosis |
|
|
Depressed fracture
|
broken bone is pressed inward
common in skull fractures |
|
|
Spiral fracture
|
jagged break due to twisting force on bone
common fracture in sports injuries |
|
|
What are the five stages of fracture healing? ***
|
- hematoma - blood seeps out and surrounds fx’s surfaces
- granulation - hematoma invaded by tiny capillaries; tissue becomes soft and rubbery - callus - osteoblasts (repair cells for bone from periosteum) enter site of repair and lay irregular trabeculae of bone; new blood vessels grow into tissue; osteoclasts reabsorb necrotic bone - consolidation - osteoblasts organized, callus transformed into mature bone - remodeling - union is complete; newly formed bone forms a “collar” that is stronger, thicker, and denser than the original bone |
|
|
What are four types of treatment for fractures? ***
|
- closed reduction
- open reduction internal fixation - external fixation - mechanical traction |
|
|
What is the primary goal of fracture treatment? ***
|
reduction of fracture
realignment of bone |
|
|
What is closed reduction of a fracture? ***
|
- manual manipulation
- realignment of bone from outside - no surgery - cast to immobilize while healing |
|
|
What is open reduction and internal fixation (ORIF) of a fracture? ***
|
surgery performed
- fracture site and wound cleaned out, and - fracture fixed with pins, plates, screws, etc., or - prosthesis (TKA, etc.) |
|
|
What is external fixation of a fracture? ***
|
- percutaneous pins/wires connected to a rigid external frame
- allows 3-plane correction of a deformity |
|
|
What is mechanical traction of a fracture? ***
|
- fracture is immobilized in a traction unit
- especially with long bones of the lower extremities - until healed or ORIF (think of the old cartoons with the casted leg elevated in a sling) |
|
|
What are some possible complications of a fracture? ***
|
- TBI (skull fracture)
- SCI (vertebral fracture) - damage to surrounding organs (muscles, vessels, organs) - embolism (fat, blood clot, air) can become pulmonary embolism - infection, especially with compound fracture or ORIF - delayed union, or non-union, due to poor vascular supply - bone shortening - issues due to immobilization (pneumonia, decubitus ulcers) - avascular necrosis - death of bone tissue due to lack of blood supply ---- can lead to tiny breaks in the bone and eventual bone collapse ---- most often affects head of femur, causing hip pain ---- can affect other bones as well |
|
|
What is a joint? ***
|
the articulation of two or more bones
|
|
|
Structure of a joint ***
|
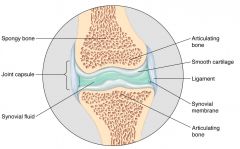
- articulation of two or more bones
- articulating surfaces covered with hyaline cartilage - often cartilaginous discs/menisci present between bones to ----- serve as shock absorbers/distributors ----- accommodate movement (vertebrae, knee) |
|
|
What is a sprain? ***
|
- tearing or stretching of ligaments surrounding joint (Grade I-III)
- can rupture blood vessels of surrounding tissue; joint intact - once torn, it’s torn because the tissue is avascular - also easier to re-sprain b/c it is stretched and remains stretched |
|
|
Signs and symptoms of a sprain ***
|
- inflammation
- edema - ecchymosis (blood from somewhere superior) - pain - LOM |
|
|
What is dislocation/subluxation of a joint? ***
|
- bone displaced from joint (shoulder, finger, patella)
- secondary to excessive force or poorly formed joint - soft tissue damage - edema - pain - deformity - LOM - may be congenital: displaced bone in joint due to improperly formed joint in newborn; usually hip |
|
|
What is arthritis? ***
|
inflammation of a joint or joints resulting in pain, swelling, and stiffness
|
|
|
What is rheumatoid arthritis? ***
|
- progressive, chronic, systemic inflammatory disease of the joints
- inflammation of synovial membrane with membrane thickening (pannus) - spreads to joint space and results in erosion of articulating surfaces due to inflammatory phase (inflammation continuous) - scar tissue forms - joint ankyloses (fuses); can be severely crippling - results in no joint motion - subcutaneous nodules in areas of increased mechanical pressure often occur (usually in MCPs) - affects multiple bilateral joints - periods of exacerbation/remission |
|
|
Cause of and treatment for rheumatoid arthritis ***
|
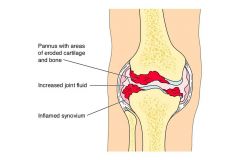
cause:
- possible tissue hypersensitivity secondary to autoimmune reactions - possible genetic factor treatment: - no cure - treat symptoms with anti-inflammatories, prednisone (steroids) - exercise (do not overstretch pt) - possible surgery |
|
|
What is juvenile RA? ***
|
- RA with onset prior to age 16
- can be severe and crippling by young adulthood |
|
|
What is the most common form of arthritis? ***
|
osteoarthritis
|
|
|
What is osteoarthritis? ***
|
- deterioration of articulating cartilage resulting in exposure of underlying bone
- causes new bone formation (hypertrophy) - osteophytes (spurs) develop - often affects only one joint; usually a weight bearing joint (hip, knee, vertebra) - affects sexes equally |
|
|
Cause of and treatment for osteoarthritis ***
|
- cause unknown
- associated with injured/overworked joints - aging worsens with increased weight - no cure - treat symptoms with analgesics, NSAIDS, corticosteroid injections - decrease WBing on joint, lose weight, - possible surgery |
|
|
What is the structure of skeletal muscle? ***
|
- consists of bundles of muscle cells (fibers)
