![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
The Retail Medication order (medication order) |
The prescription |
|
|
|
medication order |
may be comunicated to the pharmacy by several means it may be presented by the patient or communicated by telephone fax or email.
Schedule 2 drugs are treated differently. |
|
|
|
Written Presciption order |
Precriptions are generally written on a form with preprinted required information. If the required information is not preprinted it may be wrtittern in or typed on the form. The prescription order must be completed in ink or typed to avoid possible alteration, and it must contain specific information when it is received in the pharmacy. If the perscription is incomplete or illegible it cannot be filled and the patient should be referred back to the prescriber or the the pharmacist. |
|
|
|
Required information to be written on the prescription order |
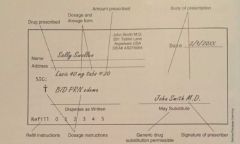
The upper portion:
The patients full name
The date of issue of the perscription
The name and title of the prescriber
The DEA number assigned to the prescriber
On the body:
The name of the drug prescribed
Strength and dosage form
Quantity of the drug to be dispensed
Instructions for dosage SIG
Instructions for Labeling
Signature of the prescriber
Authorization to dispense a generic substitution
Refill information
Instructions for the preperation of the drug |
|
|
|
The patients Full name |
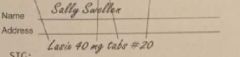
The is required for positive identification |
|
|
|
The date of issue of the prescription |
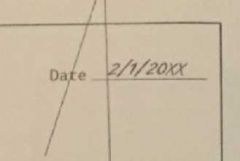
The date of writing helps to determine if the prescription may be filled. Prescriptions are valid only for one year after being written with the exception of prescriptions for controlled substances ( schedule 2 through 5), which are valide for six months or less. If the prescription is presented after the allotted time ( ie one year) the prescription cannot be filled. |
|
|
|
The name and title of the prescriber |
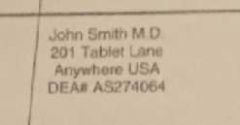
The prescriber may be a doctor of medicine MD, osteopathic medicine DO, optometry OD, dentistry DDS, veterinary medicine DVM, or podiatry. Other individuals liscensed to prescribe drugs include the physicians assitant and nurse practitioner. |
|
|
|
The Drug enforcement Agency prescriber number |
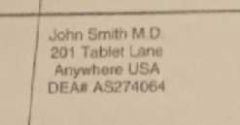
The Drug enforcement Agency DEA number assigned to the prescriber (required for controlled substances only): The DEA number is a seven digit number issued to the prescriber or institution by DEA. It should begin with two letters. The first letter, an A,B,F or M, designates the status of the prescriber. The second letter of the DEA number is the first letter of the prescribers last name. |
|
|
|
The name of the drug prescribed |
Can be generic or brand name |
|
|
|
Strength and dosage form |
|
|
|
|
Quantity of drug to be dispensed |
eg 20 tablets or 80 ml if the drug is to be administered in liquid form. |
|
|
|
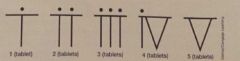
Instructions for dosage (SIG) |
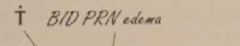
These should be clear and understandable. Dosage instructions on the prescription form are normally written in "medical shorthand" which the technician should be familiar with. For example numerical designation of the number of tablets, teaspoons, etc. are written in lowercase Roman numerals. |
|
|
|
instructions for labeling |
The prescriber may not want certain information on the prescription form to be shown on the label. In this case, instructions for what information is to be printed on the label are included. |
|
|
|
signature of the prescriber |
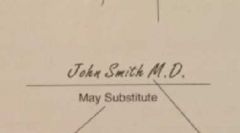
in ink no prestamped facsimiles are acceptable. |
|
|
|
Authorization to dispense a generic substitution |
The way in which a generic substitution is authorized or disallowed varies from state to state. Some states have an open box printed on the prescription form in which the prescriber writes DAW "dispense as written" or "Brand Medically Necessary" if the prescription is to be filled exactly as it is written. In other states, the prescription blank has two lines for signature and the line on which the prescriber signs designates how the prescription is to be filled. |
|
|
|
Refill information |
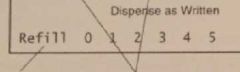
The number of refills should be clearly designated on the prescription form |
|
|
|
Instructions for the preperation of the drug |
This is rarely seen on a prescription form; however if a drug needs to be made a certain way, such as a cream, lotion, or suppository instead of a tablet, the prescriber may write out instructions for preperation of the drug. If specific written instructions exist for preperation of the drug, it may be prepared by the technician. |
|
|
|
Two letter method of DEA # verfication |
prescribers are assigned either a capital A, B, or F as the first letter of the DEA number. No particular signigicance is attached to the letter. Letters are simply assigned according to the date that the application for the DEA number was made. As more DEA numbers are assigned the letter designation will continue to move through the alphabet. Mid level practitioners are assigned with an "M" (physicians Assistant's, nurse practitioners) The second letter of the DEA number is the first letter of the prescribers last name. Thus it is easy to check the validity of the prescription: If the prescribers name is Smith, for example and the DEA number starts with AU it is invalide. It should be AS not AU, unless the practioner has gotten married and changed their last name since receiving a DEA number. |
|
|
|
Mathematical Verfication of the DEA # |
Step 1: First add the odd numbered digits ( the first, third, and fith numbers after the first two letters)
Step 2: Then add the even numbered digits ( the second, fourth, and sixth positions) and multiply by 2
Step 3: Add the two sums together
The last digit in the calculate sum should match the last digit in the DEA number. If these numbers do not match the DEA number is invalid and so is the prescription.
