![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
Myths about Schizophrenia
|
- People with schizophrenia are Dangerous
- People with schizophrenia have Split Personalities |
|
|
Prevalence
|
- Approx. 1% of population suffers from schizophrenia
- Peak Age: Men 15 - 25 years, Women 25 - 35 years - Rare onset at < 10 years or > 50 years - Men are 30 - 40% More likely to develop schizophrenia - Approx. 50 % of all schizophrenics attempt Suicide - All cultures & SES groups - Most Schizophrenics born in winter months - Most expensive mental disorder (treatment, loss of productivity and public assistance costs) (Prevalence) |
|
|
Schizophrenia DSM-IV Criteria
|
A. Characteristic Symptoms
B. Social Occupational Dysfunction C. Duration D. Schizoaffective & Mood Disorder Exclusion E. Substance/General Medical Condition Exclusion F. Relationship to a Pervasive Developmental Disorder (Schizophrenia DSM-IV Criteria) |
|
|
Characteristic Symptoms
|
At least 2 of the following each present for a significant portion of time during a 1 month period:
- Delusions - Hallucinations - Disorganised Speech - Grossly Disorganised or Catatonic Behaviour - Negative Symptoms (Affect flattening, Alogia, Avolition) (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Duration of Schizophrenia
|
Continuous Signs for 6 Months
(Schizophrenia DSM-IV Criteria, Duration) |
|
|
Delusion
|
Disturbance in content of thought. False belief, based on incorrect inference about external reality, not consistent with patients intelligence & cultural background, that cannot be correct by reasoning.
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Delusion
|
- Delusions of Persecution (others are out to get you)
- Delusions of Reference (irrelevant or unrelated phenomena have refer directly to them/have special personal significance) - Delusions of Grandeur (unrealistic beliefs about the self) (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Disorganised Speech
|
Disturbance in Form of Thought. Disturbances in production & organisation of thought, revealed by peculiarities of verbal expression
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Disorganised Speech
|
- Neologism (creating words)
- Perseveration (persevering topics/memories) - Word Salad (incoherent jumble of words) - Circumstantiality (drifts away from topic, but comes back to the point) - Tangentiality (drifts away from topic, and doesn't return to the point) (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Hallucinations
|
Disturbance of Perception. False sensory perception not associated with external stimuli
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Hallucinations
|
- Auditory
- Visual - Olfactory - Gustatory - Tactile (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Affect
|
Disturbances in Affect. The expression of emotion as observed by others
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Affect
|
- Restricted Affect
- Blunted Affect - Flat Affect (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Catatonia
|
Disturbance in Psychomotor Behaviour. Abnormality of movement and behavior arising from a disturbed mental state
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Catatonia
|
- Catatonic Stupor (near non-existent motor activity)
- Catatonic Rigidity (rigid limbs that instantly return to original position) (Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Positive Symptoms
|
Excess behaviours such as: Delusions, Hallucinations, Loose Associations, Disorganised Behaviour
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Negative Symptoms
|
Deficits such as: Flat affect, Apathy, Social withdrawal, Poor attention
(Schizophrenia DSM-IV Criteria, Characteristic Symptoms) |
|
|
Types of Schizophrenic Disorders
|
- Disorganised type
- Catatonic type - Paranoid type - Undifferentiated type - Residual type (Types of Schizophrenic Disorders) |
|
|
Disorganised Schizophrenia
|
Disorganised Speech, disorganised Behaviour & Flat or Inappropriate Affect
(Types of Schizophrenic Disorders) |
|
|
Catatonic Schizophrenia
|
Marked psychomotor disturbance which may involve stupor, rigidity, excitement or posturing
(Types of Schizophrenic Disorders) |
|
|
Paranoid Type
|
Preoccupation with one or more delusions or frequent auditory hallucinations related to a single theme
(Types of Schizophrenic Disorders) |
|
|
Undifferentiated Schizophrenia
|
People diagnosed as schizophrenic who don't fall neatly into one category
(Types of Schizophrenic Disorders) |
|
|
Residual Schizophrenia
|
When psychotic symptoms of schizophrenia lessen in intensity & number, yet remain in a residual form
(Types of Schizophrenic Disorders) |
|
|
Type I Schizophrenia
|
- Sudden onset
- Normal intellect - No brain damage - No negative symptoms - Good drug response (Type I & Type II Schizophrenia) |
|
|
Type II Schizophrenia
|
- Slower onset
- Intellectual deterioration - Brain abnormality - Prominent negative symptoms - Poor drug response (Type I & Type II Schizophrenia) |
|
|
Course of Schizophrenia
|
- Prodromal phase (an early symptom)
- Active phase - Residual phase - Typically the disorder is episodic |
|
|
Prognosis of Schizophrenia
|
- 20 - 30% are able to lead normal lives
- Approx. 20 - 30% experience moderate symptoms - Approx. 40 - 60% remain significantly impaired |