- muscle fibers consist of myofibrils which contain actin and myosin - myofibrils comprise contractile units called sarcomeres - the number of muscle fibers present in a muscle is fixed - any increase in size of muscle is brought about by hypertrophy of each individual fiber (increased mitochondria, increased myofibrils) |
|
|
What is a motor unit, and how does it function? ***
|
- motor unit = all the muscle fibers innervated by one motor neuron and its axon
- stimulation of motor unit occurs at neuromuscular junction - requires release of Ach from presnynaptic junction - excess Ach cleaned up by (acetyl)cholinesterase enzyme |
|
|
What is tendinitis/tendonitis and how is it treated? ***
|
inflammation of tendon due to
- trauma - repeated microtrauma (sports) - postural malalignment - can result in scarring, calcium deposits laid down treatment: - immobilization - NSAIDs - steroidal injections - PT |
|
|
What is a strain? ***
|
- damage to muscle tissue
mild; without loss of continuity of fibers severe: - partial or complete tear of muscle - loss of continuity of muscle fibers |
|
|
What is a cramp? ***
|
painful, involuntary muscle contraction due to
- electrolyte imbalance or - muscle fatigue decreased blood flow leads to ischemia, which sets off reflex contraction muscle soreness due to: 1) microtears of muscle or CT 2) edema due to accumulation of metabolic wastes (need acetylcholinesterase to clear wastes out; this is why DOMS is helped by doing a couple of pushups) |
|
|
What is compartmental syndrome? ***
|
- condition which develops when there is increased pressure in an enclosed and limited anatomical space resulting in compression of muscles, nerves, vessels
- extremities (esp LE) are susceptible to compartmental syndrome because muscles, nerves, blood vessels, and bone are surrounded by non-expanding fascial sheaths - any condition that increases the contents of the compartment (usually inflammation, edema) puts patient at risk for neuromuscular damage due to ischemia - check distal muscles, pulse, sudden onset of foot drop - can cause permanent damage if not treated |
|
|
Causes of and treatment for compartmental syndrome? ***
|
causes:
- burns - intensive use of muscles - bites - capillary filtration treatement - fasciotomy |
|
|
What is Muscular Dystrophy? ***
|
- a group of uncommon inherited conditions in which there is progressive degeneration and destruction of muscle fibers
- cell defect which interferes with protein metabolism necessary for providing energy for muscle contraction - muscles necrose and are replaced by connective tissue and fat - different types of dystrophies (9 in all), all have muscle wasting in common |
|
|
What is Duchenne's Muscular Dystrophy? ***
|
- sex-linked recessive gene carried by mother
- affects males exclusively - diagnosed by 2-3 years (Gower’s sign) - affects proximal muscles (shoulder/pelvic girdles) - wheelchair-bound by 8-10 years after diagnosis - death usually by 20 years due to cardiac/respiratory complications |
|
|
What is myasthenia gravis? ***
|
- disorder of the neuromuscular junction; but nerve and muscle are intact
- autoimmune disease - antibodies produced which cover many of the Ach receptors at motor end plate on post-synaptic membrane - results in decreased stimulation of muscle tissue; weakness - females > males 20-40 years - can be life threatening if respiratory muscle involvement |
|
|
Treatment for myasthenia gravis ***
|
treatment:
- cholinesterase-inhibiting drugs (Ach stays in cleft longer an has more a chance to bind onto available receptor site) - plasmaphereis – blood removed, plasma which contains antibodies is skimmed off, blood elements returned |
|
|
What is rhabdomyosarcoma and how is it treated? ***
|
- rare, malignant cancer of skeletal muscle
- highly malignant, metastasizes early - poor prognosis - treatment: aggressive chemotherapy, surgery to remove cancerous muscle tissue |
|
|
What is myositis (heterotropic) ossificans? ***
|
a.k.a. heterotropic ossification
- an extra-osseous, non neoplastic growth of new bone - occurs most commonly in the second and third decade in the arms and thighs of patients who have experienced some sort of trauma - quadriceps and brachialis are the most affected |
|
|
What causes myositits (heterotropic) ossificans? ***
|
- not applying R.I.C.E.M. (rest, ice, compression, elevation, and motion) immediately after injury.
- having intensive physical therapy or massage too soon after injury - returning too soon to training after injury |
|
|
What are the signs and symptoms of myositis ossificans? ***
|
- restricted range of motion
- pain in the muscle with movement - (palpable) hard lump in the muscle - x-ray showing bone growth |
|
|
Treatment of myositis ossificans ***
|
- rest from activity
- usually will resolve itself in time - may require surgical excision of calcified tissue - also prone to reoccur |
|
|
What is Osgood Schlatters disease? ***
|
- common cause of knee pain in children and young athletes
- tibial tuberosity becomes inflamed, painful and swollen |
|
|
Cause of Osgood Schlatters disease ***
|
- patellar tendon inserts at the tibial tuberosity and through overuse can tug away at the bone causing inflammation
- most often in children involved with running and jumping activities - with repeated trauma, new bone grows back during the healing - causes a bony lump which is often felt at the tibial tuberosity. |
|
|
Signs and symptoms of and treatment for Osgood Schlatter's disease ***
|
- tenderness and pain on the tibial tuberosity during and after exercise.