EXAMPLE:
DEA#: AU3284065
Step 1: 3+8+0 = 11
Step2: (2+4+6)(2)=24
Step 3: 11 + 24 = 35
The last number in the DEA number matches the last number of the two summed quantities. This number is valid based on the mathematical verfication.
|
|
|
|
Information to be added to the perscription form |
There is some infomation necessary for the pharmacy to have in order to protect the patient. This information should be obtained from the patient by the technician and written on the prescription form.
Prescriptions for Schedule II drugs, such as morphine (MSContin), meperidine (Demerol), or oxycodone (Roxicet), must have all information complete on the form before acceptance at the pharmacy window. |
|
|
|
Information that may be placed on the prescription form at the time of acceptance |
The patients address and telephone number
Age or date of birth
Allergies and concurrent medication
The insurance coverate of the patient |
|
|
|
Adress and Telephone Number |
This will help identify the patient and provide a contact in case of drug recall |
|
|
|
Age or Date of Birth |
This will assist in identification and assure an appropriate drug regimen. |
|
|
|
Allergies and concurrent medication |
This will prevent adverse reactions to medication |
|
|
|
The insurance coverage of the patient |
How does the patient intend to pay? Payment might be in the form of cash (Self-Pay) co pay ( the pharmacy bills the insurance company directly) or receipt for reimbursement. |
|
|
|
Authentication and Clarification of theprescription order |
In the event that the prescription form is unreadable or questionable, the technician should ask thepharmacist for clarification. Often the handwriting of the prescriber is illegible, or the signature orother information is questionable. In this case, the pharmacist will be aware of normal prescribedamounts for the drug in question and will be able to easily clarify the instructions and verify theprescription by telephone with the prescriber. This is especially important in the case of writtenprescriptions for Schedule II drugs, as they may be altered in order to obtain more drugs for abuse orsale. |
|
|
|
Accepting Refill Requests |
Refill requests for prescriptions other than Schedule II drugs may be made by the patient either overthe telephone, by fax, or in person. These requests my be accepted by the technician. After filling therefill prescription, the appropriate amount of drug is then deducted from the number of remainingprescription refills listed in the patient profile.Refills are normally spaced out over an appropriate amount of time however, they may be given all atone time ( at the discretion of the pharmacist) if the patient requests it. Sometimes when the drug istaken for a long period of time (eg antiseizure drugs and anxiolytics) it is less expensive for the patientto buy larger quantities at one time. Conversely the patient might not be able to afford the entirequantity of drug prescribed and may be allowed to purchase only part of the prescription at a time.Changes in the amount of drug dispensed are made at the discretion of the pharmacist as thepharmacist is legally responsible for everything that happens in the pharmacy.Controlled Substances such as Schedule II drugs, are treated in a very different way. Theseprescriptions may be filled by the technician, but any refills ( available on Schedules III-V drugs only)must be dispensed every 30 days. Five refills in six months are allowed on prescriptions for drugsclassified as Schedules III-IV. No refills may be dispensed on a prescription for Schedule II drug |
|
|
|
Refill Authorizations |
Sometimes a patient runs out of a needed medication and has not obtained a new prescription. In thiscase, the pharmacy may contact the physician/ prescriber to extend the original prescription. This iscalled the refill authorization and may be obtained only by a licensed pharmacy practitioner (e.g, thepharmacist or pharmacy intern). Some state now allow technicians to this also.Prescription refills may be accepted and filled by the technician. However, refill authorizations may betaken only by a licensed pharmacist or pharmacy intern. |
|
|
|
Prescriptions for Schedule II (controlledsubstance) Drugs |
A state may require a special prescription form for Schedule II drugs. In some states, this is a triplicateform, with the copies of the form serving as records for dispensing: one copy is sent to the DrugEnforcement Agency, one is sent to the prescriber, and one is filed in the pharmacy.As discussed previously, prescriptions for controlled substances must be filled exactly as prescribed.Again, no errors, corrections, or write-overs should be present on the form. If any corrections or extrawriting appears on the form when it is presented, the prescription should not be filled and it should bebrought to the attention of the pharmacist.Prescriptions for drugs classified as Schedule II must be complete when presented. No corrections oradditions are permitted. |
|
|
|
Receiving Prescriptions by Electronic Means |
Some states grant licensure to pharmacy interns. In this case, telephone prescriptions may also belegally taken by a licensed pharmacy intern. The technician may not take prescription orders formelectronic devices.Prescriptions received electronically must be transcribed onto a hard copy form before filling. Thismust be done by the pharmacist of pharmacy intern in most states.Prescriptions received electronically must be transcribed onto prescription form ( “ hard copy”) forpurposes of documentation. This may only be done by a licensed practitioner ie. The pharmacist. |