|
|
Good Outcome Predictors for Schizophrenia
|
- Good Premorbid adjustment
- No family history of schizophrenia - Sudden onset - Precipitating Stress - Good response to medication - Positive Symptoms - Later Age of onset - Female Gender (Outcome Predictors for Schizophrenia) |
|
|
Poor Outcome Predictors for Schizophrenia
|
- Poor premorbid adjustment
- Family history of schizophrenia - Slow onset - No precipitating stress - Poor response to medication - Negative Symptoms - Early age of onset - Male Gender (Outcome Predictors for Schizophrenia) |
|
|
Other Psychotic Disorders
|
- Schizophreniform Disorder
- Schizoaffective Disorder - Delusional Disorder - Brief Psychotic Disorder - Shared Psychotic Disorder - Psychotic Disorder due to General Medical Condition - Substance-Induce Psychotic Disorder (Other Psychotic Disorders) |
|
|
Schizophreniform Disorder
|
- Duration at least 1 month but less than 6 months
- Impaired social/occupational functioning not required (Other Psychotic Disorders) |
|
|
Schizoaffective Disorder
|
- Symptoms fall on the boundary between schizophrenia and mood disorders
- Prominent episode of mood disturbance concurrent with Criterion A schizophrenia symptoms - Delusions/hallucinations for at least 2 weeks in absence of prominent mood disturbance (Other Psychotic Disorders) |
|
|
Delusional Disorder
|
One or more delusions & never met criterion A schizophrenia
(Other Psychotic Disorders) |
|
|
Brief Psychotic Disorder
|
- Sudden onset of at least 1: delusions, hallucinations, disorganised speech, disorganised/catatonic behaviour
- Lasts at least 1 day but less than a month & full return to premorbid functioning (Other Psychotic Disorders) |
|
|
Biological Aetiology of Schizophrenia
|
- Genetics: Schizophrenia is a heterogeneous disorder & therefore unlikely to trace aetiology to a single gene
- Biochemical: Dopamine Hypothesis (decrease dopamine to decrease schizophrenic symptoms) - Abnormal Brain Structure: Enlarged ventricles especially on the left side (Biological Aetiology) |
|
|
Problems with Dopamine Hypothesis
|
- Many of the drugs used to treat schizophrenia are effective in treating other disorders
- Clozapine (recent drug) primarily blocks serotonin (Biological Aetiology) |
|
|
Behavioural Aetiology of Schizophrenia
|
- Failure to attend to relevant social cues result in bizarre responses to environment
- These bizarre responses/behaviours become learned and reinforced (operant conditioning) - Yet it is unable to fully account for the origins of the various symptoms of schizophrenia (Psychosocial Factors) |
|
|
Family Views Aetiology of Schizophrenia
|
- Schizoprenogenic Mother
- Double-bind Communication - Family structure - Communication deviance - Expressed Emotion (Psychosocial Factors) |
|
|
Expressed Emotion
|
- Stressors may precipitate relapses
- Family stress = expressed emotion (criticism, hostility, emotional over-involvement) - Person with schizophrenia is 3.7 times more likely to relapse if living in a High EE family than a Low EE family (Psychosocial Factors) |
|
|
Family Burden Studies
|
- Patient's problem behaviours (negative symptoms)
- Families reaction (emotional reactions, family conflicts) - Needs of families (information on the illness, practical guidance in patient management, community resources) - Burden of Blame (being ignored, used only as a source of information, Blamed for causing/exacerbating the illness) - Reciprocal transaction between patient & family (Psychosocial Factors) |
|
|
Limitations of Family Views
|
- Earlier views were not based on empirical evidence
- Many of the findings were correlational - These family patterns also occur in families of patients with other disorders - Reciprocal relationship between patient & family members not taken into account - The impact of living with a family member with schizophrenia neglected (Psychosocial Factors) |
|
|
Diathesis-Stress Model of Schizophrenia
|
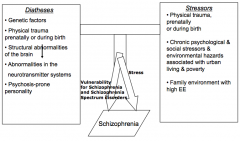
Diathesis-Stress Model of Schizophrenia
|
|
|
Treatment
|
- Psychosocial Interventions (CBT, Rehabilitation, Family interventions)
- Somatic Treatments (Anti-psychotics) - Multifaceted Treatment Approaches - Community Approach (Deinstitutionalisation) - Effective Community Care - Developing countries have better recovery rates for schizophrenia than developed countries |
|
|
Cognitive Behavioural Therapy (CBT)
|
- Psychoeducation
- Social Skills Training - Coping Strategies Enhancement Training (Problem solving, Strategies for maximising medication compliance, Identification of relapse warning signals, Stress management strategies) (Psychosocial Interventions) |
|
|
Family Interventions
|
Supplementing drug treatment with either individual social skills training or family intervention reduces relapse
(Psychosocial Interventions) |
|
|
Anti-Psychotics
|
- Positive symptoms respond better than negative symptoms
- A substantial minority of patients, perhaps 25% do not improve on classical antipsychotic drugs - Unwanted effects/side effects (Somatic Treatments) |
|
|
Effective Community Care
|
- Coordinated Services
- Short-term hospitalisation - Partial hospitalisation - Community houses/half-way houses - Advocacy (Treatment) |