- pain when contracting the quadriceps against resistance or when contracting the muscles with the leg straight treatment - rest from activity - ice after sports activity - knee brace or support |
|
|
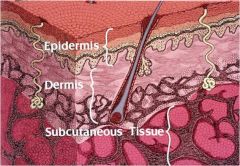
Structure of skin ***
|
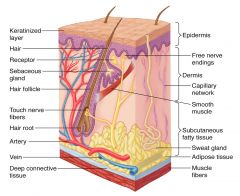
Skin consists of two primary layers:
- epidermis (outer layer) and - dermis (deeper layer) with an - underlying subcutaneous layer of fat |
|
|
What is the epidermis? ***
|
- multi-layered
- consists of squamous (layered) epithelium - contains free nerve endings - no blood vessels - keratinocytes (water-proofing cells) - melanocytes (skin pigments) |
|
|
What is the dermis? ***
|
- underlies epidermis
- has nerve endings - has special sensory receptors - rich vascular bed - hair follicles (epithelial beds) - sweat glands - sebaceous glands |
|
|
What is the subcutaneous fat layer? ***
|
- underlies dermis
- connects dermis to underlying fascia - provides food reserve and insulation - sweat glands - sebaceous glands |
|
|
Name 10 types of skin lesion ***
|
- bulla
- fissure - macule - nodule - papule - pustule - scales - ulcer - vesicle - wheal |
|
|
What is a macule? ***
|
a discolored spot of skin that is neither elevated above nor depressed below the surrounding skin surface
|
|
|
What is a papule? ***
|
a solid, red, elevated skin lesion
|
|
|
What is a nodule? ***
|
a solid, hardened, elevated skin lesion
|
|
|
What is a vesicle? ***
|
a small (generally less than 0.5 cm) fluid-filled blister
|
|
|
What is a bulla? ***
|
a large (generally greater than 0.5 cm) fluid-filled blister
|
|
|
What is a pustule? ***
|
a circumscribed, raised skin lesion filled with pus
|
|
|
What is a wheal? ***
|
a generally round, transient elevation of skin, white in center, with pale red edges
often accompanied by itching |
|
|
What are scales? ***
|
thin, dry dead tissue shed from upper layers of skin
|
|
|
What is a fissure? ***
|
a crack like a sore or ulcer
|
|
|
What is an ulcer?
|
an erosion or eating away of tissue
|
|
|
What are infectious skin diseases? ***
|
those that result from
- bacteria - virus - fungus - parasite |
|
|
What is impetigo and how is it treated? ***
|
- bacterial infection
- most often seen in children - caused by strep or staph - oozing vesicles that crust over - treated with antibiotics |
|
|
What is an abscess and how is it treated? ***
|
- a.k.a. carbuncle
- cluster of boils (furuncles) - caused by staph infection - involve imbedded hair follicles and subcutaneous tissue - treated with antibiotics - occasionally irrigation and drainage (I&D) |
|
|
What is herpes simplex I and how is it treated? ***
|
- painful vesicles which form scabs
- cycles of dormancy/activity - recur with stress, sunburn, reduced immunity - treated with topical analgesics |
|
|
What is herpes zoster (shingles)? ***
|
- reactivation of chicken pox
- eruptions of painful water blisters along nerves affected by virus - usually on trunk or face - unilateral |
|
|
What are warts? Name three types. ***
|
- virus causes proliferation of keratinocytes and hypertrophy of epidermis
- verucca vulgaris (elevated, seen in children) - plantar (grow inward on soles of feet, painful) - genital (can be sexually transmitted) |
|
|
Name two fungal diseases and their treatment ***
|
- ringworm - red, ring-shaped pruritis (actually a fungus, not a worm)
- athlete's foot - fissures, pruritis - treated with antifungal medications and good hygiene |
|
|
Name two parasitic infections and their treatment ***
|
- pediculosis - skin infestation with lice
- scabies - skin infestation with mites - treated with medication and good hygiene |
|
|
Name two hypersensitivity disorders and their symptoms ***
|
- urticaria (hives) - allergic reaction, wheals, pruritus
- eczema (dermatitis) - delayed allergic response to substance which has contacted skin (e.g., poison ivy, dyes, perfumes, soaps) erythema, vesicles, bulla, pruritus |
|
|
Name four types of neoplastic skin diseases ***
|
- nevus
- basal cell carcinoma - squamous cell carcinoma - malignant melanoma |
|
|
What is a nevus? ***
|
- benign neoplastic growth of melanocytes
- can become malignant |
|
|
What is a basal cell carcinoma and how is it treated? ***
|
- slow-growing skin cancer
- caused by overexposure to the sun - non-metastasizing - treated with radiation and surgery |
|
|
What is squamous cell carcinoma and how is it treated? ***
|
- fast-growing skin cancer
- caused by overexposure to the sun - metastasizing - treated with radiation and surgery |
|
|
What are malignant melanomas? ***
|
- arise from melanocytes
- highly malignant - can develop from nevi |
|
|
Name six metabolic skin disorders? ***
|
- acne - caused by hyperactive sebaceous glands
- chronic dandruff - caused by hyperactive sebaceous glands - sebaceous cysts - from blocked sebaceous glands ---- large nodules form; contain bacteria and pus; tend to reoccur - pilonidal cysts - gluteal crease near rectum ---- treated with I&D, removal of glands - seborrheic keratosis (senile warts) - raised horny lesions ---- excessive production of keratinocytes; occur with aging - psoriasis - chronic disease, possibly with genetic factor ---- patches of red skin lesions covered with silvery scales ---- non-infectious ---- exacerbations/remissions |
|
|
What are decubitus ulcers? ***
|
- localized area of ischemic necrosis and ulceration
- develops primarily over bony prominences that have been subjected to ---- prolonged pressure ---- shearing forces ---- friction ---- moisture |
|
|
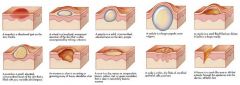
Describe a first stage decubitus ulcer ***
|
- epidermis is intact
- skin is red, does not resolve after 20-30 minutes - usually resolves with pressure relief |
|
|
Describe a second stage decubitus ulcer ***
|
- superficial breakdown in epidermis
- redness, edema, induration (dented in), occasional blistering - usually resolves with pressure relief |
|
|
Describe a third stage decubitus ulcer ***
|
- necrosis into dermis and subcutaneous fat layer
- eschar (leathery, dark, dead skin) present - drainage from wound, infection - PT wound care intervention, debridement (must remove old/dead skin before new skin can proliferate) |
|
|
Describe a fourth stage decubitus ulcer ***
|
- ulceration beyond fat layer into muscle and bone
- eschar (leathery, dark, dead skin), drainage, and infection - if bone is exposed - osteomyelitis, bone destruction - often requires surgical debridement, skin/muscle flaps, osteotomy |
|
|
Are decubitus ulcers typically painful? ***
|
no, especially early on
this is why they go undiagnosed you can test skin blanching to detect |
|
|
What types of patients are most susceptible to decubitus ulcer? ***
|
- debilitated (cancer, pneumonia)
- malnourished (cancer) - immobilizaed (fractures, coma, paralysis) - lack of sensation/mentation (SCI, CVA, TBI) - edematous body parts (esp. due to burns) |
|
|
Where are the most common sites of decubitus ulcers? ***
|
- occiput
- scapula - spinous processes (usually thoracic) - elbow - sacrum - ischial tuberosity - greater trochanter (side-lying) - iliac crest - malleoli (side-lying) - heels |
|
|
What are some means of preventing decubitus ulcers? ***
|
- position, position, position!!