|
|
|
The institutional pharmacy |
pharmacies in hospitals |
|
|
|
The medication order and medication adminstration Record (MAR) |
The inpatient medication order is found only in a hosptial or instiutional pharmacy and serves as the drug order. It is very detailed much more so than a retail prescription. From the medication order, Medication Administration Record MAR is generated. |
|
|
|
What goes on the medication order |
The list of medications ordered for the patient includes a shedule for the administration (MAR) of the drugs, and if necessary instructions for preperation of the drugs. By looking at the dosage schedyle and the age height weight medical history diet and diagnosis of the patient, the pharmacist can determine whether the patient is receiving the appropriate drug and dose for the diagnosis and also that the drug is compatible iwht the patients diet and will not adversly affect existing condition that the patient may have. |
|
|
|
Medication orders must specify |
The exact dosage form of the drug ( ie solution, suspension, tincture, etc. instead of just "liquid".
The dosage strength
Direction for use, where appropriate
Information regarding the patient and the patients meidcal condition
route of administration Instructions for preperation
|
|
|
|
The dosage form |
The dosage form ordered should be appropriate tothe patients medical consition; a vomitting patient would not be prescribed an oral medication, for example, but would receive the medication as suppository form or by injections. If there is only one dosage form or strength of the prescribed medication it is not specified.
The drug dosage form must be clearly specified and must be appropriate to the patients medical condition. If only one dosage form exists specification of dosage form is not required. |
|
|
|
information regarding the patient and the patients medical condition |
information regarding the patient and the patients medical condition allows the pharmacist to verify the drugs prescribed and dosage schedule are appropriate. |
|
|
|
route of administration |
In the hosptital setting, the route of administration of the drug must be specified (eg an order of morphine gr 1/4 could be given orally, intravenously or intramuscularly). This assists the technician in preparing the drug for administration. |
|
|
|
intructions of preperation of the drug |
Often pateint medications must be prepared for injection in a certin way. The medication order may contain instructions for the proper dilution of a drug and the diluent ( the liquid that the durg is to be dissolved in) to be used. These should be transcribe onto the MAR. |
|
|
|
Total Parenteral Nutrition Solutons (TPN's) |
Frequently a patient who undernourished, vomitting or has severe diarrhea may require intravenous feeding, and total parenteral nutrition solutions (TPN's) may be ordered. These medications contain a balanced mixture off sugars proteins and fats to be adminstered intravenously. The exact mixture depends on the patients needs, so instructions for compounding ( how to make the solution) are also stamped or written on the medication order. The hospital order includes information such as Drugs to be administered doses and routes of administration and reason for use Date of drug order The date that the therapy is started and the date that it is to be discontinued The prescribers name for each drug Designation of drugs for which generic substitutions are allowed/ disallowed Drug dosages and schedule for administration Dosage instructions Instructions for compounding medications. |
|
|
|
Generation and organization of the medication administration record MAR |
The medication administration record (MAR) is generated by the pharmacy and serves as a record ofmedication administration by nursing staff. It contains a list of the drugs dispensed from the pharmacy,the time of dispensing, and the initials of the person dispensing the medication, as well as dosages andtimes of administration.Instead of giving a set of dosage instructions with each drug (the SIG), the MAR puts the medicationorder within a specific dosage schedule. This schedule tells when the medications are to be given tothe patient and is normally determined by the institution. Most hospitals have set times when “routine”medication is delivered, in order to decrease confusion and minimize the possibility of dosage errors.The dosage ScheduleDrug dosages have to be scheduled relative to each other, and medications are usually administeredaccording to the hospital work shift or during preset medication administration times for the hospital.Therefore, the MAR usually contains a dosage schedule for drug administration. For example the timesof administration may be listed across the top of the MAR according to a 24 hour clock. The nurseadministering the medication may place a mark in the block underneath the time that the medicationwas administered to the patient. Next to the time of administration, there may be black spaces for thepharmacy technician to note the time that the drug was dispensed and his pharmacy technician to notethe time that the drug was dispensed and his or her initials. The nurse also initials as to the actual timeof administration. In this way an accurate record is kept of when the drug was dispensed and how longthe drug was stored before it was given. The MAR also serves as a record that the drug actually wasadministered, by whom, and the actual time of administration (this is particularly important withnarcotic drugs).The MAR also serves as documentation of the drugs actually administered to the patient, whichfacilitates accurate patient billing.In a hospital setting, the patient receives several drugs at one time, so dosages must be scheduledrelative to each other to avoid medication errors. |