- care in transfer (watch shearing with sheet) - decrease weight bearing - types of mattresses can make a difference - clean sheets - flat sheets (get wrinkles out before putting pt in) - dry sheets Air splints Sheepskin (??) |
|
|
What types of agents can cause burns? ***
|
- thermal
- chemical - electrical - radiation (x-ray, UV) |
|
|
Describe a thermal burn ***
|
- temperature over 111 degrees
- liquids (water, oil, molten metal) - flame (fire, flash burns) - hot objects |
|
|
Describe a chemical burn ***
|
- can continue for long periods of time
- requires immediate washing with copious amounts of water |
|
|
What is cellulitis? ***
|
- spreading skin infection caused by streptococci
- follows other skin damage - red, swollen skin surrounding lesion - streaks, spreads rapidly - fever, chills, pain - may be life-threatening if it spreads to the lymph system or bloodstream |
|
|
What is the clinical importance of burn depth determination? ***
|
- wound care
- excision and grafting - outcome |
|
|
What is a superficial burn (first-degree)? ***
|
- outer epidermal layer, no dermal involvement
- painful (nerve endings) (e.g., sunburn - no blisters, dry and red, will peel) - healing 2-5 days, usually not treated by healthcare team |
|
|
What is a partial-thickness (second-degree) burn? ***
|
- burn into the dermal layer
- epidermis completely destroyed - painful since the dermal layer is not completely destroyed, there are still sweat glands and hair follicles - epithelial beds generate new skin growth |
|
|
What is a superficial partial thickness burn? ***
|
- burn into dermis
- blisters - extremely painful - healing in 1-3 weeks |
|
|
What is a deep partial thickness burn? ***
|
- severe damage to entire dermis
- bleeding - moist, weeping - edema - blanches, mottles - painful - healing in 3-5 weeks - extensive burns usually seen by healthcare team for wound care (change dressing, prevent infection) |
|
|
Upon what does the healing of a partial-thickness burn depend? ***
|
- prevention of infection
- scarring |
|
|
What is a full-thickness (third-degree) burn? ***
|
- all of epidermis, dermis destroyed
- damage to underlying subcutaneous fat layer/muscle - thick eschar, dry and leathery, brown, black, or red - tissue does not blanch (needs to be excised) - anesthetized because nerve endings destroyed - epithelial beds destroyed (no skin buds) - tissue regeneration only from wound edges - usually requires skin grafts - healing time usually takes months, scarring |
|
|
Describe electrical burns ***
|
- complete destruction of all tissues from epithelium to bone
- entrance wound (charred and depressed) and - exit wound (explosive edges) - may require amputation of extremity - often a lot of internal soft tissue/organ damage - difficult to assess |
|
|
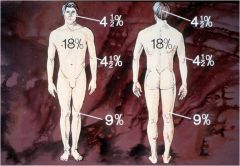
What is the Rule of Nines? ***
|
- size of wound expressed as percentage of total body surface area (TBSA) burned
- Rule of Nines is rapid calculation for determination of %TBSA burned - divides body into multiples of 9 (head = 9%, leg = 18%) - calculations differ from infant-child body to adult body |
|
|
What is the Lund-Browder method for assessing burns? ***
|
- more accurate way to assess TBSA burned
- measures the extent of area burned based on percentage of total surface area affected - uses a table that divides the body based on areas as well as age |
|
|
When area of body burned is greater than 70%, ... ***
|
more than half of victims die
|
|
|
What is mental illness? ***
|
a group of psychiatric disorders characterized by severe disturbances in
- thought - mood - behavior |
|
|
What is psychiatry? ****
|
medical specialty that diagnoses and prescribes medical treatment for mental illness
(can write a prescription) |
|
|
What is psychology? ***
|
studies normal and abnormal behavior and applies counseling to treat mental illness
(no prescriptions) |
|
|
What is the incidence of mental illness in the US? ***
|
1 in 4
|
|
|
What are some warning signs of mental illness? ***
|
- aggression
- changes in eating or sleeping habits - confusion - decline in school or work performance - depression - euphoria alternating with depression - excessive fear - frequent complaints of physical illnesses (somaticizing) - hearing voices - substance abuse - thoughts of suicide - withdrawal from family and friends |
|
|
How many psychiatric diagnoses exist for adults and children? ***
|
over 200
|
|
|
What is the DSM-IV? ***
|
Diagnostic and Statistical Manual of Mental Disorders (IV)
|
|
|
How is the DSM-IV used? ***
|
- internationally to classify, assess, and guide treatment for mental illness
- disorders are categorized according to groups of symptoms or diagnostic criteria - disorders are assigned 5 axes that address adaptive issues and contribute to primary diagnoses - all disorders require evidence of impairment in academic achievement, occupational performance, or social relationships |
|
|
How are the five axes of psychiatric disorders used? ***
|
they guide documentation and are used like a SOAP note
- Axis 1: primary diagnosis (clinical disorders and other conditions that may be a focus of clinical attention) - Axis 2: primary diagnosis (personality disorders, mental retardation, learning disabilities)—hardest to treat - Axis 3: general medical conditions (may not be mental, e.g., TKA, these will be what we see) - Axis 4: psychological and environmental problems - Axis 5: global assessment of functioning |
|
|
How are psychiatric records protected? ***
|
even more stringently than medical records
|
|
|
What are some potential biological causes of mental illness? ***
|
- genes/heredity
- brain size - altered neural connections from trauma - degenerative processes - neurotransmitter malfunction |
|
|
How may neurotransmitters cause mental illness? ***
|
- inadequate regulation
- excess neurotransmitter - burned out receptor sites due to substance abuse, prolonged depression/sadness |
|
|
What is the function of dopamine? ***
|
regulates
- mood - behavior - thought processes - heart rate - blood pressure - appetite/satiety |
|
|
What mental illnesses are associated with inadequate regulation of dopamine? ***
|
- schizophrenia
- depression - ADHD - bipolar disorder - eating disorders - autism - Tourette’s syndrome |
|
|
What mental illnesses are associated with inadequate regulation of norepinephrine? ***
|
- depression
- anxiety disorders - ADHD - bipolar disorder |
|
|
What is the function of norepinephrine? ***
|
regulates
- mood - anxiety - vigilance - arousal - heart rate - blood pressure |
|
|
What is the function of serotonin? ***
|
regulates
- perception of pain - feeding - sleep-wake cycle - motor activity - sexual behavior - body temperature |
|
|
What mental illnesses are associated with inadequate regulation of serotonin? ***
|
- depression
- aggression - suicidality - bipolar disorder - eating disorders |
|
|
What is the function of acetylcholine? ***
|
regulates
- learning - memory - muscle tone |
|
|
What mental illnesses are associated with inadequate regulation of acetylcholine? ***
|
- Alzheimer’s disease
- Parkinson’s disease - Huntington’s Chorea - Tourette’s syndrome |
|
|
What is the function of Gamma aminobutyric acid (GABA)? ***
|
interacts with a wide range of neurotransmitters to enhance inhibition
|
|
|
What mental illnesses are associated with inadequate regulation of Gamma aminobutyric acid (GABA)? ***
|
- anxiety disorders
- alcoholism - Tourette’s syndrome - sleep disorders |
|
|
List two disruptive behavior disorders and their common characterization. ***
|
- conduct disorder
- oppositional defiant disorder they are characterized by willful disobedience |
|
|
Attributes of disruptive behavior disorders ***
|
- affects males > females
- affects children most often - defiance of authority, fighting, school failure, destruction of property are common behaviors - often from broken or violent home situations - associated with harsh physical punishment - often parents may have antisocial disorder or be substance abusers - often (nearly always) overlaps with other psychiatric disorders |
|
|
What is attention deficit hyperactivity disorder (ADHD) and what is its typical treatment? ***
|
neurobiological condition
prominent symptoms of - inattention and/or - hyperactivity/impulsivity affects boys > girls; often persists into adulthood treatment - stimulants and behavioral therapy |
|
|
What are the three subtypes of ADHD? ***
|
- predominantly inattentive - spacey, socially withdrawn, fewer conduct and behavior problems
- predominately hyperactive - impulsive, runs around and fidgets, difficulty engaging in quiet activities, interrupts others, blurts out answers - combined - characteristics of both |
|
|
What is mental retardation? ***
|
- low intelligence
- deficits in social and language skills - results from ---- psychosocial factors ---- biological factors or ---- combination of the two - often unknown etiology |
|
|
What is autistic disorder and what causes it? ***
|
characterized by deficits in
- reciprocal language/language development - social interaction - repetitive stereotyped behaviors (posturing, hand flapping, self-injurious behavior, abnormal eating or drinking patterns) - limited eye contact - speech may be echo-like, and illogical - may not appear until after 3 years of age causes may include - illness that affects CNS: rubella, seizures, encephalitis, toxins. |
|
|
What are tic disorders and how are they treated? ***
|
- tic: sudden, rapid, involuntary movement or vocalization that may be temporarily suppressed by subconscious effort
- exacerbated by stress, anxiety, boredom, fatigue - typically decreases when subject is concentrating on enjoyable task - affects boys > girls - transient tics require no medical treatment - complicated tic disorders require titrated medication therapy |
|
|
What is dementia? List three types and their characteristics. ***
|
dementia - degenerative syndrome with deficits in memory, language in mood
- Alzheimer's disease - most common form; develops gradually after age 60 - Vascular dementia - more abrupt onset, caused by physical insults from HTN, DM, CVA as well as poor nutrition and possibly chronic alcoholism - Parkinson's disease - degenerative neurological movement disorder; dementia in late stages |
|
|
Progression of Alzheimer's disease ***
|
early signs - short-term memory loss
advanced disease - psychosis, aggression, profound personality changes - severe disease - judgment lost, personal care neglected, physical illnesses may lead to death - degeneration of neurons and plaque formation on and around neurons - acetycholine is neurotransmitter most affected |
|
|
Two most common risk factors for Alzheimer's and current treatment methods ***
|
risk factors
- advanced age - family history treatment - medication to slow progression and treat comorbid conditions (e.g., depression, antianxiety medications) |
|
|
Characteristics of substance abuse disorders and treatment for them ***
|
- substance abuse is a conscious choice
- includes alcohol and drug addiction - social problem with extensive emotional and economic consequences warning signs of disorders include - continued use in spite of medical, social, economic, and legal consequences core symptoms of dependency include: - compulsive use, - physical and psychological cravings, - tolerance, and - withdrawal (may be unable to function without substance) treatment: rehab centers, 12 step programs, counseling |