|
|
|
Filling the medication order |
In a hospital setting, the medication order (Physicians order) is transmitted to the pharmacy, eitherdirectly or by computer. Computerized transmission is preferable, as it decreases the probability oftranscription errors. Once in the pharmacy, it is the responsibility of the pharmacist to review the orderand evaluate the suitability of the drugs prescribed, with regard to the patient and his or her existingdrug and dosage regimen. Once reviewed, the order is passed to the technician for filling. Thetechnician the fills the order. A technician or the nurse then transcribes the information onto the MAR.Rather than filling an order for an individual drug and sending it up to the floor at the appropriate timefor administration, the unit dose system is used. |
|
|
|
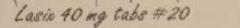
The unit Dose |
A unit dose is defined to be the amount of drug needed for a single dose. The dose of drug iscalculated, the order is filled with the drug stock available in the pharmacy, and th drug packaged as anindividual (unit) dose.Example: An order is for 80 mg tablets of Lasix po bid. The pharmacy only has 40 mg tablets in stock.A unit dose would be the amount of the drug needed for a single does, so two of the 40 mg tabletswould be packaged together. |
|
|
|
The unit dose system |
In the unit dose system, all of the drug doses for an individual patient that will be required for entireday are prepared at one time and distributed to the patient floors.The individual drugs are read off the medication order, with dosage strength, form, and instructions.The technician is responsible for assessing the instructions for dosage of the drug (eg one tablet bid, qidetc.) and calculating the amount of drug ( the number of tablets, number of milliliters, etc.) that will begiven to the patient in the course of one day. The technician then prepares the proper amount and placesit in a properly labeled container (cassette/drawer) for insertion into the medication cart.Proper labeling of the cassette should include The patients name The hospital identification number The attending physicians name The location of the patient (e.g, room 222, bed 1) |
|
|
|
the medication cart |
Modern pharmacies now use medication carts, which are located on the individual patient floors. Thesecarts are free-standing, computerized cabinets containing the daily medications for all patients on aparticular floor or wing within a hospital or nursing home. The technician delivers the unit dose cassettes to the patient floor and files the medication within the drawers of the medication cart, so thatenough drugs for a particular patient is sent up for entire day at one time. Normally, the drugs for anindividual patient are filed by patient identification number. Unused medication, if the package has notbeen opened, may be returned to the pharmacy for restocking and patient credit (i.e., medicationsintended for dosing “as needed” for example, and are not used, or medication assigned to a dischargedpatient). |
|
|
|
Comparison of Medication orders in retail andinstitutional Settings |
The two types of medication order discussed in this chapter have many things in common: the name ofthe patient and other identifying information, the prescriber's name and title, and drugs prescribed. Themajor difference is the amount of detail presented.The institutional medication order gives a detailed schedule of administration. The retail order givesonly instructions to be followed by the patient, because the medication is self-administered. There ismore identifying information present on the institutional medication order as well, to ensure that themedication is administered to the right patient.The amount of information included on the order differs also. This information may include diagnosis,laboratory tests, height and weight, and other information about the patient as well. |
|
|
|
Prescription of Controlled Substances |
In an institutional setting, the prescription of controlled substances does not require a special form; theyare just included on the order. Since prescriber may use the DEA number assigned to the hospital, thereare no prescriber DEA numbers on the order (which may also have several different prescriber's)Delivery of the controlled substances to the hospital floor or unit may require special documentation,however, including signatures of the technician delivering the medication and th head nurse in thepatient care area, documenting transfer of the drug ( and responsibility for the drug) from the pharmacyto the patient care area.In a retail setting, a prescription for a controlled substance (specifically a Schedule II drug, such asmorphine or Demerol) requires triplicate form in many states, which must be filed separately from theother prescription forms, with copies sent to the prescriber and the DEA. |
|