|
|
What is schizophrenia? ***
|
a complex, characterized by
- loss of contact with reality, - severe disturbances in social functioning, - bizarre thoughts - changes in affect or emotional state - patient may have no regard for ADLs - onset usually late teenage years, or adulthood |
|
|
How does schizophrenia present? ***
|
Presentation:
- withdraws from society, increasing concern for abstract and eccentric ideas - may be only episodic, - depression, anxiety, suspiciousness, difficulty concentrating, restlessness early signs - hallucinations, delusions: ---- persecutory (watched, followed, plotted against) ---- grandiose (special powers, influence or wealth) ---- somatic (belief that something is rotting inside their body) |
|
|
Affectation of schizophrenia ***
|
Affects
- “feeling tone”, outward expression of emotion - schizophrenic affect may be unstable and shift rapidly - may be flattened, devoid of emotional expression - motor disturbances: ---- may be catatonic, rigid, disorganized or ---- range from “zombie-like” to wild and aggressive conduct may be blunted having no relationship to social signals |
|
|
Cause of and treatment for schizophrenia? ***
|
causes:
- neurobiological, - family influences, - social and environmental attributes treatment: - most serious known psychiatic illness, - suicide rate 10%, - lower life expectancy - medications influencing dopamine |
|
|
What are mood disorders? Name two. ***
|
- characterized by marked periods of sadness and euphoria
- mood disorders are debilitating and result in vocational failure, social withdrawal, and dysfunctional relationships two mood disorders - major depression - bipolar disorder |
|
|
Characteristics of major depression ***
|
- heredity is predisposing factor
- occurs at any age - women two times more often than men - common in the elderly - feelings of hopelessness, sadness, and despair major depressive disorder consists of at least one episode of serious mood depression followed by a number of changes in behavior - loss of interest or pleasure, - feelings of guilt, worthlessness, anxiety and shame - unexplained weight loss or gain, - disturbed sleep, - poor eye contact, - monosyllabic speech |
|
|
Subcategories of major depression ***
|
Seasonal Affective Disorder: due to decreased sunlight exposure
Postpartum Depression: usually 2 to 6 weeks postpartum, persistent care of newborn, sleep disturbances, social stresses and hormonal changes Premenstrual dysmorphic disorder: Chronic depression or dysthymia if symptoms persist more than 2 years; cyclic depressive symptoms may occur for some women. |
|
|
Treatment for major depression ***
|
- antidepressants
- counseling common comorbid diseases - thyroid disease - chronic heart disease - cancer - HIV infection should be treated as well |
|
|
Characteristics and treatment of bipolar disorder ***
|
a.k.a. manic-depressive illness:
- unusual shifts in mood from depression to mania - affects more than 2 million American adults - typically develops in late adolescence or early adulthood treatment: mood stabilizers (Lithium), individual and family counseling |
|
|
Characteristics of anxiety disorders ***
|
- include a number of disorders with primary feature being abnormal or inappropriate anxiety that interferes with ADLs
- anxiety is normal in response to danger. “fight or flight” - at onset of stressful event HR, respiratory rate, blood pressure, and muscle tension increase in order for us to respond quickly - symptoms of anxiety are problematic if they occur without known cause or disproportionately to stimulus. |
|
|
Name five types of anxiety disorders ***
|
- panic disorder
- generalized anxiety disorder - phobias - obsessive compulsive disorder - post-traumatic stress disorder |
|
|
Characteristics of panic disorder ***
|
- panic attack is sudden onset of fear and terror
accompanied by - physical signs in vital organs, - SOB, - palpitations, - chest pains - symptoms peak within 10 mins.and usually subside within 30-60 mins. - worry about having a panic attack can lead to anxiety disorder - may seek ER care |
|
|
Characteristics of generalized anxiety disorder ***
|
- severe persistent worries, out of proportion to circumstances
- common worries related to work, money, health, safety are difficult to control - restlessness, fatigue, muscle tension, impaired concentration, and disturbed sleep - may be misdiagnosed as depression |
|
|
Characteristics of phobic disorders ***
|
- most common type of anxiety disorder
- irrational fear of something - some, such as fear of the dark, large animals, begin in childhood and disappear with age - may be accompanied with hyperventilation, rapid breathing - facing fear may bring on panic attack |
|
|
What is social phobia? ***
|
- excessive worry and self-consciousness in everyday social situations
- fear of being humiliated to the point that it interferes with ordinary activities - physical symptoms include blushing, profuse sweating, nausea, and difficulty talking. |
|
|
What is obsessive-compulsive disorder? ***
|
- obsessions lead to rituals to prevent or get rid of obsessive stimulus
- rituals are patterns of irrational behaviors, or compulsions that provide temporary relief from the anxiety - patients are often aware of irrational compulsions but cannot stop behavior |
|
|
What is post-traumatic stress disorder? ***
|
- exposure to an intense traumatic event or encounters with rape, child abuse, war or other violence
- victims develop persistent frightening thoughts and memories months or years after event - repeatedly relive experience through nightmares and flashbacks - avoid reminders of event, startle or frighten easily, may feel detached and numb - may lose interest in things previously enjoyed, avoid affection, and become irritable or aggressive |
|
|
How are anxiety disorders treated? ***
|
- medication
- psychotherapy |
|
|
What are personality disorders? ***
|
- persistent, inflexible patterns of behavior that affect interpersonal relationships
- appear in adolescence or early adulthood - remain stable throughout a person’s lifetime |
|
|
What are the three categories of personality disorders? ***
|
Described in DSM-IV in three categories:
- Cluster A: Paranoid and Schizoid - Cluster B: Antisocial, Borderline, Histrionic, and Narcissistic - Cluster C: Avoidant, Dependent, and Obsessive- Compulsive |
|
|
What is a Cluster A personality disorder? ***
|
paranoid personality:
- indifferent, suspicious, and hostile - shallow relationships due to tendency to mistrust acts of kindness schizoid personality: - appear cold and isolated - introverted, self-absorbed, and withdrawn - often deal with fears through superstitions, magical thinking, and unusual beliefs |
|
|
What is a Cluster B personality disorder? ***
|
antisocial personality:
- callous disregard for others and - manipulation of people for personal gratification borderline personality: - often occurs in women deprived of care in childhood - moods are unstable and characterized by crisis and anger alternating with depression histrionic personality: - theatrical and exaggerate their emotions narcissistic personality: - exaggerated self-image and tendency to think little of others - expects others to admire their grandiosity and feel entitled to having needs met |
|
|
What is a Cluster C personality disorder? ***
|
avoidant personality:
- appear shy and timid - fear relationships, although have strong desire to feel accepted - hypersensitive to criticism and rejection dependent personality: - extremely poor self-image - appoint others to make significant decisions our of fear of expressing themselves or offending others - extended illness may bring out a dependent personality in adults obsessive-compulsive personality: - dependable - meticulous, orderly and intolerant of mistakes - often high achievers - attend to details, but never finish the task at hand - avoid new situations and relationships because they cannot be methodically controlled |
|
|
What is the treatment for personality disorders? ***
|
- most people with personality disorders see no need for treatment
- individual, family and group therapy is necessary to point out consequences of behavior - often secondary medical and psychiatric illnesses force persons with PD to seek treatment - rigid thoughts and behavior often complicate treatment, and compliance is an issue - tend to frustrate health care providers - medication is helpful to relieve anxiety, depression, and psychosis |
|
|
Characteristics of suicide risk ***
|
- most often associated with mental illness
- irrational self-directed acts of aggression - seems an alternative when all is viewed as hopeless with no solutions to problems those at risk: - substance abusers, - those with family history of suicide, - those with history of sexual abuse, - those making previous suicide attempts, - those with history of impulsive, aggressive behavior - suicidal behavior most often occurs when people experience major losses and stressful events (e.g., divorce, loss of a job, incarceration, and chronic illness) |
|
|
Warning signs of suicide ***
|
- withdrawal
- talk of death - giving away cherished possessions - sudden shift in mood (severely depressed person may suddenly appear better) - schizophrenic may progressively develop delusions about death |
|
|
What is stress? ***
|
how a person reacts to what happens to them
|
|
|
What is eustress? ***
|
stress that invigorates
|
|
|
What is the difference between distress and eustress? ***
|
- the individual's reaction
- the meaning they attach to stress - how they cope with stress |
|
|
Distress arises when... ***
|
imposed demands are perceived to exceed one's ability to cope
(again, it's all about perceptions) |
|
|
What is the alarm reaction? ***
|
the body's response to stress
under stress, the body requires more - glucose and - oxygen for extra energy - hypothalamus regulates internal functioning of body to - control homeostasis and - direct proper responses during stressful situations hypothalamus does this through regulation of ANS and endocrine system |
|
|
How does the ANS function during stress? ***
|
hypothalamus stimulates SNS
SNS releases epinephrine - vasoconstriction of skin and GI - increased BP - vasodilation of heart, brain, respiratory tract - increased respiratory, venous return, cardiac output - stimulation of liver to release glucose = more oxygen and glucose for "fight or flight" |
|
|
How does the endocrine system (hormones) function during stress? ***
|
hypothalamus stimulates pituitary gland through release of hormones
pituitary gland stimulates: - adrenal cortex to release corticosteroids--inflammatory response, increased blood glucose - thyroid gland releases thyroxine--Increased cellular activity (increased energy, body heat) |
|
|
What happens due to corticosteroid presence in the body for long periods of time? ***
|
- an excess of anti-inflammatory hormones produced during stress can cause the spread of an infection by weakening the body’s barricade around the infectious organism
- steroids suppress the immune reaction reaction against microorganisms, reducing the patient’s response to infection |
|
|
Name some stress-related diseases ***
|
gastrointestinal:
- diarrhea/constipation - vomiting, eating disorders - GI ulcers, ulcerative colitis, Crohn’s disease cardiovascular: - elevated BP secondary to vasoconstriction of peripheral vessels - increase of adrenal cortex sexual function: - decreased libido, sexual function, impotence respiratory: - common cold - asthma skin: - fever blisters - eczema - psoriasis |
|
|
What factors influence wellness? ***
|
- genetic make-up, family medical history, body size and shape
- family environment, loved ones and friendships - psychological characteristics: positive self image, ability to manage stress - external physical environment: food, water, air, work setting, residential setting - lifestyle: proper diet; regular exercise; avoidance of smoking, alcohol and drug abuse - unresolved negative emotions: emotional stress, tension, anger |
|
|
What are the components of a well-balanced diet? ***
|
High-fiber low-fat diet: research suggests a high fiber, low-fat diet lowers the risk of colon and rectal cancer and leads to lower fatty deposits in arteries
Recommended daily requirement of fiber = 20 to 30 grams of fiber per day met by eating: 5 servings of fresh or cooked fruit or vegetables 2 slices of whole wheat bread Peas and beans (legumes) – rich in protein, fiber, and virtually no fat Vitamins: may relate to cancer protection Beta carotene: contained in deep yellow and dark green vegetables: carrots, spinach, sweet potatoes, winter squash, and tomatoes Antioxidants: Vit C: oranges, grapefruit, strawberries, baked potatoes, and broccoli Vit E: vegetable oils, leafy greens, and whole grains Bone density: Vit D needed for absorption of calcium and phosphorus from the GI tract Vit D – fortified milk and sunlight Formation of red blood cells: Vit B 12 and folic acid Sources: lean meat, eggs, dairy products, breakfast cereals |
|
|
How do cholesterol and triglycerides influence health? ***
|
cholesterol: does not dissolve in blood, carried on lipoproteins
Total blood cholesterol includes the following: - LDL: low-density lipoprotein = bad cholesterol (deposits on vascular walls) - HDL: high-density lipoprotein = good cholesterol (prevents deposits, carries substances away from arteries and to liver) 1/3 to 1/4 of total cholesterol Triglycerides: form of fat made in body (from carbohydrates) - levels can generally be reduced with weight reduction, increased exercise, decreased alcohol intake L(p)a cholesterol: genetic variation of LDL. High levels associated with vascular disease |
|
|
How does aerobic exercise influence health? ***
|
regular aerobic exercise improves the body’s ability to utilize oxygen which is necessary to burn calories for the production of energy
aerobic exercise: target heart rate should be maintained for 20 to 30 minutes at least 3 times per week to attain aerobic benefits Target heart rate = 220 – your age x .70 (moderate intensity) 220 - your age x .90 = (high intensity) |
|
|
Reforms in the treatment of the mentally ill started after the French Revolution with an Austrian physician named:
|
Franz Mesmer
|
|
|
Psychiatric diagnoses are categorized in a book named the:
|
DSM
|
|
|
Which neurotransmitter is implicated in schizophrenia, depression, and ADHD?
|
dopamine
|
|
|
Which of the following regarding ADHD is false?
a. ADHD is limited to children b. ADHD is a neurobiological disorder c. ADHD is more common in males than in females d. There are three subtypes of ADHD |
a. ADHD is limited to children
|
|
|
Medications that replace ________ are effective in improving memory in persons with Alzheimer's disease.
|
acetylcholine
|
|
|
A false belief that one is being watched or punished is also known as a _______ delusion.
|
persecutory
|
|
|
Binge eating followed by purging behavior such as self-induced vomiting most commonly occurs in:
|
bulimia nervosa
|
|
|
Periods of intense mania and depression that last for several weeks is also known as _______.
|
bipolar I
|
|
|
Adults with bipolar illness may be treated with all of the following types of medications except _______.
a. sedatives b. antidepressant medications c. stimulant medications d. antipsychotic medications |
c. stimulant medications
|
|
|
Anxious, irrational thoughts and images are also called _______.
|
obsessions
|
|
|
Bones are soft in rickets due to a ____ deficiency.
|
Vitamin D
|
|
|
Osteomalacia affects (bones/joints) of young (children/adults).
|
bones of adults
|
|
|
Carpal tunnel syndrome is caused by damage to the _______.
|
median nerve
|
|
|
Biopsy in addition to electromyography is a diagnostic test for __________
|
Duchenne's MD
|
|
|
________ is the most common form of arthritis.
|
osteoarthritis
|
|
|
Ankylosis and immobility results in severe _______.
|
rheumatoid arthritis
|
|
|
Colchicine and corticosteroids are used to treat acute cases of _______.
|
gout
|
|
|
Which of these is NOT due to calcium deficiency?
a. osteoporosis b. osteomalacia c. osteogenic sarcoma d. rickets |
c. osteogenic sarcoma
|
|
|
Which of these is a type of autoimmune disorder?
a. rhabdomyosarcoma b. Duchenne's MD c. myasthenia gravis d. osteitis fibrosa cystica |
c. myasthenia gravis
|
|
|
Streptococci and staphylococci are associated with
a. Pott's disease b. tuberculosis c. osteomyelitis d. osteoporosis |
c. osteomyelitis
|
|
|
Bacterial infections on the skin may be caused by ________.
|
staphylococci
|
|
|
A discolored spot of the skin is a _________.
|
macule
|
|
|
A sac filled with a fluid or semifluid material is a _____.
|
cyst
|
|
|
The outermost layer of the skin is the ________.
|
epidermis
|
|
|
In pallor, the skin appears _______.
|
white
|
|
|
The ________ lies under the dermis and connects the skin to underlying structures.
|
subcutaneous tissue
|
|
|
Solid elevated areas of the skin are called ________.
|
papule
|
|
|
Folliculitis is an inflammation of _________.
|
hair follicles
|
|
|
Pediculosis is a ________ infection.
|
parasitic
|
|
|
________ is the oily fluid that is released through the hair follicles.
|
sebum
|

